A comprehensive examination of the eyes and their functions is important for all individuals with ocular symptoms, and to screen for visual acuity, glaucoma Glaucoma Glaucoma is an optic neuropathy characterized by typical visual field defects and optic nerve atrophy seen as optic disc cupping on examination. The acute form of glaucoma is a medical emergency. Glaucoma is often, but not always, caused by increased intraocular pressure (IOP). Glaucoma, and retinal pathology. A routine examination includes testing for visual acuity, peripheral vision, and color vision, plus an examination of the external eye, conjunctiva Conjunctiva The mucous membrane that covers the posterior surface of the eyelids and the anterior pericorneal surface of the eyeball. Eye: Anatomy, sclera Sclera The white, opaque, fibrous, outer tunic of the eyeball, covering it entirely excepting the segment covered anteriorly by the cornea. It is essentially avascular but contains apertures for vessels, lymphatics, and nerves. Eye: Anatomy, iris, pupil Pupil The pupil is the space within the eye that permits light to project onto the retina. Anatomically located in front of the lens, the pupil's size is controlled by the surrounding iris. The pupil provides insight into the function of the central and autonomic nervous systems. Pupil: Physiology and Abnormalities, and extraocular movements. Primary care clinicians evaluate and refer for visual acuity issues, and treat minor eye conditions such as infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, hordeola (styes), and corneal abrasions Abrasions Corneal Abrasions, Erosion, and Ulcers. Slit-lamp exams are performed by eye specialists or emergency providers to examine the cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy, anterior chamber Anterior chamber The space in the eye, filled with aqueous humor, bounded anteriorly by the cornea and a small portion of the sclera and posteriorly by a small portion of the ciliary body, the iris, and that part of the crystalline lens which presents through the pupil. Eye: Anatomy, lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy, and fundus Fundus The superior portion of the body of the stomach above the level of the cardiac notch. Stomach: Anatomy. Dilated exams help examine the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy. Annual examinations are recommended for individuals with diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus for early detection and treatment of retinopathy Retinopathy Degenerative changes to the retina due to hypertension. Alport Syndrome.
Last updated: May 17, 2024
Recommended frequency of eye exams is not standard, but in general:
A dilated exam helps diagnose:
The eye and its appendages are situated in the orbit. The eyeball is spheroidal and attached to the extraocular muscles.
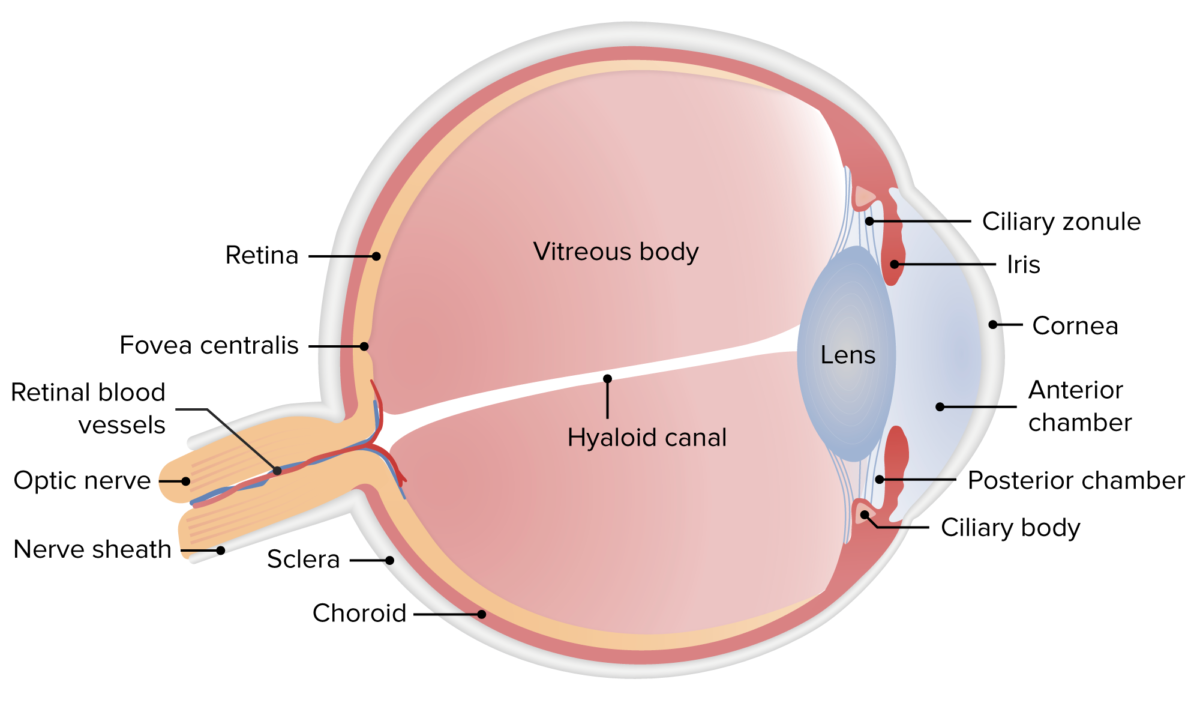
Anatomy of the human eye
Image by Lecturio.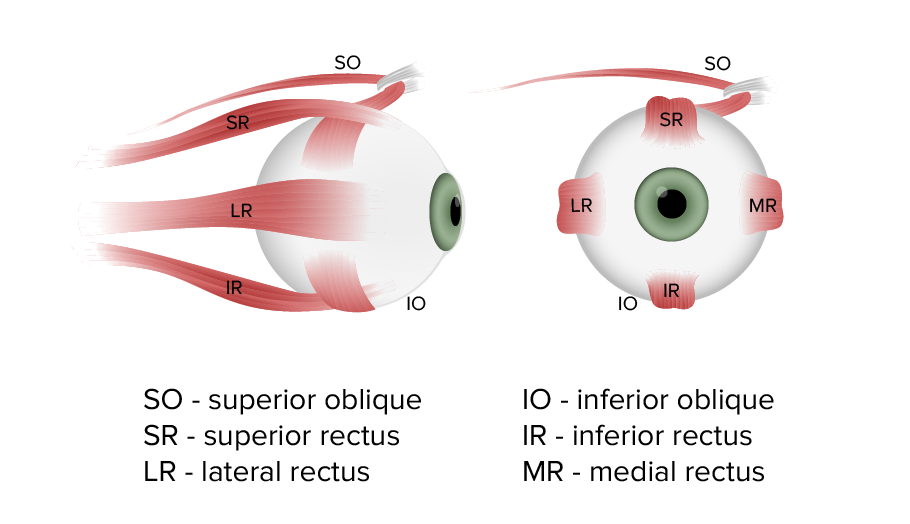
Extraocular muscles involved in controlling the movements of the eye
Image by Lecturio.
Portable slit lamp used for examination of the cornea
Image: “Portable slit lamp” by University of California, Irvine School of Medicine, Emergency Department, Irvine, California. License: CC BY 4.0
Handheld ophthalmoscope (and otoscope)
Image: “Ophthalmoscope and otoscope combination by Welch Allyn” by James Heilman, MD. License: Public DomainSnellen chart:
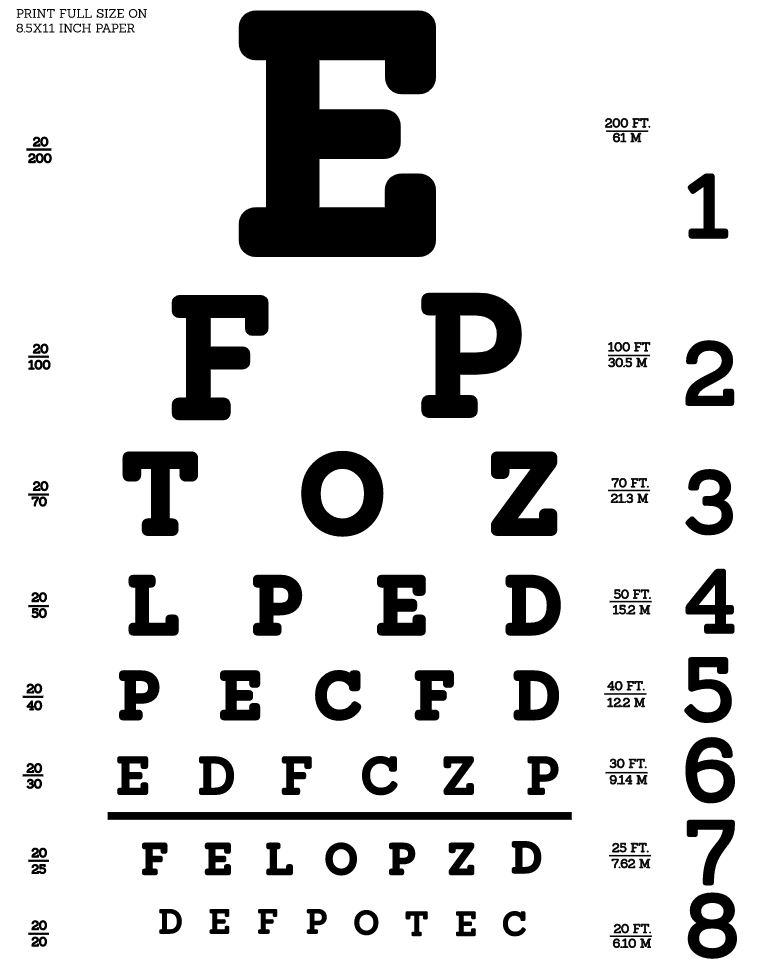
Snellen eye chart: used to test visual acuity
Image: “Snellen chart by Openclipart” by Openclipart. License: CC0 1.0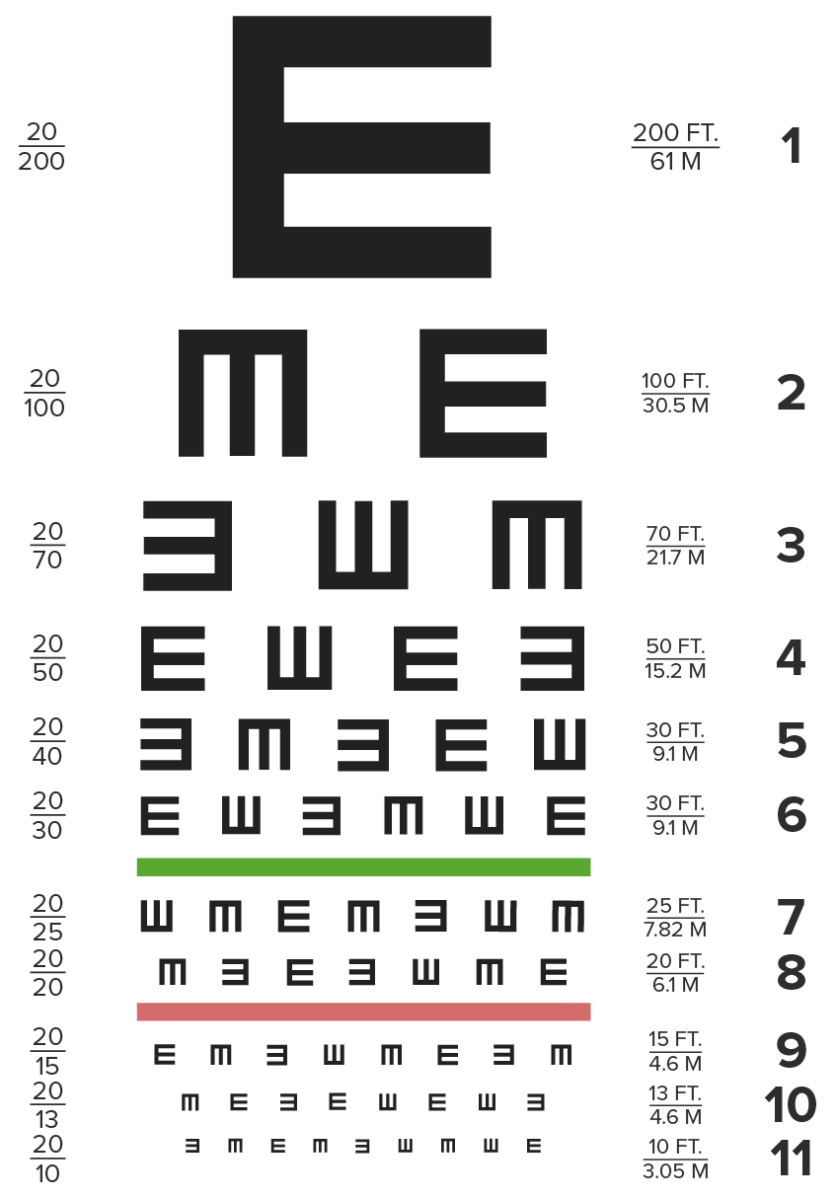
Tumbling E eye chart
Image by Lecturio.Near-vision chart:
Clinical relevance:
The field of vision is the total area in which objects can be visualized while looking straight ahead; it includes central vision and peripheral vision.

Testing visual fields:
The examiner’s left eye is closed, so he can compare the field of his right eye with the field of the subject’s left eye.
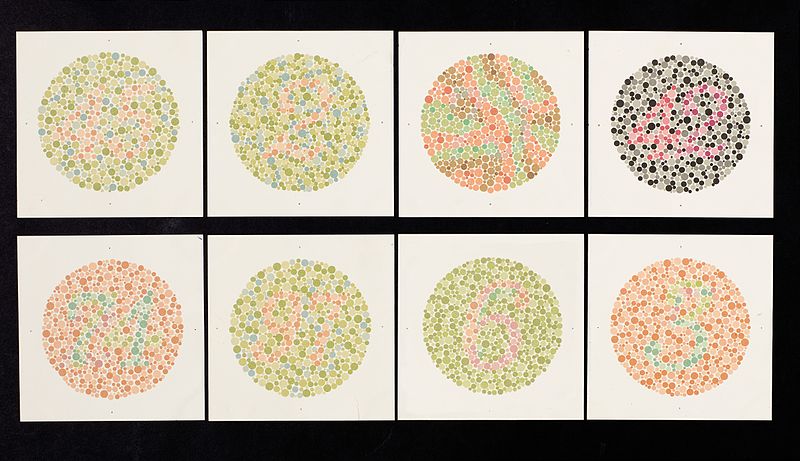
Ishihara chart used for examining color vision
Image: “Ishihara chart” by Wellcome Trust. License: CC BY 4.0Preliminary examination for any gross anomalies in the eye and the surrounding structures is conducted in diffuse light. The clinically relevant findings are:
Eyebrow:
Eyelids Eyelids Each of the upper and lower folds of skin which cover the eye when closed. Blepharitis:

Papillae on the everted upper eyelid in vernal keratoconjunctivitis
Image: “Papillae on the everted upper eyelid in vernal keraconjunctivitis” by Millicent Bore. License: CC BY 2.0Examination:
Clinical relevance:
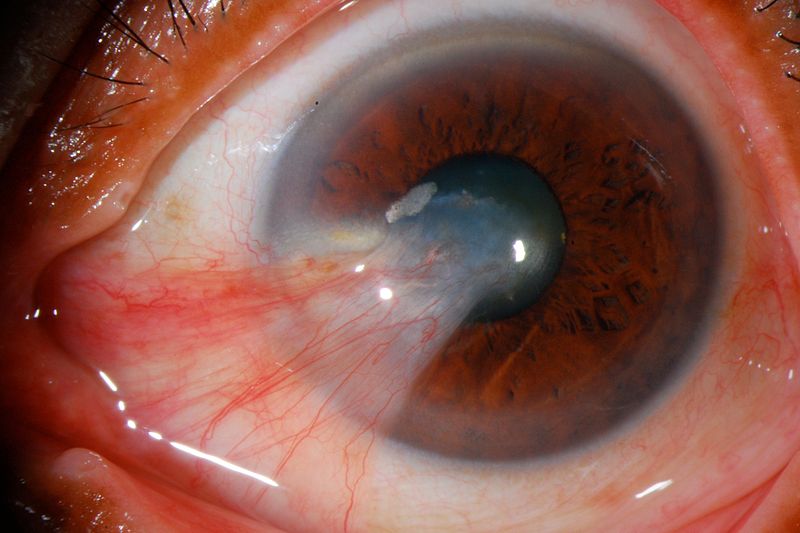
Severe pterygium reaching the pupil
Image: “Pterygium” by José Miguel Varas, MD. License: CC BY 3.0
Child with retinoblastoma of the right eye presenting with leukocoria
Image: “Pathology: Patient: Retinoblastoma” by National Cancer Institute. License: Public DomainThe cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy is examined with a slit lamp or after corneal staining.
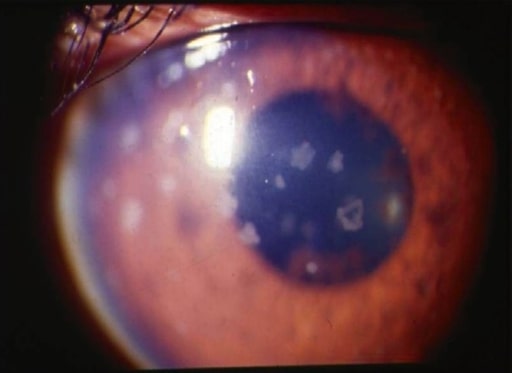
Anterior uveitis: slit-lamp photograph showing large, old keratic precipitates
Image: “Anterior uveitis” by L. V. Prasad Eye Institute, Kallam Anji Reddy Campus, Hyderabad, India. License: CC BY 2.0Examination of the lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy is done using a slit lamp after fully dilating the pupils.

Tonometer used for measuring intraocular pressure
Image: “Tonometer” by University of California, Irvine School of Medicine, Emergency Department, Irvine, California. License: CC BY 4.0Examination of the fundus Fundus The superior portion of the body of the stomach above the level of the cardiac notch. Stomach: Anatomy is important to diagnose disorders of the vitreous humor Humor Defense Mechanisms, optic nerve Optic nerve The 2nd cranial nerve which conveys visual information from the retina to the brain. The nerve carries the axons of the retinal ganglion cells which sort at the optic chiasm and continue via the optic tracts to the brain. The largest projection is to the lateral geniculate nuclei; other targets include the superior colliculi and the suprachiasmatic nuclei. Though known as the second cranial nerve, it is considered part of the central nervous system. The 12 Cranial Nerves: Overview and Functions, choroid Choroid The thin, highly vascular membrane covering most of the posterior of the eye between the retina and sclera. Eye: Anatomy, and retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy.
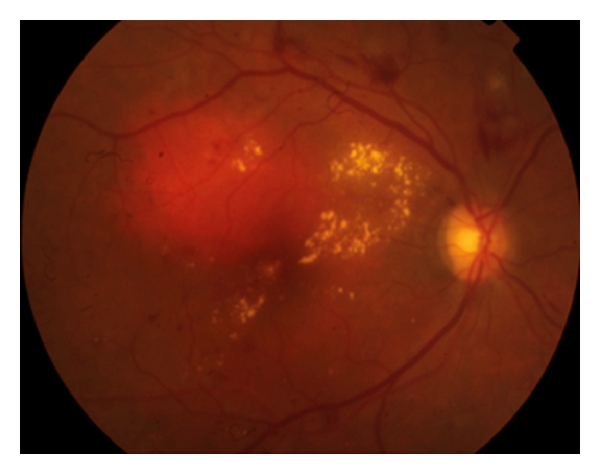
Diabetic retinopathy showing intraretinal hemorrhages, hard exudates, and microaneurysms in the posterior pole associated with diabetic macular edema
Image: “Diabetic retinopathy” by Francisco Rosa Stefanini et al. License: CC BY 3.0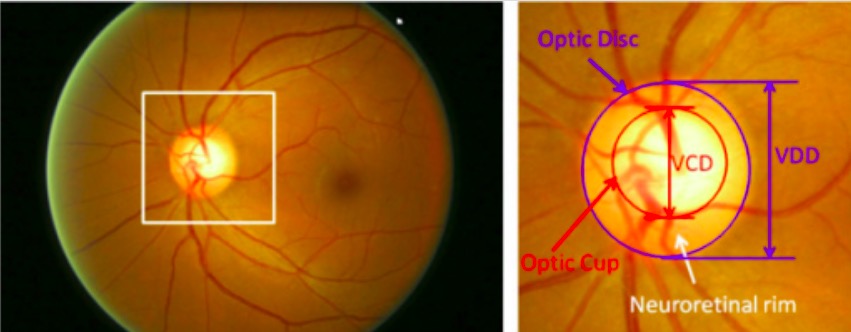
Major structures of the optic disc:
The region enclosed by the blue line is the optic disc; the central bright zone enclosed by the red line is the optic cup.
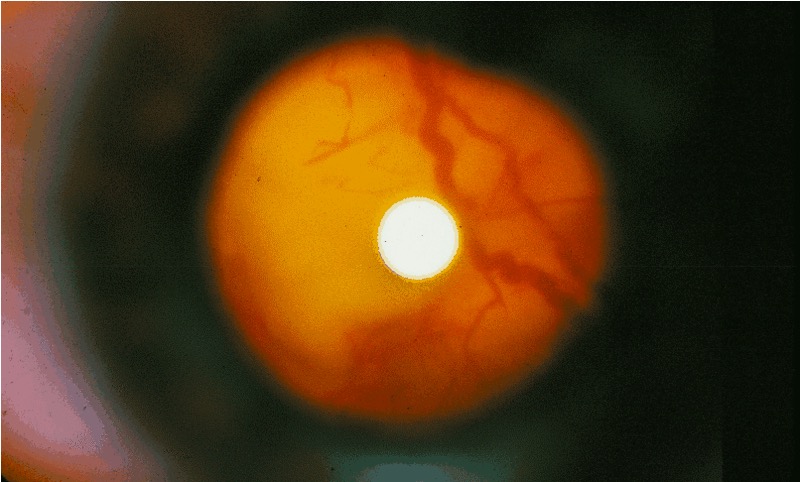
Photo of the fundus in an individual with tuberous sclerosis:
Ophthalmoscopic examination showing a large tumor extending from the right side of the optic nerve head