Fibromuscular dysplasia (FMD) is a nonatherosclerotic, noninflammatory, medium-sized angiopathy due to fibroplasia of the vessel wall. The condition leads to complications related to arterial stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms, or dissection. The clinical presentation can differ depending on which arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology are affected, but may include secondary hypertension Secondary hypertension Hypertension from renal artery Renal artery A branch of the abdominal aorta which supplies the kidneys, adrenal glands and ureters. Glomerular Filtration stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) ( RAS RAS Renal artery stenosis (RAS) is the narrowing of one or both renal arteries, usually caused by atherosclerotic disease or by fibromuscular dysplasia. If the stenosis is severe enough, the stenosis causes decreased renal blood flow, which activates the renin-angiotensin-aldosterone system (RAAS) and leads to renovascular hypertension (RVH). Renal Artery Stenosis), neurologic deficits Neurologic Deficits High-Risk Headaches from cerebrovascular involvement, claudication due to limb involvement, and intestinal angina Intestinal Angina Mesenteric Ischemia from mesenteric artery disease. The diagnosis is confirmed with imaging, such as computed tomography with angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery. Treatment includes lifestyle modifications, antihypertensive therapy for RAS RAS Renal artery stenosis (RAS) is the narrowing of one or both renal arteries, usually caused by atherosclerotic disease or by fibromuscular dysplasia. If the stenosis is severe enough, the stenosis causes decreased renal blood flow, which activates the renin-angiotensin-aldosterone system (RAAS) and leads to renovascular hypertension (RVH). Renal Artery Stenosis patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, and potential revascularization Revascularization Thromboangiitis Obliterans (Buerger Disease).
Last updated: Jan 17, 2024
Fibromuscular dysplasia (FMD) is a noninflammatory, nonatherosclerotic angiopathy characterized by stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms, dissection, and tortuosity of medium-sized arteries Medium-Sized Arteries Kawasaki Disease.
Fibromuscular dysplasia primarily affects the renal (most common), carotid, visceral, external iliac, and vertebral arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology.
The cause of this disease is unknown.

Diagram showing fibroplasia of the tunic media, which can result in narrowing of the arterial lumen: Aneurysms may form as well, with thinning of the vessel wall.
Image by Lecturio.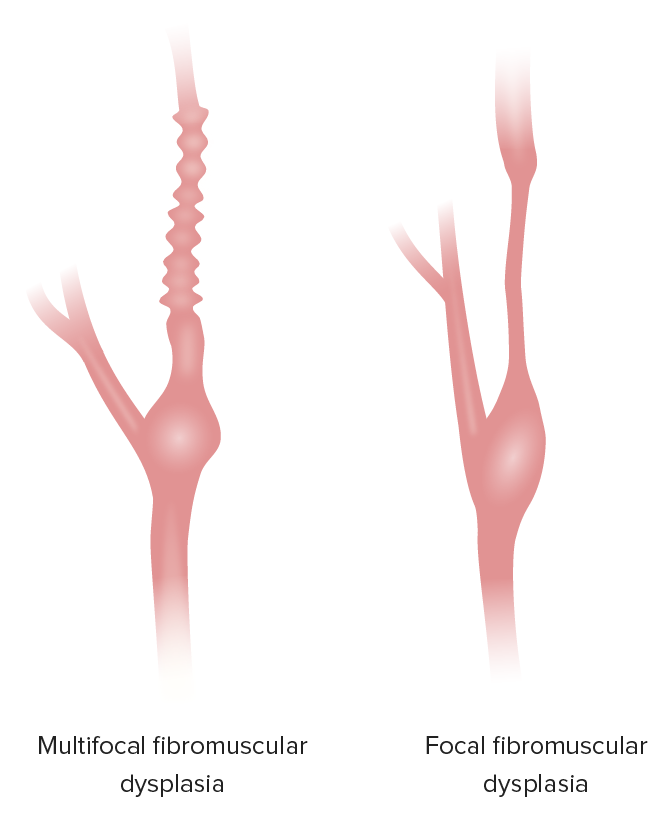
Representations of multifocal FMD and focal FMD
Image by Lecturio.The clinical presentation depends on the affected vessels and the degree of blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure disruption. Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are asymptomatic.
Imaging is used to confirm the diagnosis.
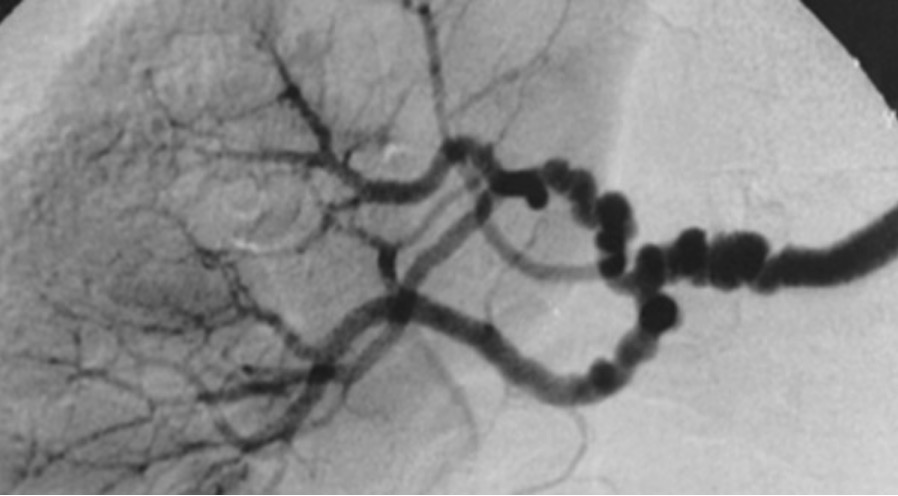
Angiography image showing the “string of beads” appearance of branches of the renal artery in a patient with multifocal fibromuscular dysplasia
Image: “String-of-beads” by Hôpital Européen Georges Pompidou, AP-HP, Université Paris Descartes, Faculté de Médecine, INSERM Unit 772, Collège de France, Paris, France. License: CC BY 2.0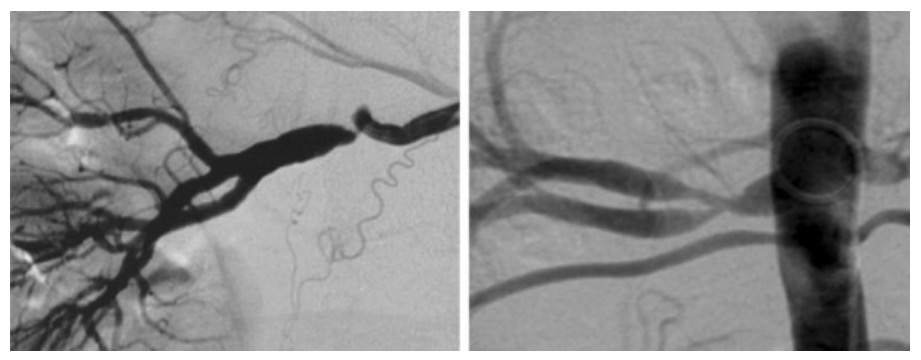
Circumferential (left) and tubular (right) stenosis seen in focal fibromuscular dysplasia on angiography
Image: “Unifocal (left) and tubular (right) stenoses” by Plouin et al; licensee BioMed Central Ltd. License: CC BY 2.0