The abdominal examination is the portion of the physical exam evaluating the abdomen for signs of disease. The abdominal examination consists of inspection Inspection Dermatologic Examination, auscultation, percussion Percussion Act of striking a part with short, sharp blows as an aid in diagnosing the condition beneath the sound obtained. Pulmonary Examination, and palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination. Along with information from the history, the information gathered from the physical examination of the abdomen is used by the physician to generate a differential diagnosis and treatment plan for the patient.
Last updated: Feb 16, 2023
1st steps:
The components of the abdominal exam:
In a different order (auscultation before percussion Percussion Act of striking a part with short, sharp blows as an aid in diagnosing the condition beneath the sound obtained. Pulmonary Examination), the same elements make up the other physical exam sections but carry different degrees of importance.
Pelvic, genital, and rectal exams should supplement the abdominal exam for a complete diagnostic workup of abdominal pathology.
Anatomy:
The abdomen is divided into 4 quadrants: right upper, right lower, left upper, and left lower. The quadrants correspond to specific organs and structures.
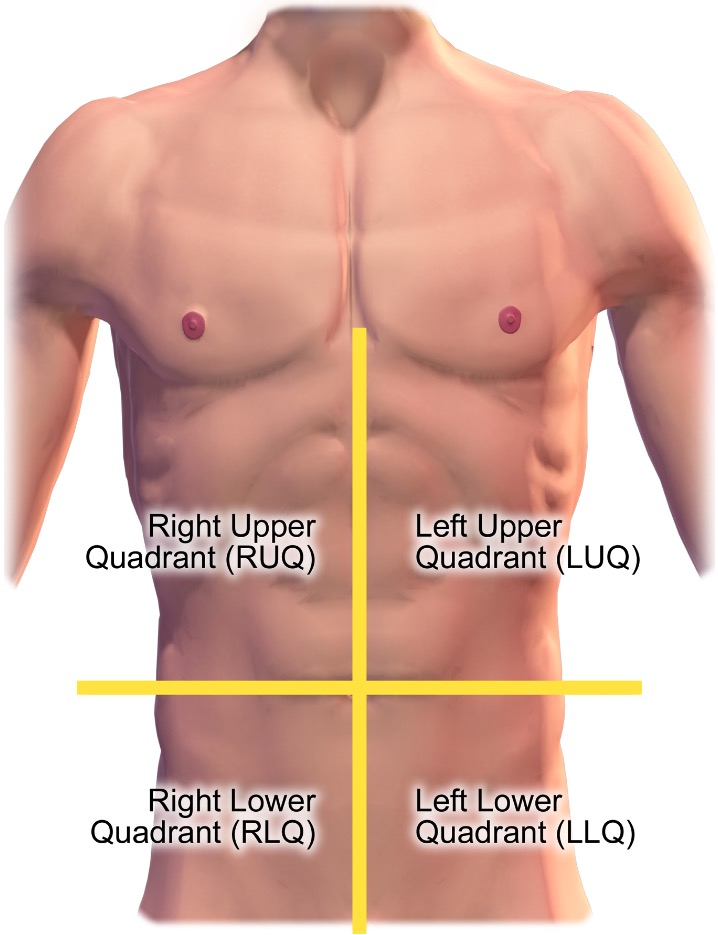
Quadrants of the abdomen
Image: “Quadrants of the abdomen” by BruceBlaus. License: CC BY 3.0, cropped by Lecturio.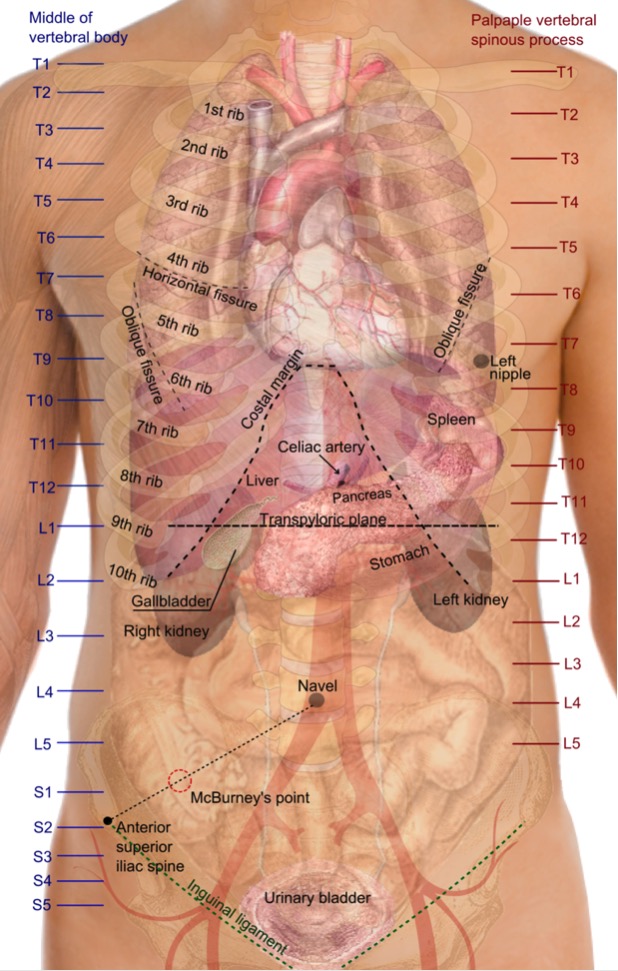
Surface projections of the organs of the trunk: Organ locations are derived mainly from vertebra levels, ribs, and the ilium.
Image: “Surface projections of the organs of the trunk” by Mikael Häggström. License: Public Domain
Caput medusae in portal hypertension
Image: “Dilatation of abdominal collateral veins” by Chen M. License: CC BY 2.0
Umbilical hernia
Image: “Umbilical hernia” by Saltanat. License: CC0 1.0
Periumbilical bruising consistent with Cullen sign (hemorrhagic pancreatitis)
Image: “Acute pancreatitis with Cullen’s sign” by Herbert L. Fred, MD. License: CC BY 2.0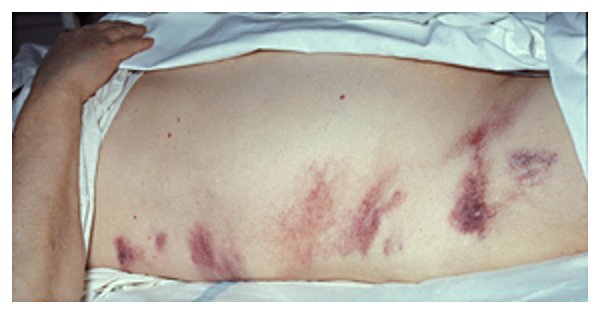
Bruising around the flanks consistent with Grey Turner sign (hemorrhagic pancreatitis)
Image by Herbert L. Fred, MD and Hendrik A. van Dijk. License: CC BY 2.0Because mechanical manipulations of the abdomen can alter the regularity of bowel sounds, auscultation is performed prior to percussion Percussion Act of striking a part with short, sharp blows as an aid in diagnosing the condition beneath the sound obtained. Pulmonary Examination or palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination.
Steps:
Findings:

Auscultation of the abdomen: listening for bowel sounds
Image by Lecturio. License: CC BY-NC-SA 4.0
Auscultation of the abdomen: listening to the bruits over the aorta, iliac, and renal arteries
Image by Lecturio. License: CC BY-NC-SA 4.0
Assessing for shifting dullness
Image by Lecturio. License: CC BY-NC-SA 4.0
Assessing liver size with percussion
Image by Lecturio. License: CC BY-NC-SA 4.0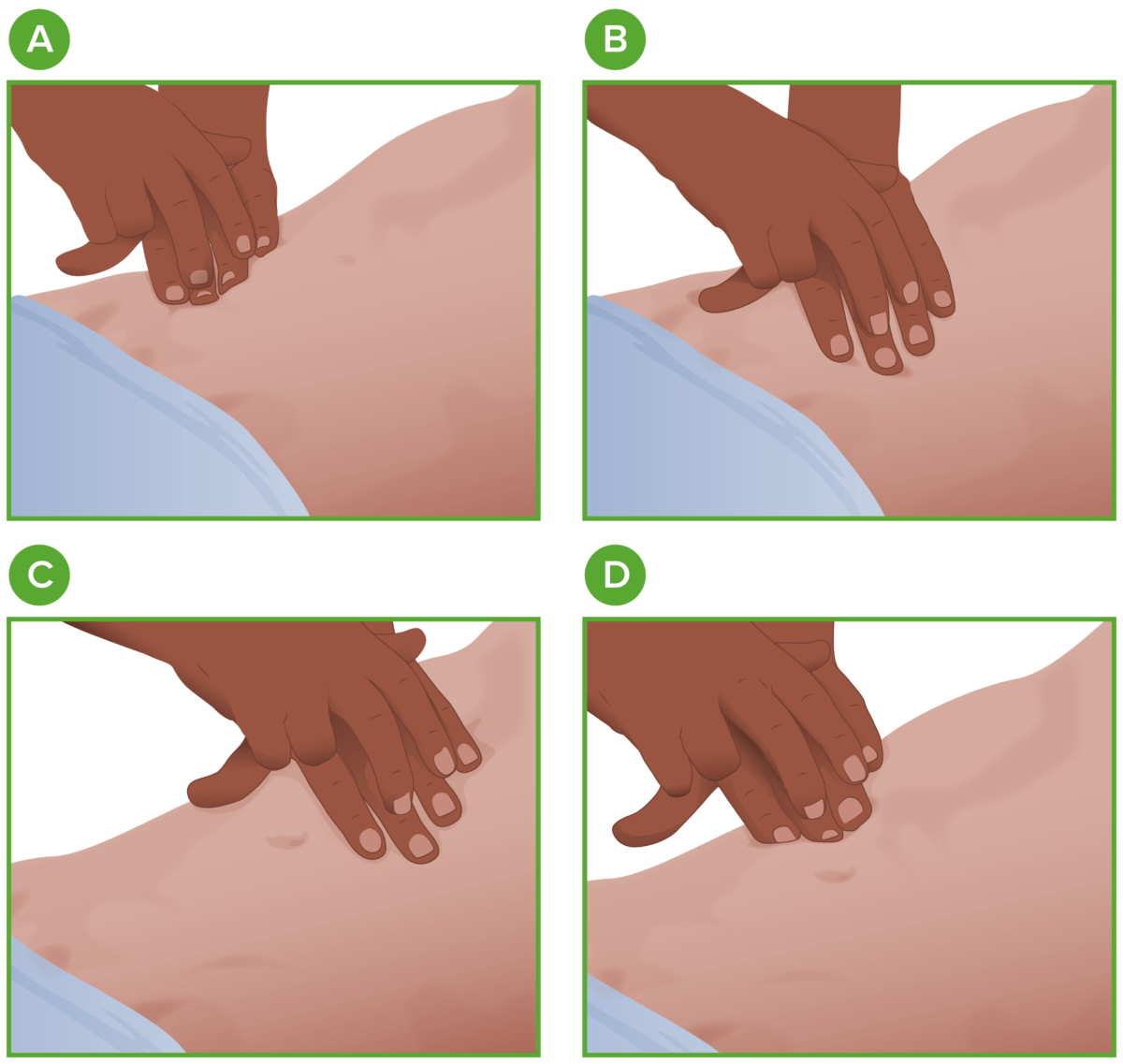
Percussion in the abdominal exam:
The examiner should percuss all 4 quadrants (A, B, C, and D) with 1 middle finger firmly on the individual’s abdominal wall and the 2nd middle finger striking the distal interphalangeal joint.
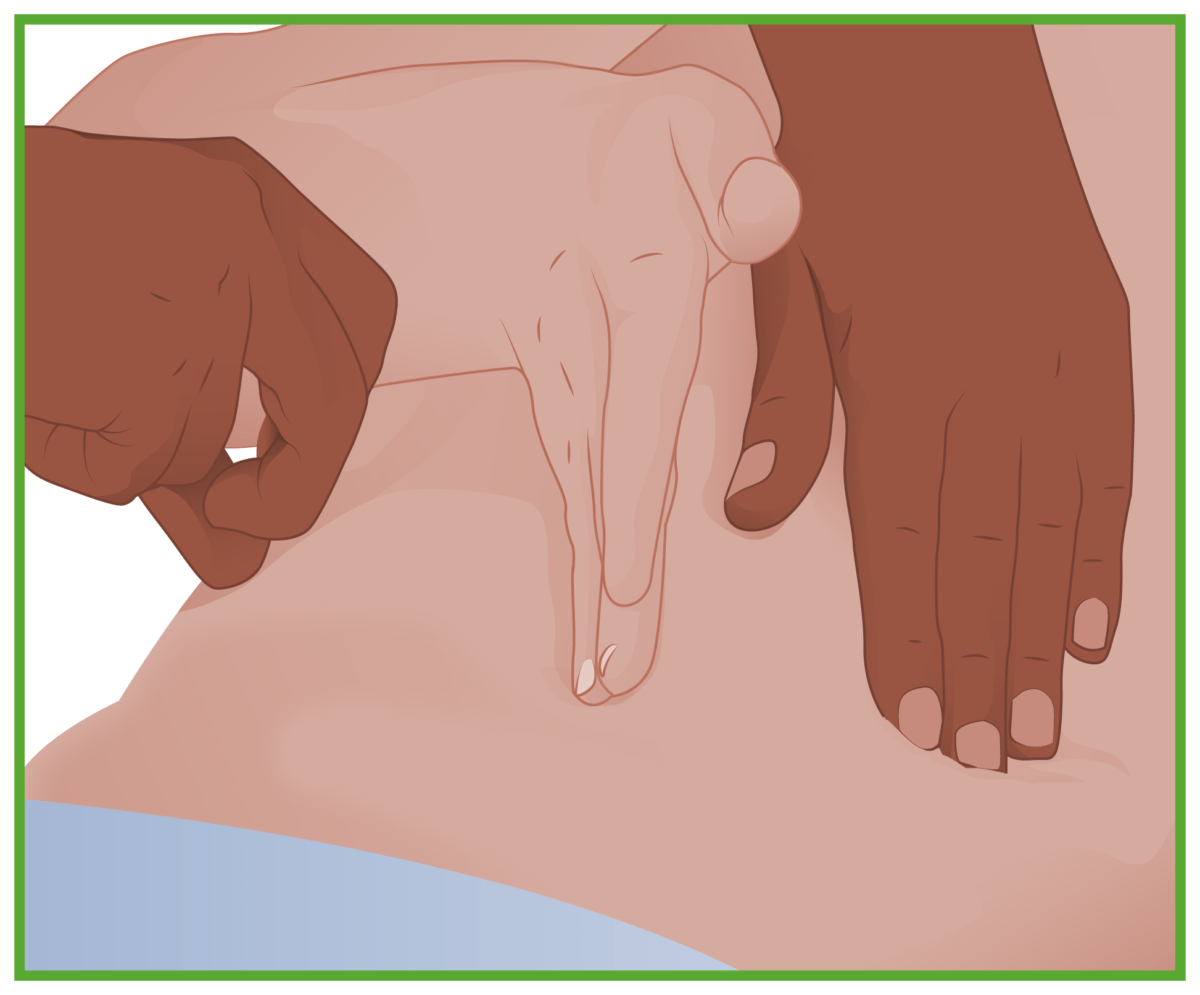
Fluid wave test:
The individual (or another colleague) places their hand on the midline of the abdomen. The examiner then taps on one side. The test is positive if the examiner feels the tap on the other side.
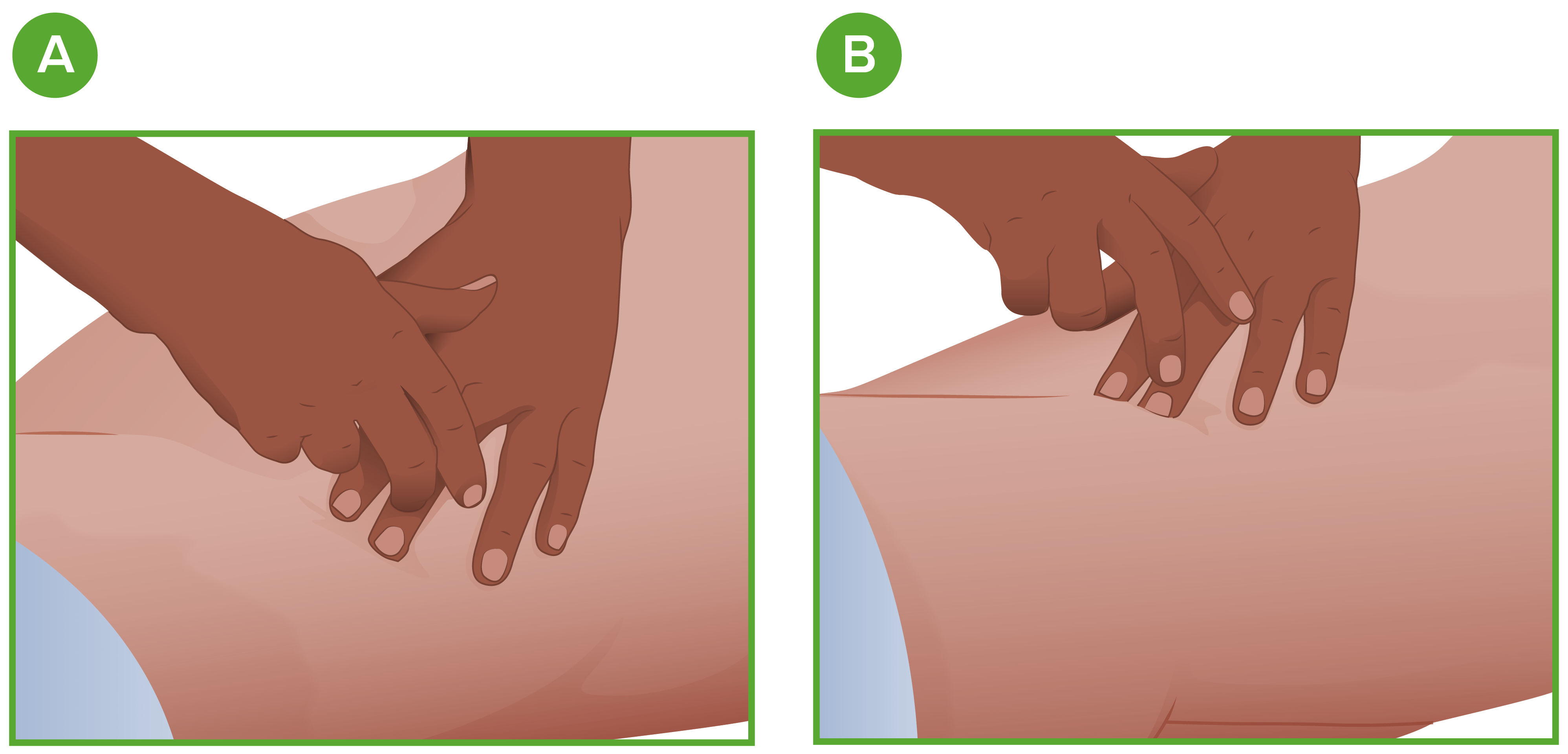
Shifting dullness exam:
A: The examiner percusses laterally from the midline.
B: The individual then leans on their side; the examiner percusses again.
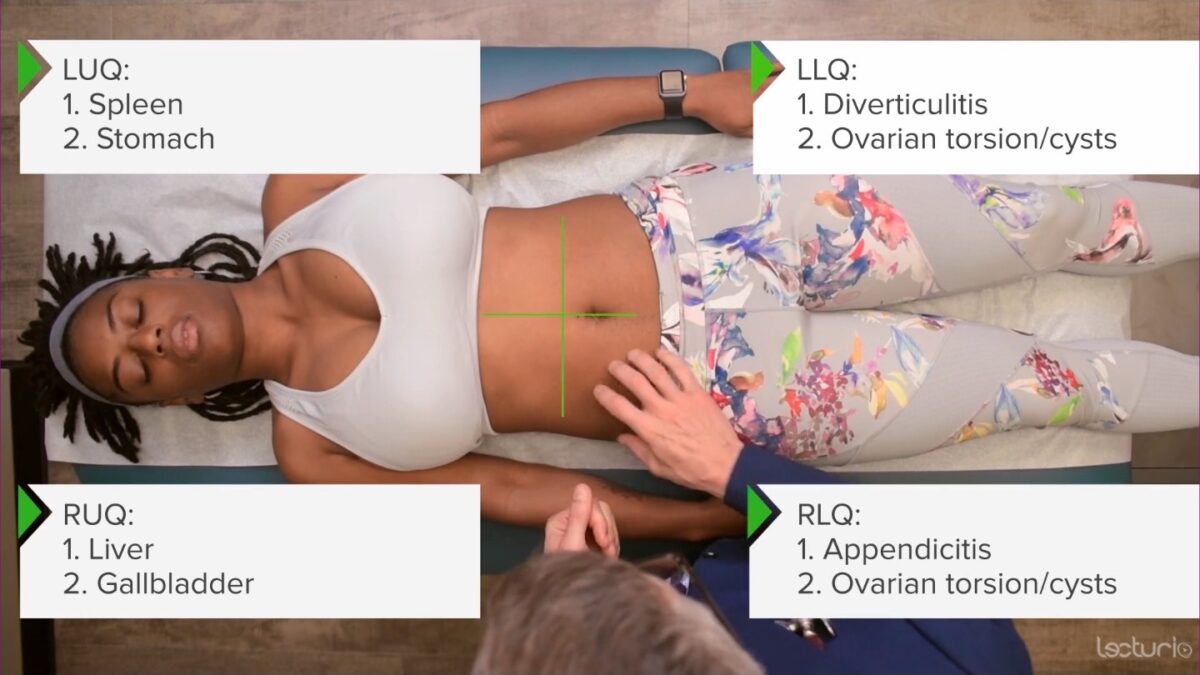
Palpation for abdominal tenderness in the 4 quadrants
Image by Lecturio. License: CC BY-NC-SA 4.0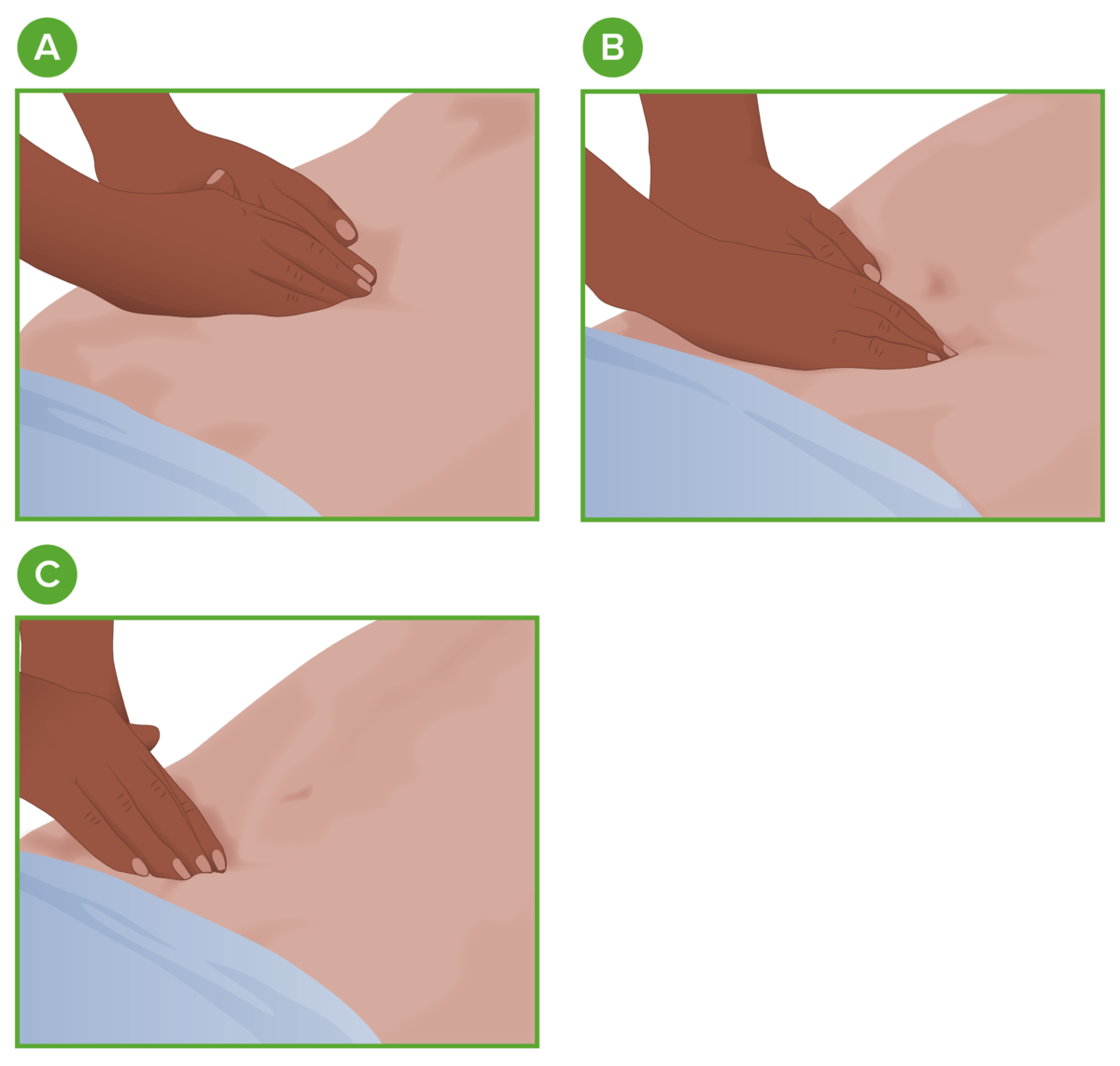
Abdominal palpation
A: Epigastric region
B: Umbilical region
C: Suprapubic region