Prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. cancer is one of the most common cancers affecting men. In the United States, the lifetime risk of being diagnosed with prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. cancer is around 11%, and the lifetime risk of dying from this condition is 2.5%. Prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. cancer is a slow-growing cancer that takes years (even decades) to develop into advanced disease, and many men remain asymptomatic and die from other medical conditions. The preferred method of screening Screening Preoperative Care is with prostate-specific antigen Prostate-specific antigen A glycoprotein that is a kallikrein-like serine proteinase and an esterase, produced by epithelial cells of both normal and malignant prostate tissue. It is an important marker for the diagnosis of prostate cancer. Prostate Cancer ( PSA PSA A glycoprotein that is a kallikrein-like serine proteinase and an esterase, produced by epithelial cells of both normal and malignant prostate tissue. It is an important marker for the diagnosis of prostate cancer. Prostate Cancer) testing. Conditions such as prostatitis Prostatitis Prostatitis is inflammation or an irritative condition of the prostate that presents as different syndromes: acute bacterial, chronic bacterial, chronic prostatitis/chronic pelvic pain, and asymptomatic. Bacterial prostatitis is easier to identify clinically and the management (antibiotics) is better established. Prostatitis and benign Benign Fibroadenoma prostatic hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation are also associated with elevated PSA PSA A glycoprotein that is a kallikrein-like serine proteinase and an esterase, produced by epithelial cells of both normal and malignant prostate tissue. It is an important marker for the diagnosis of prostate cancer. Prostate Cancer levels. Thus, confirmation of the diagnosis may be pursued through prostate biopsy Prostate Biopsy Prostate Cancer, which carries risks. The current recommendation is for the patient and clinician Clinician A physician, nurse practitioner, physician assistant, or another health professional who is directly involved in patient care and has a professional relationship with patients. Clinician–Patient Relationship to have a discussion about the risks and benefits, and to assess the patient’s risk for prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. cancer. Factors considered in the discussion include the patient’s age, life expectancy Life expectancy Based on known statistical data, the number of years which any person of a given age may reasonably expected to live. Population Pyramids, family history Family History Adult Health Maintenance, comorbid conditions, and individual values about screening Screening Preoperative Care and management-associated consequences.
Last updated: Feb 14, 2023
Inherent factors (major factors):
Medical factors:
Social and environmental factors:
Prostate-specific antigen Prostate-specific antigen A glycoprotein that is a kallikrein-like serine proteinase and an esterase, produced by epithelial cells of both normal and malignant prostate tissue. It is an important marker for the diagnosis of prostate cancer. Prostate Cancer is currently the only recommended screening Screening Preoperative Care method for prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. cancer.
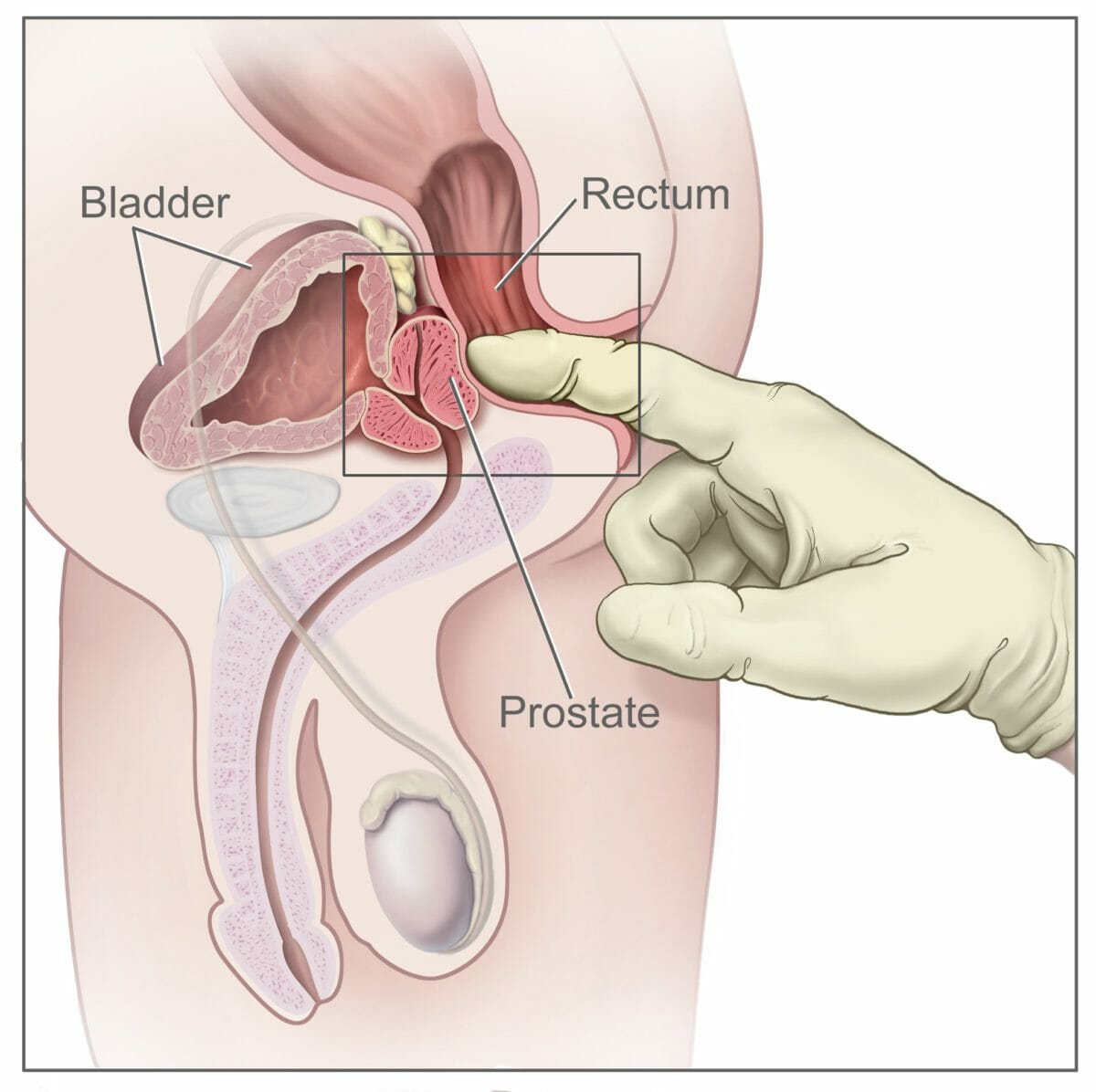
Digital Rectal Examination for screening in Prostate cancer
PD