Cholecystitis is the inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy (GB) usually caused by the obstruction of the cystic Cystic Fibrocystic Change duct (acute cholecystitis). Mechanical irritation by gallstones Gallstones Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis can also produce chronic GB inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation. Cholecystitis is one of the most common complications of cholelithiasis Cholelithiasis Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis (calculous cholecystitis) but inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation without gallstones Gallstones Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis (acalculous cholecystitis) can occur in a minority of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. The acute type usually presents with right upper quadrant Right upper quadrant Anterior Abdominal Wall: Anatomy (RUQ) pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, and leukocytosis Leukocytosis A transient increase in the number of leukocytes in a body fluid. West Nile Virus. The diagnosis is made clinically and confirmed via ultrasound (US). The definitive management is cholecystectomy Cholecystectomy Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis, cholecystitis, gallbladder polyps > 0.5 cm, porcelain gallbladder, choledocholithiasis and gallstone pancreatitis, and rarely, for gallbladder cancer. Cholecystectomy, preferably performed within 72 hours. This condition can present as a mild condition or as a severe disease (with complications such as gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction, perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis, empyema Empyema Presence of pus in a hollow organ or body cavity. Pneumonia) which require emergent intervention.
Last updated: May 17, 2024
Cholecystitis is the
inflammation
Inflammation
Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function.
Inflammation of the
gallbladder
Gallbladder
The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile.
Gallbladder and Biliary Tract: Anatomy (GB).
Types:
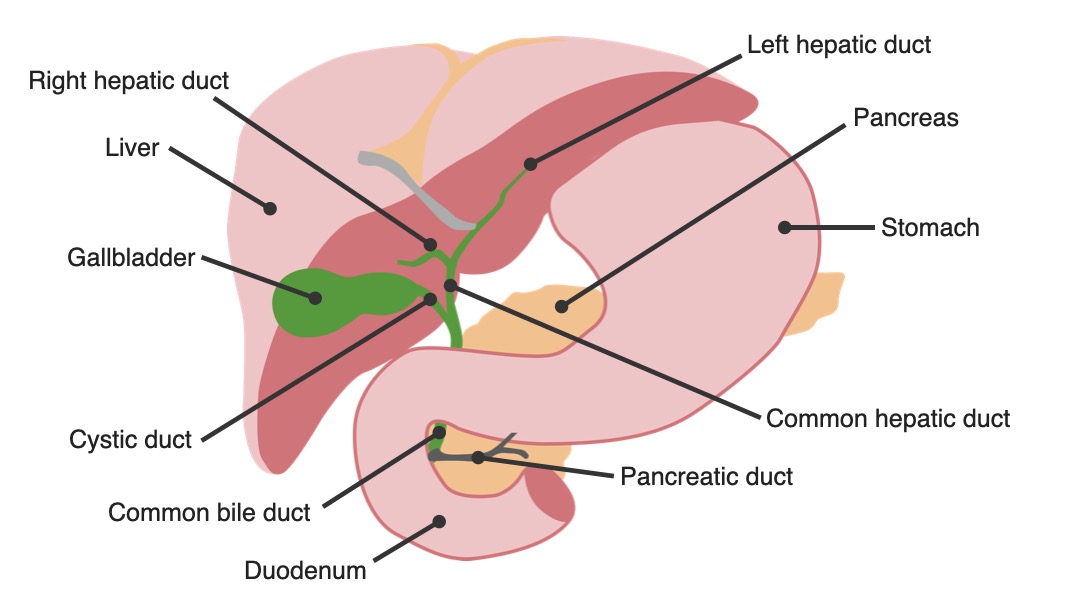
Anatomy of the biliary tree: gallbladder in relation to other organs
Image by Lecturio.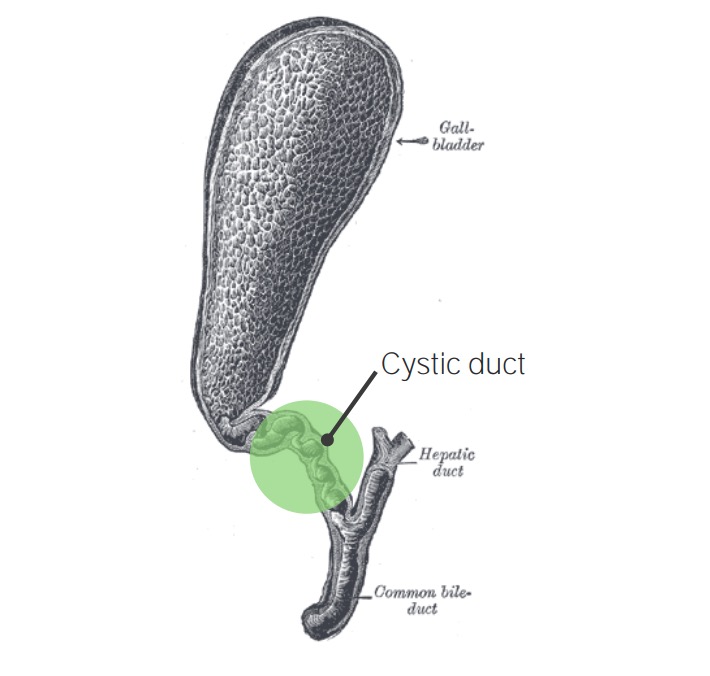
Gallbladder with cholecystitis: cystic duct obstruction
Image: “Gray1095-gall bladder“ by Henry Vandyke Carter. License: Public Domain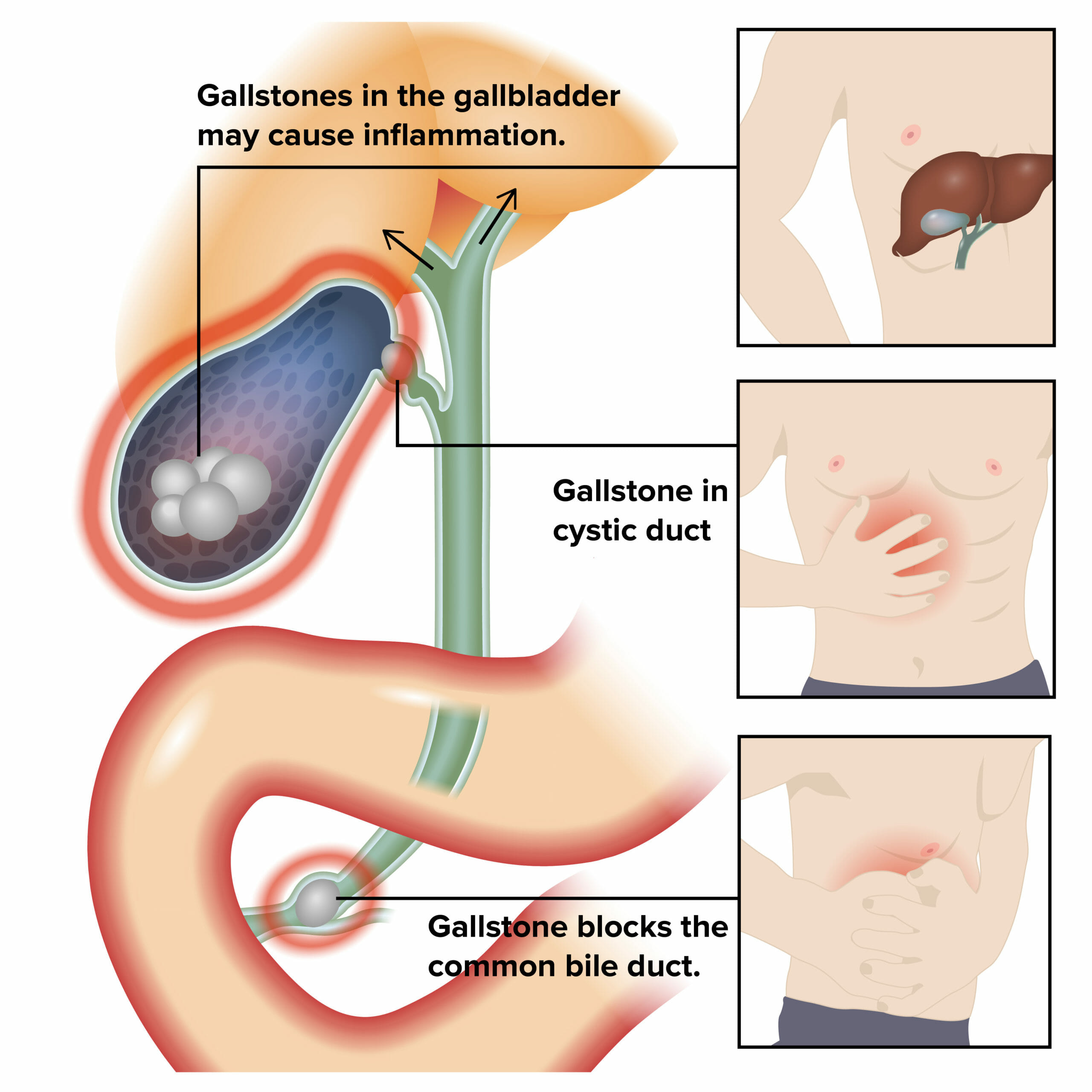
Etiology and pathophysiology of cholecystitis:
Inflammation of the gallbladder and biliary obstruction results in symptoms.

Opened gallbladder with gallstones
Image: “Opened gall bladder containing numerous gallstones” by Emmanuelm. License: CC BY 3.0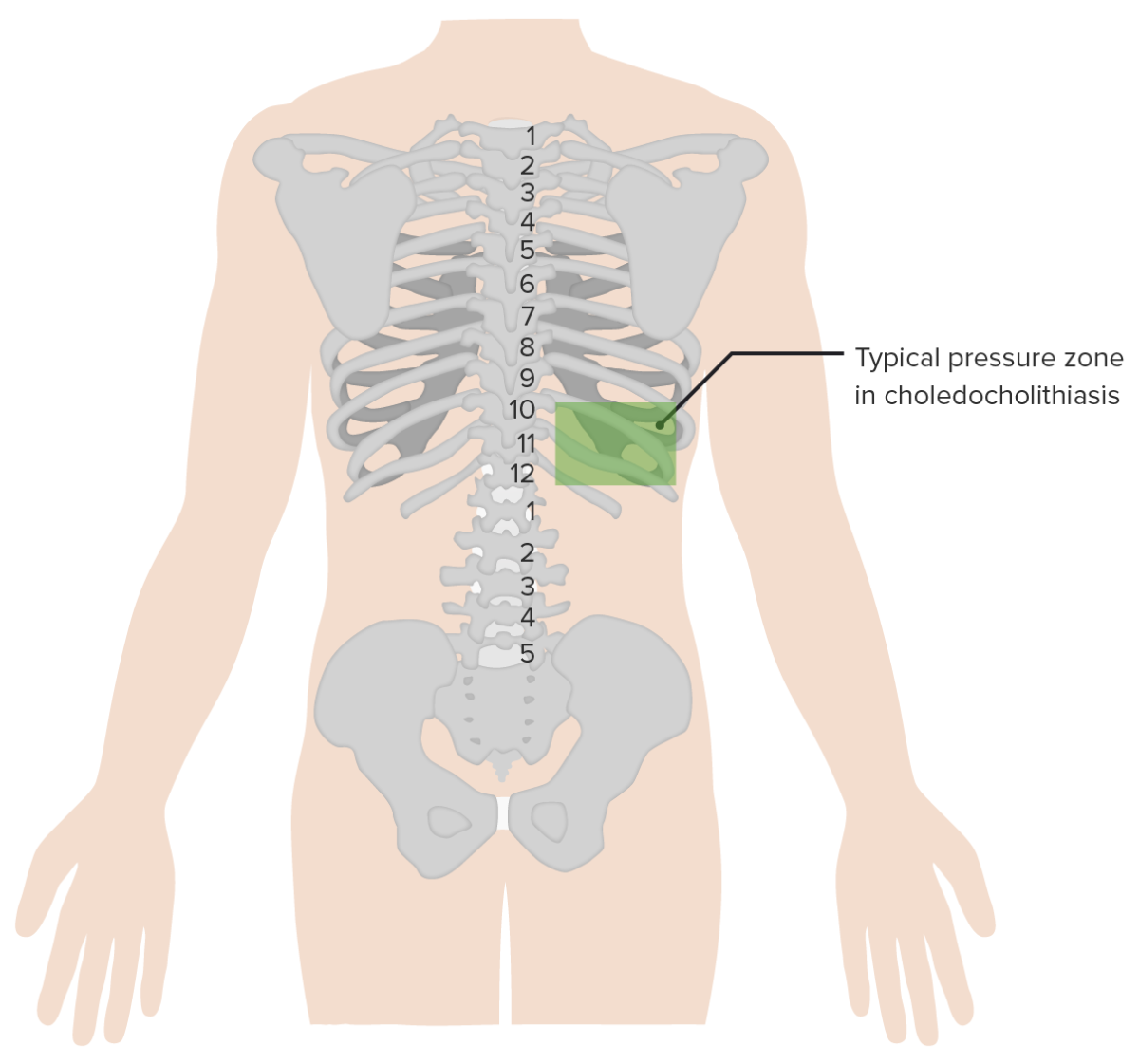
Boas’s sign is hyperesthesia below the right scapula (noted in acute cholecystitis).
Image by Lecturio.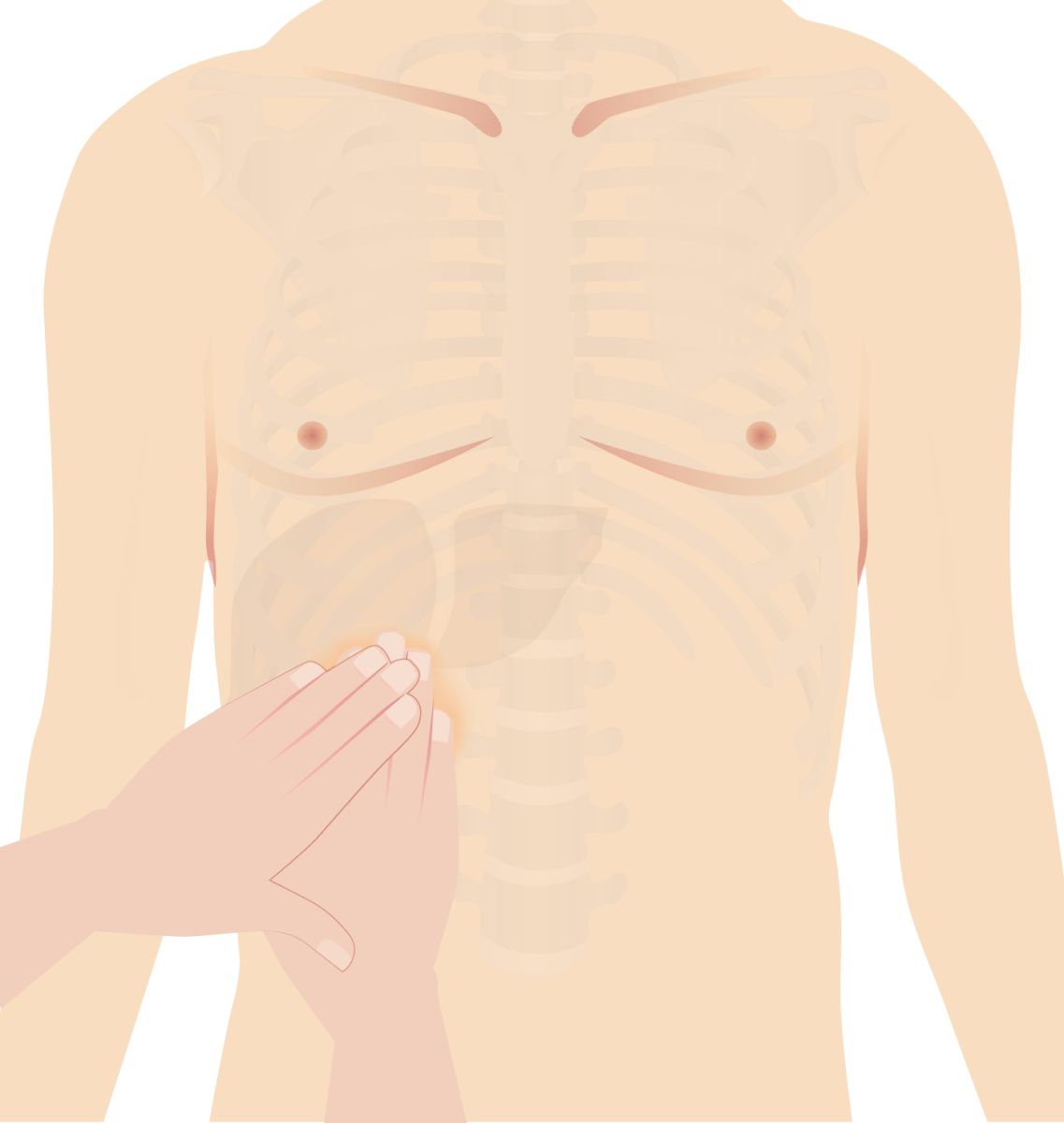
Murphy’s sign: Examiner places hand on the gallbladder area (right subcostal area). Patient is instructed to take a deep breath. On inspiration, the inflamed gallbladder descends, coming in contact with the examiner’s hand and causing pain.
Image by Lecturio.
Ultrasound of a patient with acute cholecystitis: A very large gallstone with significant surrounding edema can be seen.
Image: “Ultrasound of a patient with acute cholecystitis” by Department of Emergency Medicine, University of Maryland School of Medicine, 110 South Paca Street, 6th Floor, Suite 200, Baltimore 21201, MD, USA. License: CC BY 4.0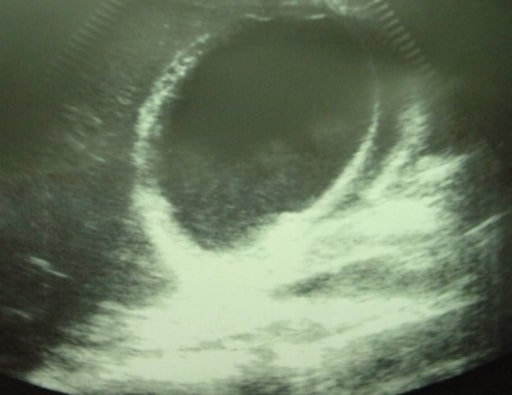
Acute cholecystitis showing pericholecystic fluid
Image: “Ultrasonographic image of the gallbladder” by Department of Surgery, University Hospital Hassan II, Morocco. License: CC BY 2.0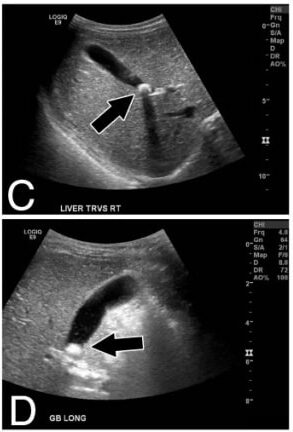
Panels C, D: Transverse and longitudinal ultrasound views of liver and gallbladder (arrows indicate the gallstone)
Image: “Calcified gallstone” by Division of Pediatric Surgery, Children’s Hospital Los Angeles, 4650 Sunset Blvd Mailstop 100, Los Angeles, CA 90027, USA. License: CC BY 2.0