Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis Cholelithiasis Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis, cholecystitis Cholecystitis Cholecystitis is the inflammation of the gallbladder (GB) usually caused by the obstruction of the cystic duct (acute cholecystitis). Mechanical irritation by gallstones can also produce chronic GB inflammation. Cholecystitis is one of the most common complications of cholelithiasis but inflammation without gallstones can occur in a minority of patients. Cholecystitis, gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy polyps > 0.5 cm, porcelain gallbladder Porcelain Gallbladder Cholelithiasis, choledocholithiasis Choledocholithiasis Presence or formation of gallstones in the common bile duct. Cholelithiasis and gallstone pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis, and rarely, for gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy cancer. Over 90% of cholecystectomies are now completed laparoscopically because of the procedure’s enhanced recovery time and decreased postoperative pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Cholecystectomy has a low-risk profile, but the most dreaded complications include vascular and biliary ductal injuries.
Last updated: Jul 26, 2023
Cholecystectomy is the surgical removal of the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy, which can be performed using either an open or a laparoscopic method.
Gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy:
Biliary tree Biliary tree The bile ducts and the gallbladder. Gallbladder and Biliary Tract: Anatomy:
Calot’s (hepatobiliary) triangle:
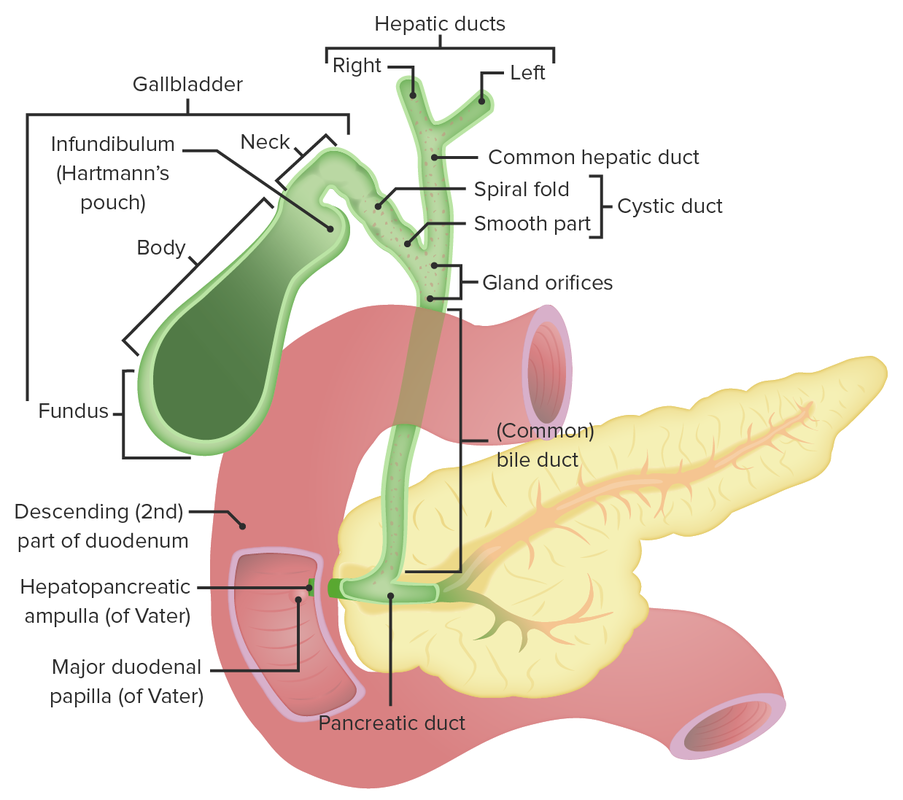
Anatomy of the gallbladder and the biliary tree
Image by Lecturio.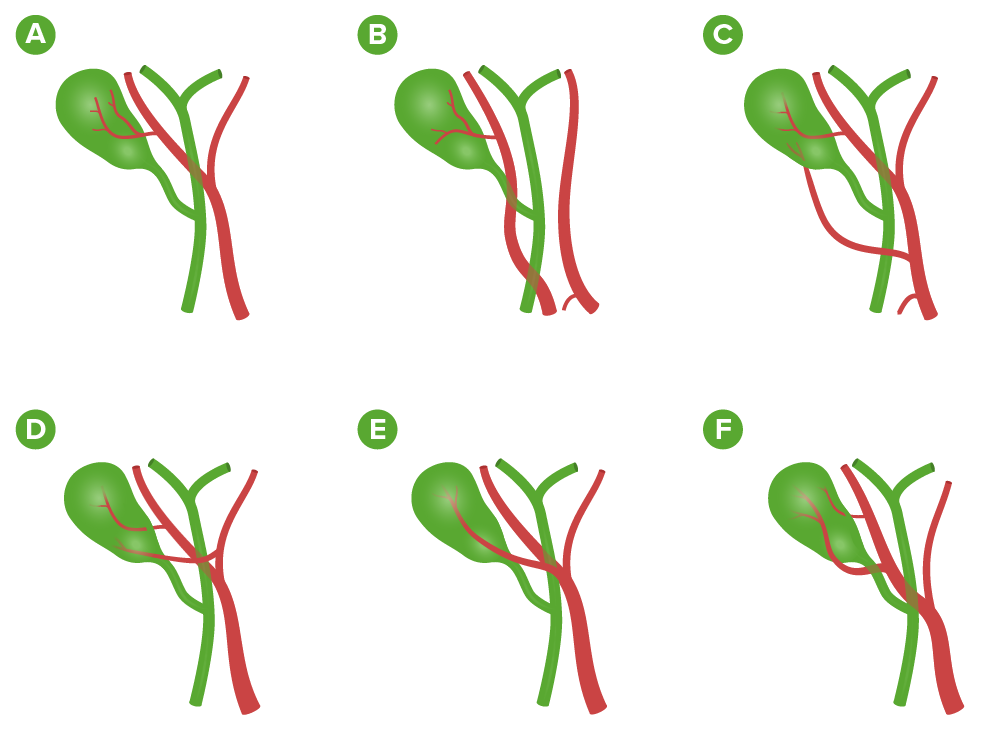
Variations in the arterial supply to the gallbladder:
A: From the right hepatic artery (most common: 90%)
B: From the right hepatic artery arising from the superior mesenteric artery
C: 2 cystic arteries: from the right hepatic and common hepatic arteries
D: 2 cystic arteries: from the right and left hepatic arteries
E: From the right hepatic artery and running anterior to the common hepatic duct
F: 2 cystic arteries from the right hepatic artery
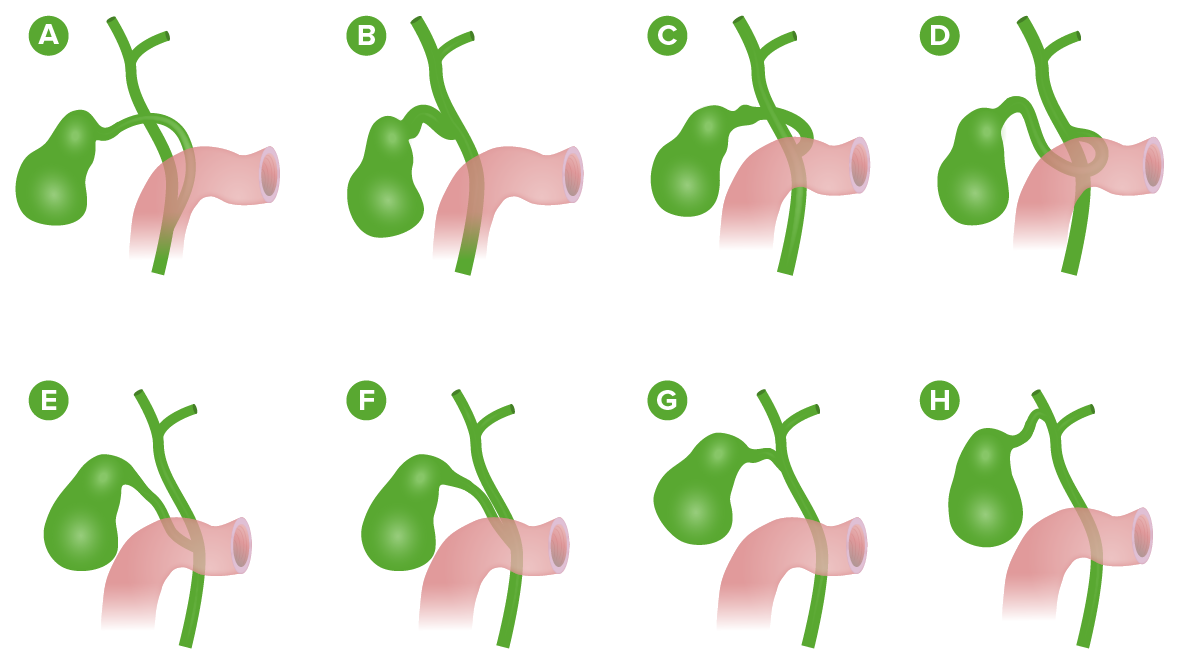
Variations of the cystic duct anatomy:
A: Long cystic duct joins the common hepatic duct behind the duodenum.
B: Absence of cystic duct
C: Cystic duct crosses posteriorly to common hepatic duct and joins it anteriorly.
D: Cystic duct crosses anteriorly to common hepatic duct and joins it posteriorly.
E: Low junction between the cystic duct and common hepatic duct
F: Cystic duct adherent to the common hepatic duct
G: High junction between the cystic and the common hepatic ducts
H: Cystic duct drains into right hepatic duct.
The goal of surgical treatment is to remove the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy and the stones it contains, while ensuring that no stones remain within the ductal system. The goals are the same for both the laparoscopic and the open approach.
Laparoscopic cholecystectomy is considered the gold standard, as it results in decreased postoperative pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, a shorter hospital stay, and an earlier return to work. Over 90% of cholecystectomies are performed laparoscopically. Conversion to an open approach is mandatory if anatomy is not clear.
Laparoscopic cholecystectomy:
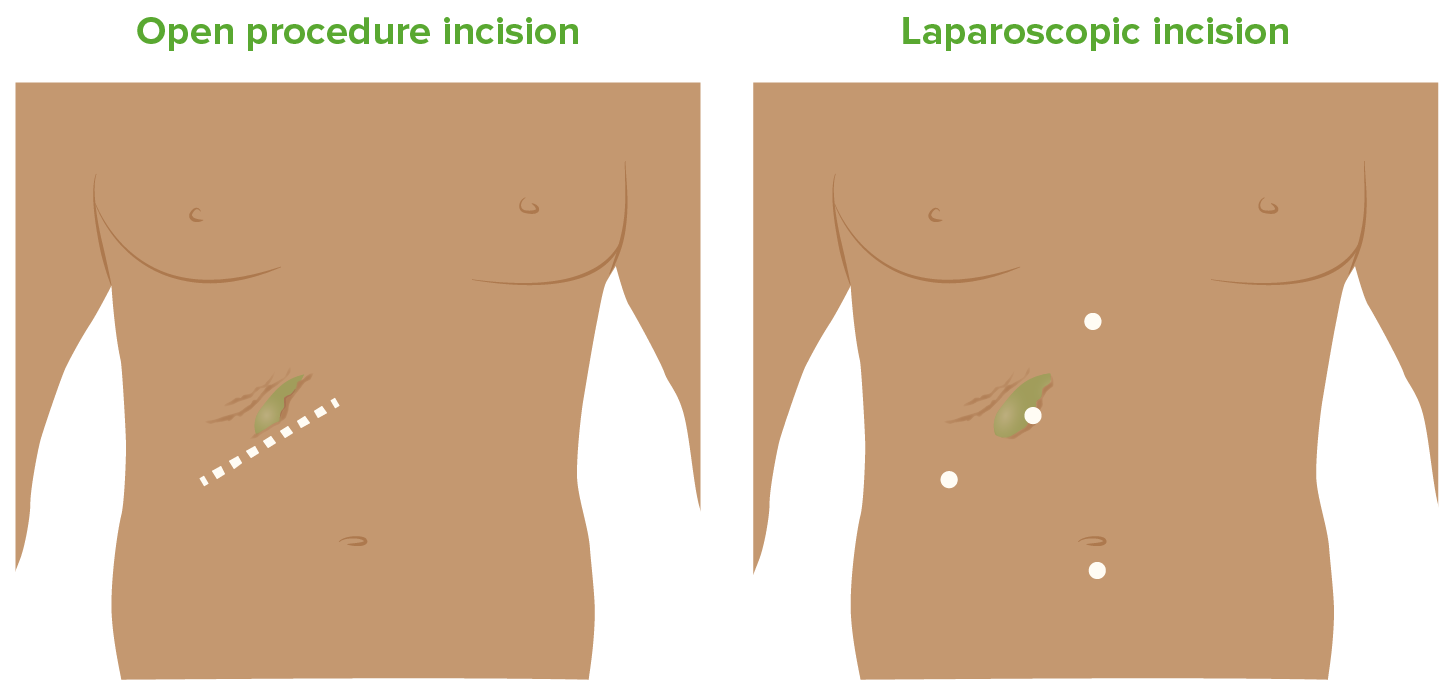
Incisions for open and laparoscopic cholecystectomy
Image by Lecturio.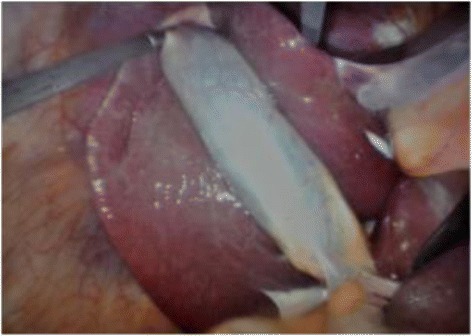
Laparoscopic view of the gallbladder:
The grasper is on the fundus of the gallbladder and is retracting it cephalad over the liver.
Open cholecystectomy:
Cholecystectomy has a low-risk profile; however, like any other surgical procedure, it has inherent risks and complications.