Computed tomography (CT) is one of the most commonly used imaging methods because it is widely available, fast, and reliable. CT scans deploy X-rays X-rays X-rays are high-energy particles of electromagnetic radiation used in the medical field for the generation of anatomical images. X-rays are projected through the body of a patient and onto a film, and this technique is called conventional or projectional radiography. X-rays to obtain cross-sectional images of the body. A CT scanner consists of a tube that rotates around the patient and emits an X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests beam and a detector that uses specialized software to receive and convert the beam to an image. The ability to create multiple views (axial, sagittal, coronal) and use contrast (intravenous, oral, rectal) allows for enhanced diagnostic yield. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are exposed to radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma, and special consideration should be given to patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with a history of iodine Iodine A nonmetallic element of the halogen group that is represented by the atomic symbol I, atomic number 53, and atomic weight of 126. 90. It is a nutritionally essential element, especially important in thyroid hormone synthesis. In solution, it has anti-infective properties and is used topically. Thyroid Hormones allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction, renal disease, or thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy disease or patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are pregnant.
Last updated: Mar 29, 2023
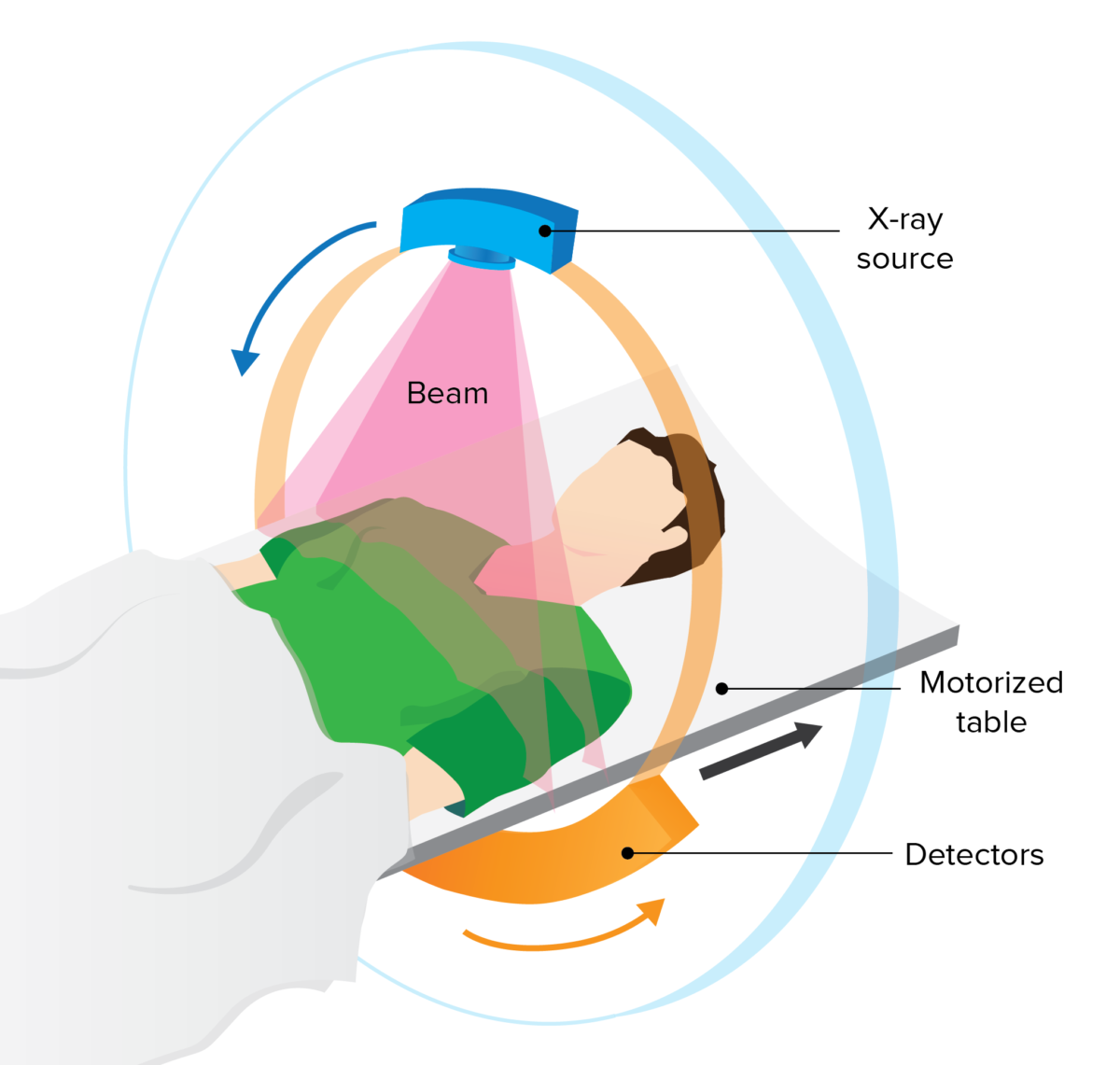
CT scan components:
Arrangement of the X-ray tube and detectors in the CT scanner

The motorized table moves the patient through the scanner, which contains the X-ray tube and detectors.
Image: “UPMCEast CTscan” by daveynin. License: CC BY 2.0Helical (“spiral”):
Sequential (step-and-shoot):
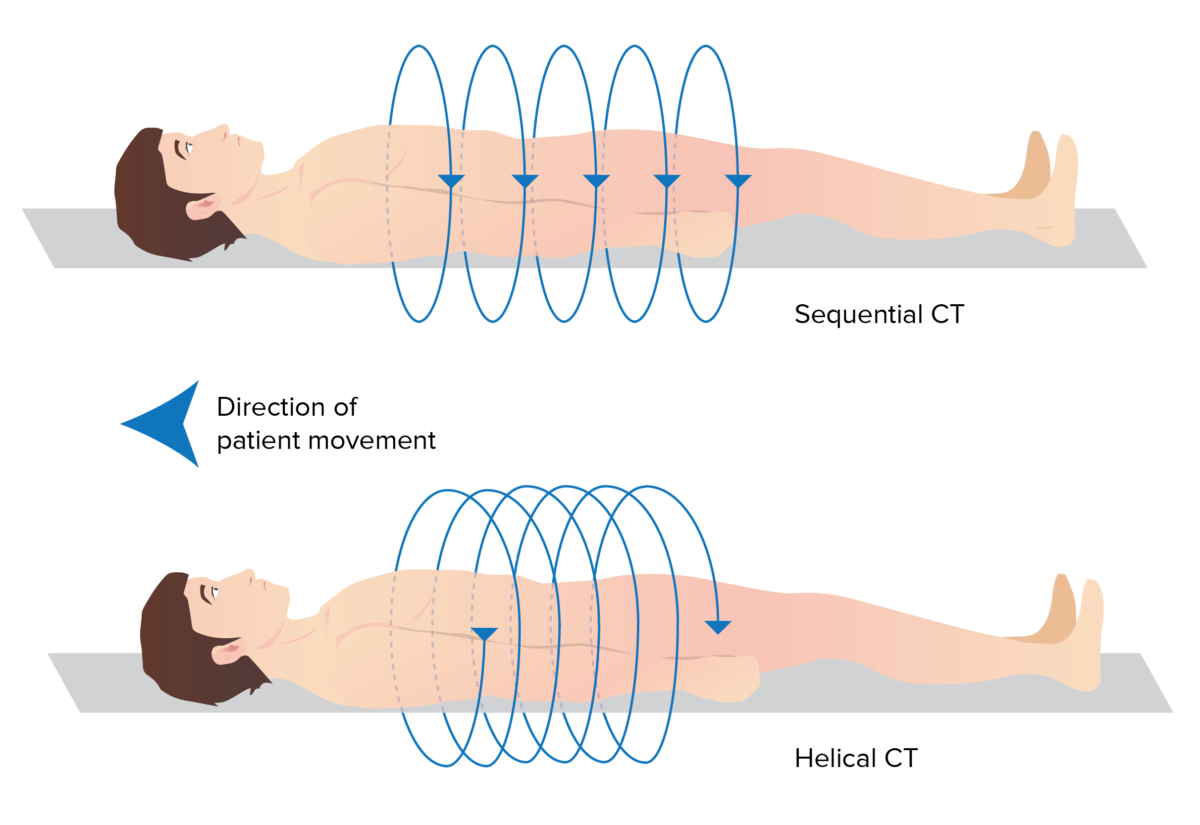
Differences between sequential and helical CT scanners:
Sequential CT takes discrete imaging slices as the patient moves through the scanner, whereas the continuous movement of the helical CT results in a spiral path.
Digital images are created with a matrix of voxels (3-dimensional pixels), which are measured in Hounsfield units (HU).
Postprocessing can be used to accentuate tissues of different densities.
Images can also be produced in different viewing planes.
| Substance | Hounsfield units (HU) | |
|---|---|---|
| Air | –1000 | The darkest (most hypodense) The brightest (most hyperdense) |
| Fat | –100 to –50 | |
| Water | 0 | |
| Soft tissue Soft Tissue Soft Tissue Abscess | 20–300 | |
| Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types | 250‒700 |
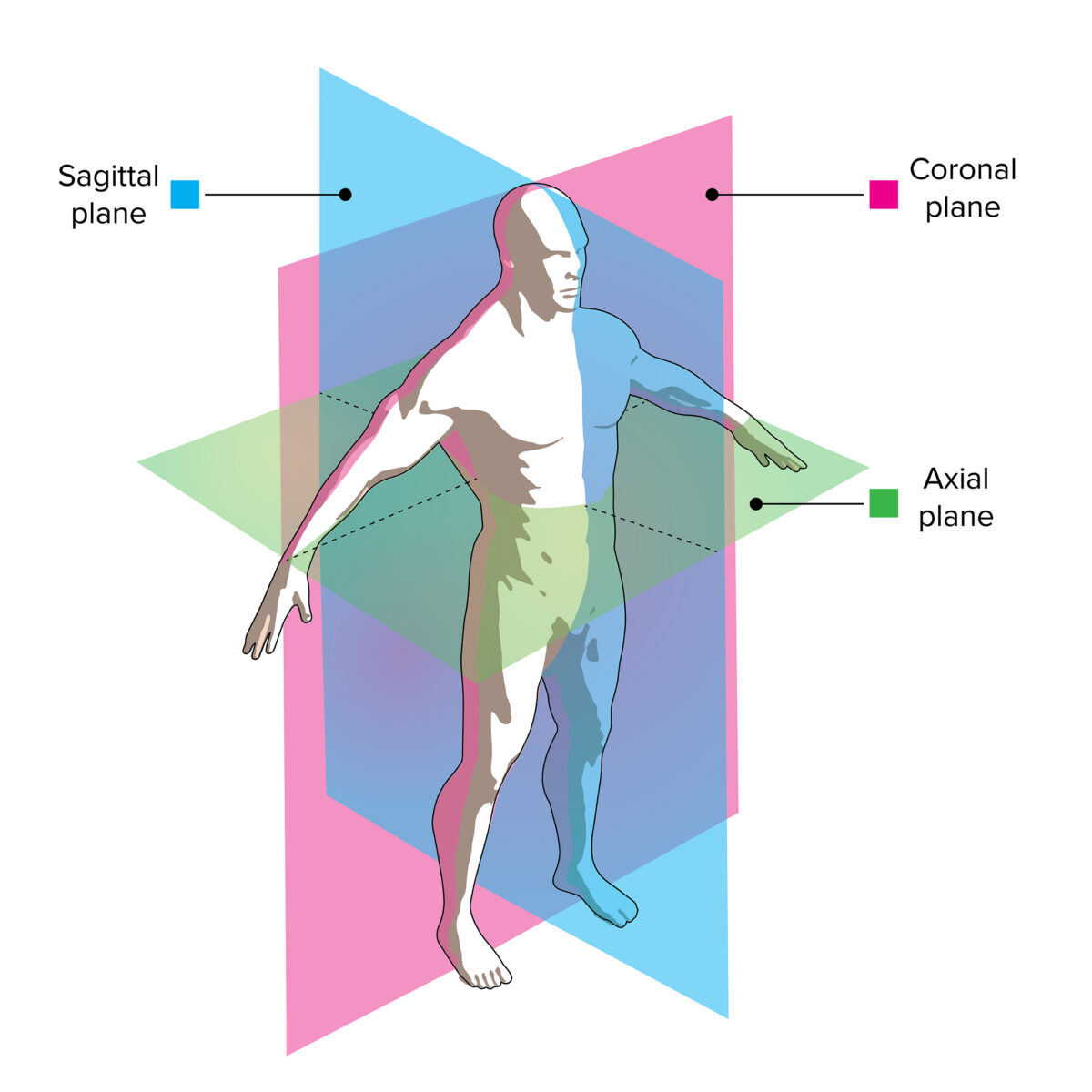
CT image viewing planes:
The slices through this model demonstrate how axial, coronal, and sagittal images correlate with the patient’s anatomy.
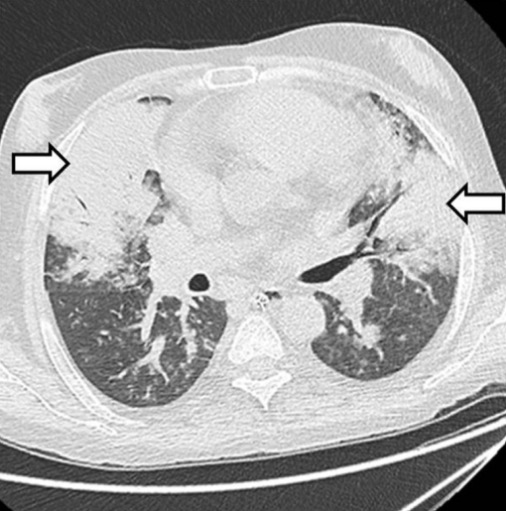
Lung window showing bilateral areas of airspace consolidation
Image: “Fungal pneumonia” by Department of Radiology/Interventional Radiology, Institute of Liver and Biliary Sciences, Vasant Kunj, New Delhi, India. License: CC BY 4.0
Bone window showing multiple lateral and anterior sclerotic bone lesions with fractures
Image: “Adenocarcinoma” by Department of Radiology, University of Yamanashi, Chuo City, Japan. License: CC BY 2.0, cropped by Lecturio.
Soft tissue window showing bilateral dependent effusions and irregular contour of the descending aorta with contrast extravasation outside the lumen, consistent with aortic rupture
Image: “Axial chest CT” by Department of Radiology, Faculty of Medicine, Bezmialem Vakif University, Fatih, 34090 Istanbul, Turkey. License: CC BY 3.0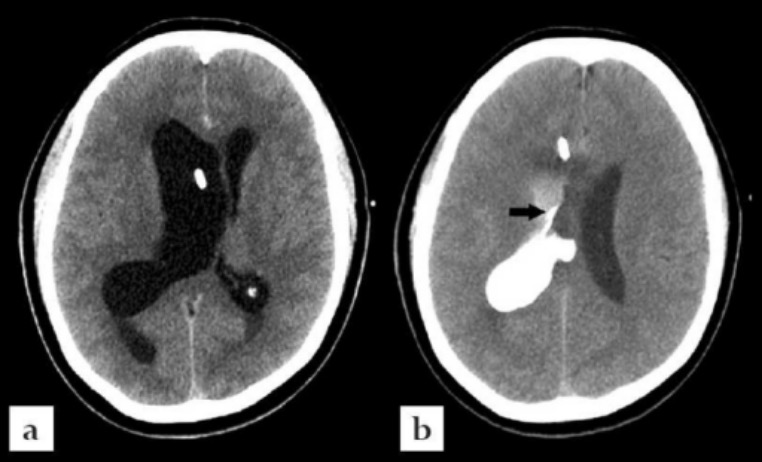
Axial CT images of the brain:
Administration of contrast via the right frontal approach external ventricular drain reveals the presence of obstruction at the level of the foramen of Monro.

CT images demonstrate different CT planes:
Coronal plane (A) and sagittal plane (B)
Contrast agents may be used to enhance visualization of targeted tissues.
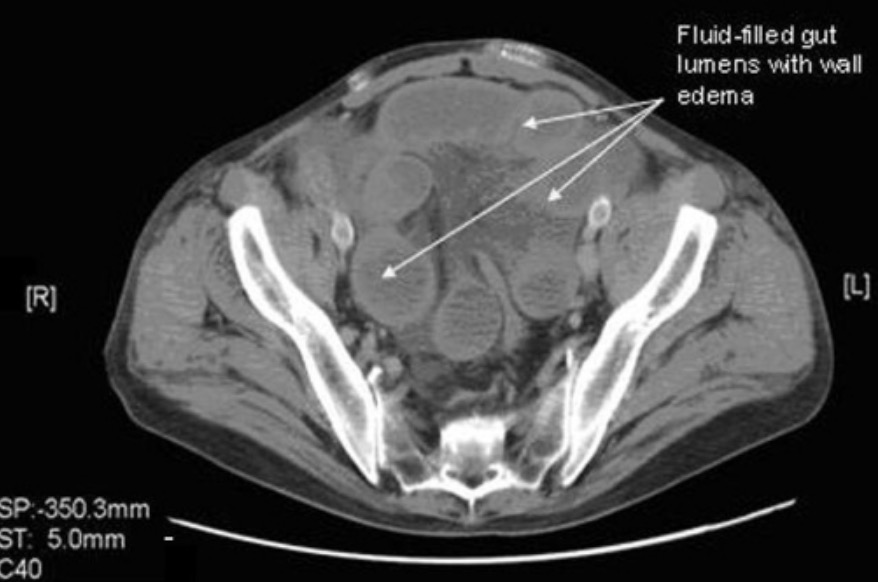
CT without oral contrast agent from a patient with Meckel diverticulum:
Note how the contrast agent in the next CT enhances the bowel in comparison to this one. In this case, the transition from enhanced to nonenhanced bowel allows the viewer to see where the bowel obstruction is located.

CT with oral contrast agent from a patient with Meckel diverticulum:
Note how the contrast agent enhances the bowel. In this case, the transition from enhanced to nonenhanced bowel allows the viewer to see where the bowel obstruction is located.
Multiphase CT can identify structures at various intervals after IV contrast administration.
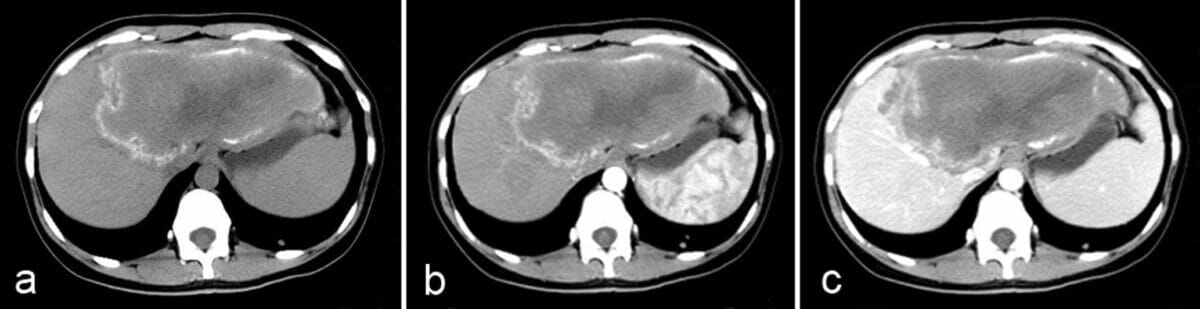
Axial multiphase CT images of the abdomen:
a: Unenhanced image shows an infiltrative tumor-like hepatic mass.
b: Postcontrast arterial phase shows a nonenhancing, hypoattenuating lesion.
c: Postcontrast portal-venous phase shows a faint enhancement of fibroinflammatory components surrounding the parasitic pseudocyst.
The best approach is a systematic approach.
Noncontrast:
Contrast:
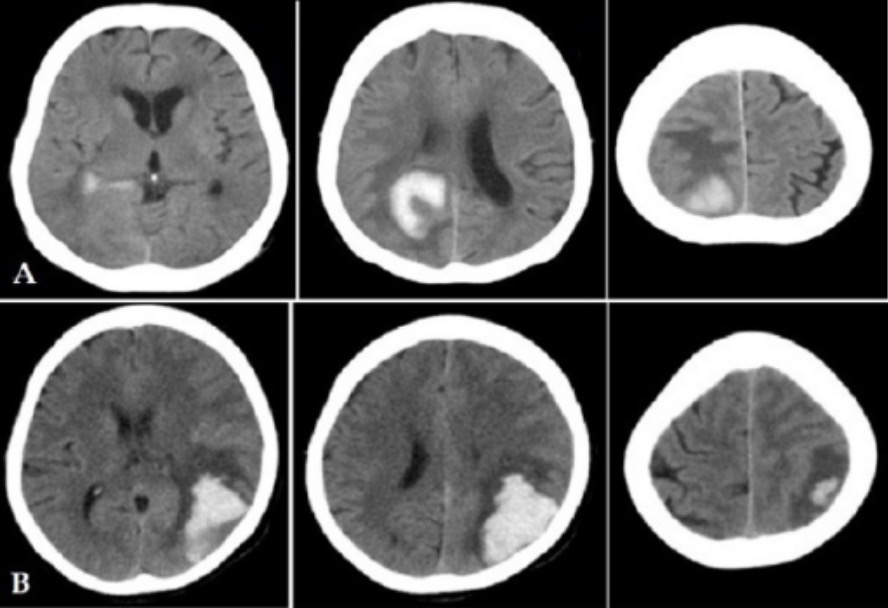
Multislice CT imaging of the brain showing hemorrhagic stroke in 2 patients (A and B)
Image: “Head MSCT imaging of haemorrhagic stroke patients” by Medical Doctor of Radiology. tatan_saepudin@yahoo.com. License: CC BY 3.0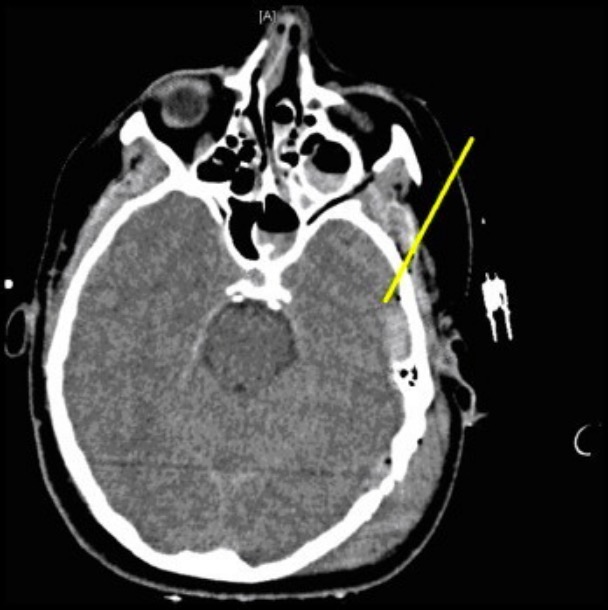
Left temporal bone fracture, pneumocephalus (air within the cranial cavity), and left-sided epidural hematoma
Image: “Left temporal bone fracture, pneumocephalus and left-sided epidural hematoma” by University of North Carolina, Chapel Hill, United States. License: CC BY 3.0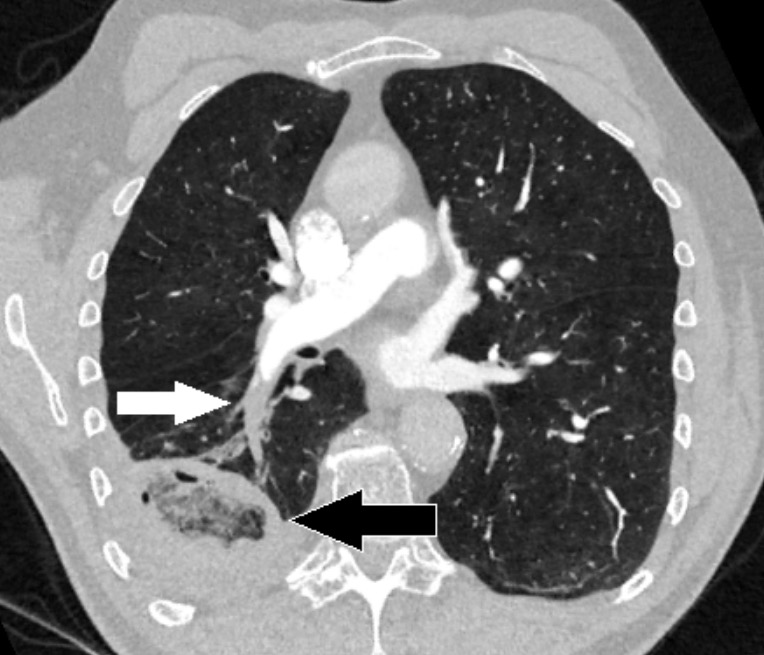
Chest CT with angiography showing a pulmonary embolism (white arrow) in the artery in the right lower lobe:
A pulmonary infarction is also seen as a reverse halo sign (black arrow).

Typical thin-sliced CT images of central (A) and peripheral (B) types of small-cell lung carcinoma (SCLC):
Each black arrow indicates the primary mass.
Evaluation for abdominal and pelvic pathology:
Evaluation of visceral malignancies:
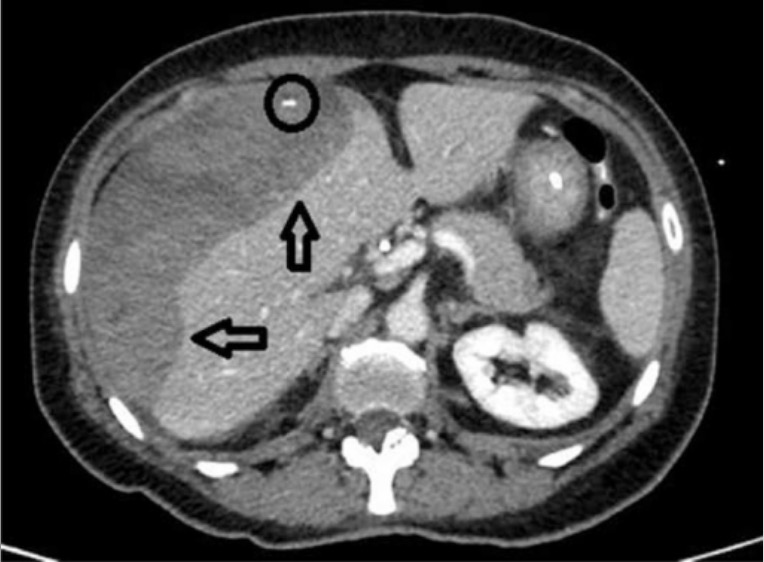
CT scan of the middle abdomen showing a subcapsular hepatic hematoma on the surface of the right lobe of the liver (hypodense area indicated by the arrows) with a source of active bleeding (circle)
Image: “CT scan of middle abdomen showing a subcapsular hepatic hematoma” by From the Department of General Surgery, C.S. General and Emergency Surgery, Azienda Ospedaliera – IRCCS Arcispedale Santa Maria Nuova, Reggio Emilia, Italy. License: CC BY 4.0Like other imaging methods, CT scans expose patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship to radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma.
| Radiography | CT | Ultrasound | MRI | |
|---|---|---|---|---|
| Mechanism of acquisition | Ionizing radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma | Ionizing radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma | Acoustic energy | Ferromagnetic pulses |
| Relative cost | Inexpensive | Expensive | Inexpensive | Very expensive |
| Portable | Yes | No | Yes | No |
| Length of exam | Seconds | < 1 minute | Seconds | Approximately 1 hour |
| Contrast | No | May be needed | May be needed | May be needed |