The urinary tract is located in the abdomen and pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 "hip" bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy and consists of the kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy, ureters, urinary bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy through the ureters to the urinary bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess and out through the urethra. The bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess acts as a reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli for urine until micturition is appropriate. Regulation of micturition relies on the CNS and the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy.
Last updated: Nov 18, 2024
Kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy go through 3 embryologic stages:
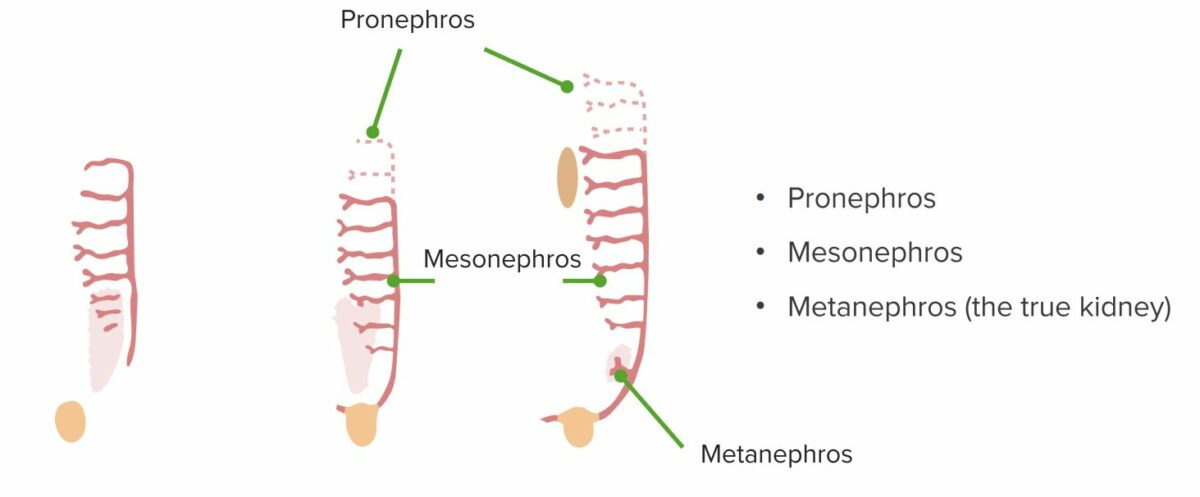
Stages of renal development: pronephros, mesonephros and metanephros
By the 3rd week, the pronephros, a segmented structure made out of a duct with a series of tubules branching off toward the midline of the embryo (1 on each side), is formed. The pronephros does not develop beyond a rudimentary state and undergoes regression. Caudal to the pronephros (in the thoracic and lumbar area), the mesonephros (a tubular structure) begins to form by the 4th week, while the pronephros is still regressing. The mesonephros is an elongated organ, connected to the pronephric duct via the mesonephric duct. Caudally, it continues as the mesonephric (wolffian) duct and connects to the cloaca. The mesonephros also eventually regresses. A few tubules remain, later becoming the efferent ducts of the epididymis in men. The ureteric bud develops from the duct. The metanephros, the urine-producing organ, forms by the 5th week, with the ureteric bud meeting the metanephric blastema.
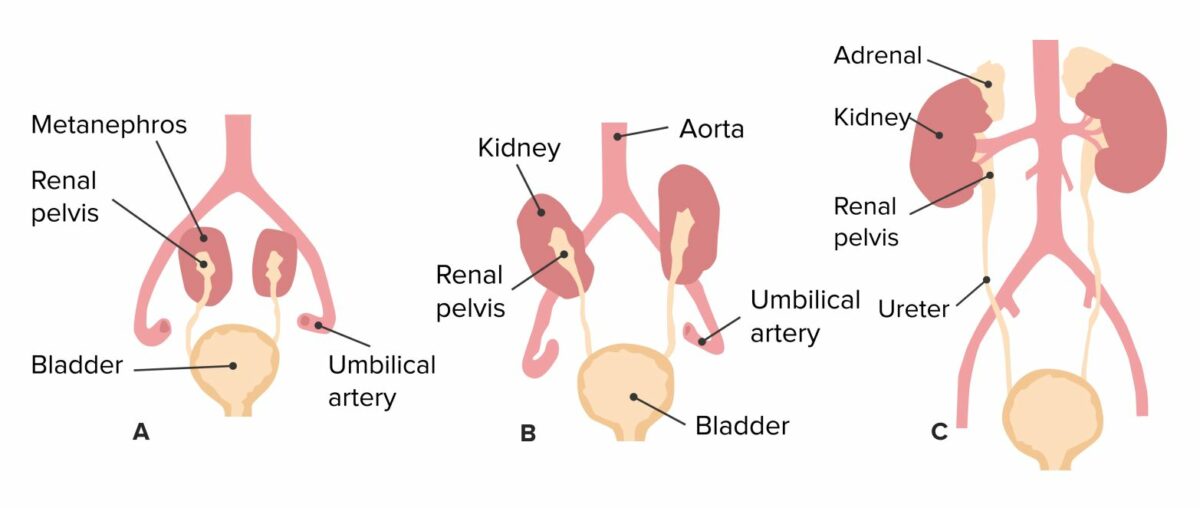
Ascent of the kidneys and development of the structures of the urinary tract
Image by Lecturio.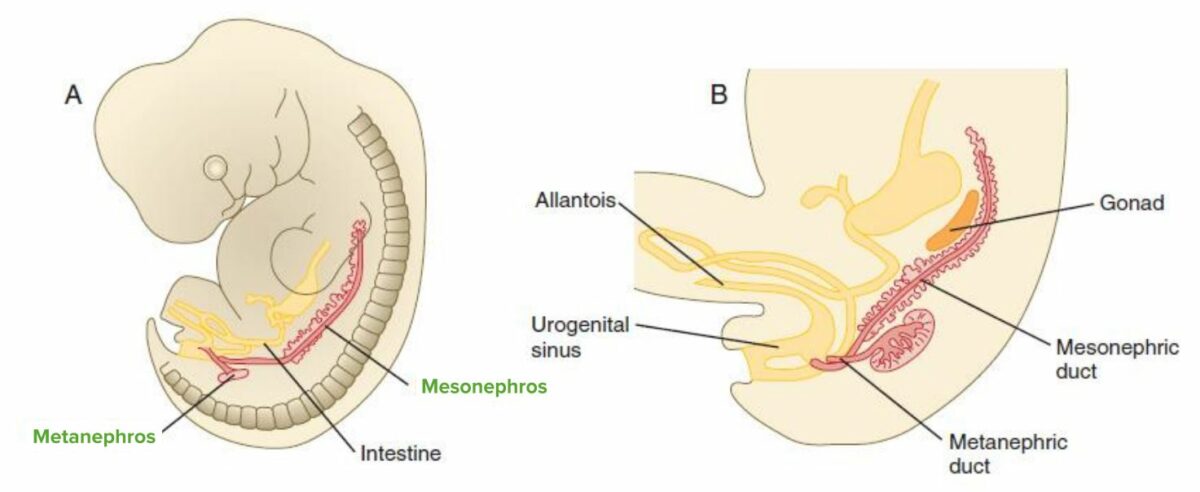
Development of the kidney and bladder
A: The metanephros forms by the 5th week, with the ureteric bud meeting the metanephric blastema, and the mesonephros regresses.
B: The mesonephric duct fuses with the cloaca, with a portion of the duct becoming part of the posterior bladder. During gestational week 7, the cloaca is divided by the urogenital membrane/septum into ventral (urogenital sinus) and dorsal (rectum) components. The urogenital sinus gives rise to the bladder (cranially) and the urethra (caudally).
Description:
Function:
The function of the ureters is to transport urine from the renal pelvis Renal pelvis Kidneys: Anatomy to the urinary bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess.
Route of ureters:
3 sites of narrowing:
Vasculature and lymphatic drainage:
Innervation:
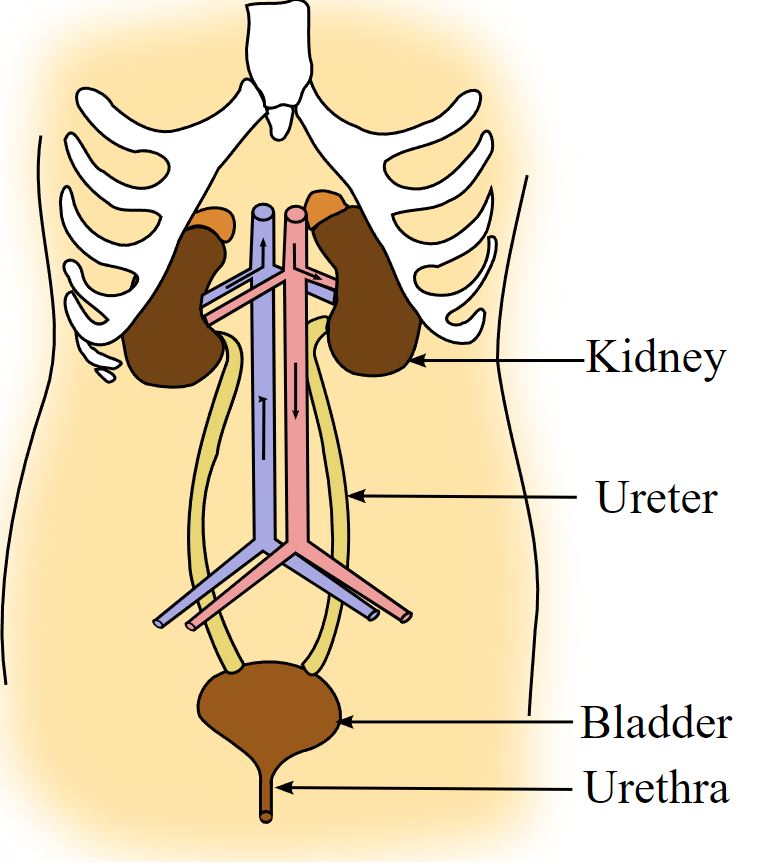
Diagram of the gross anatomy of the urinary system, showing the kidney, renal pelvis, ureter, urinary bladder, and urethra.
Image: “Illu urinary system” by Arcadian. License: Public DomainUreteral wall structure from the lumen toward the outside:
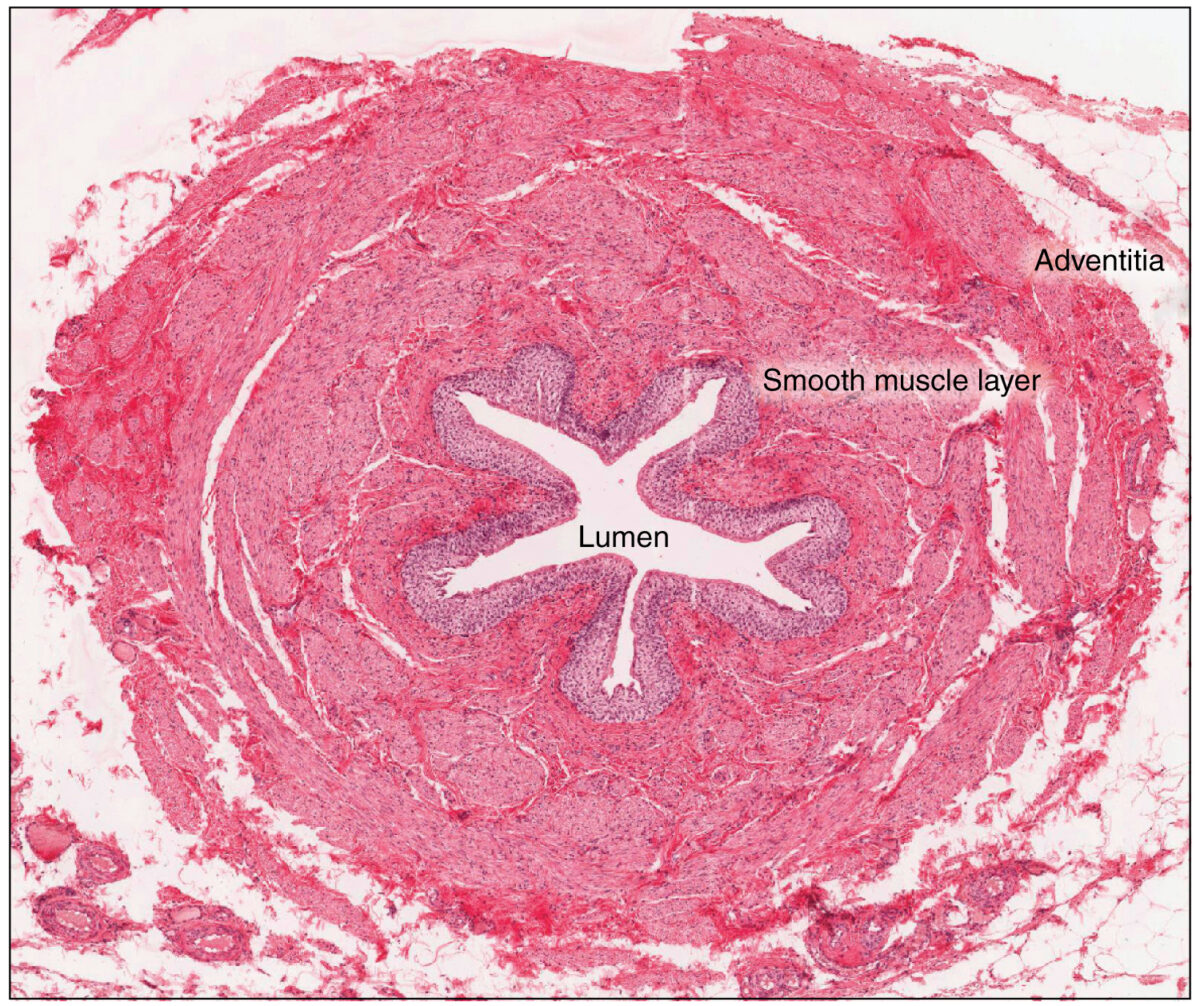
Cross-sectional histologic view of the ureter:
Various tissue types within the ureter are illustrated. Note the outermost adventitial layer, deep to which are found the muscular layer, loose connective tissue, and interior lumen lined with urothelium.
Description:
Parts:
Spatial relations:
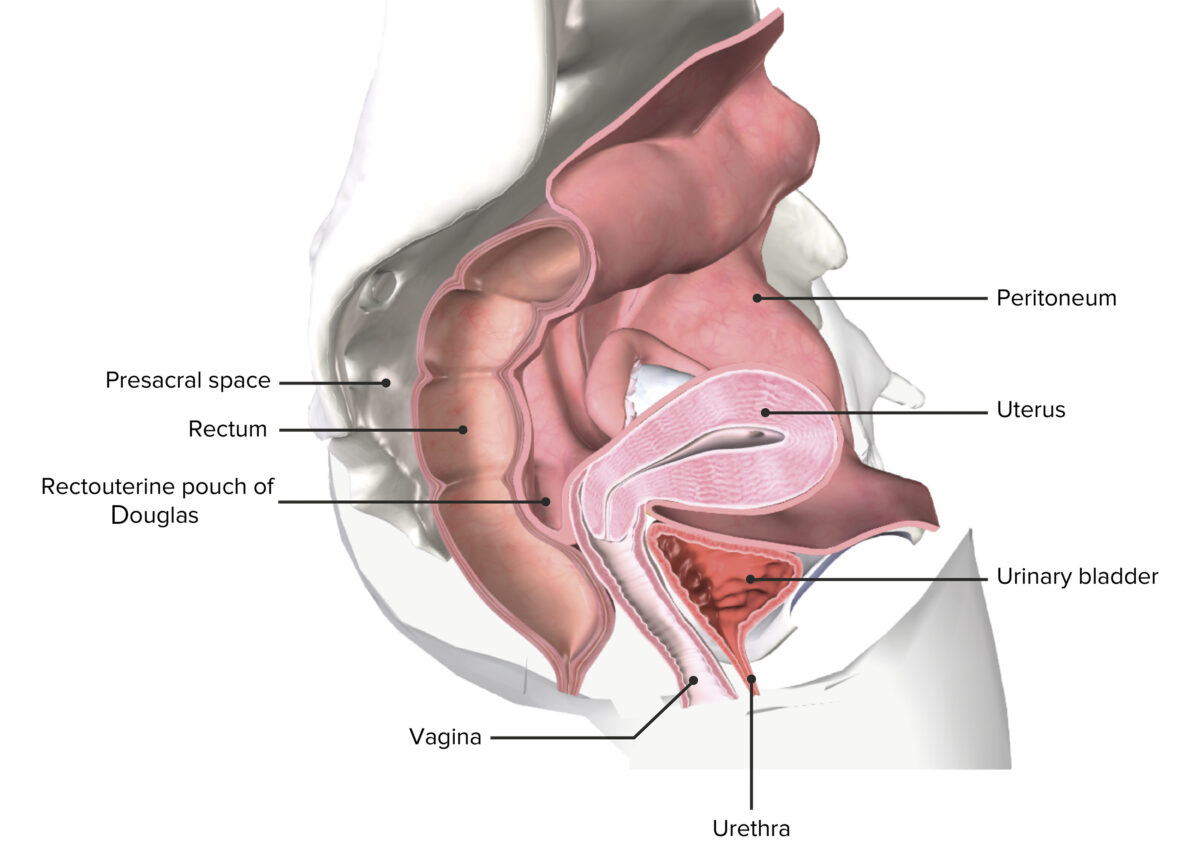
Peritoneal spaces within the female pelvis:
In the female pelvis, note the bladder’s close proximity to the anterior vaginal wall. Also note the difference in urethral length of the female urethra. This shorter length (compared to the male urethra) and proximity to the vaginal opening, increases the possibility of infection.
Image by BioDigital, edited by Lecturio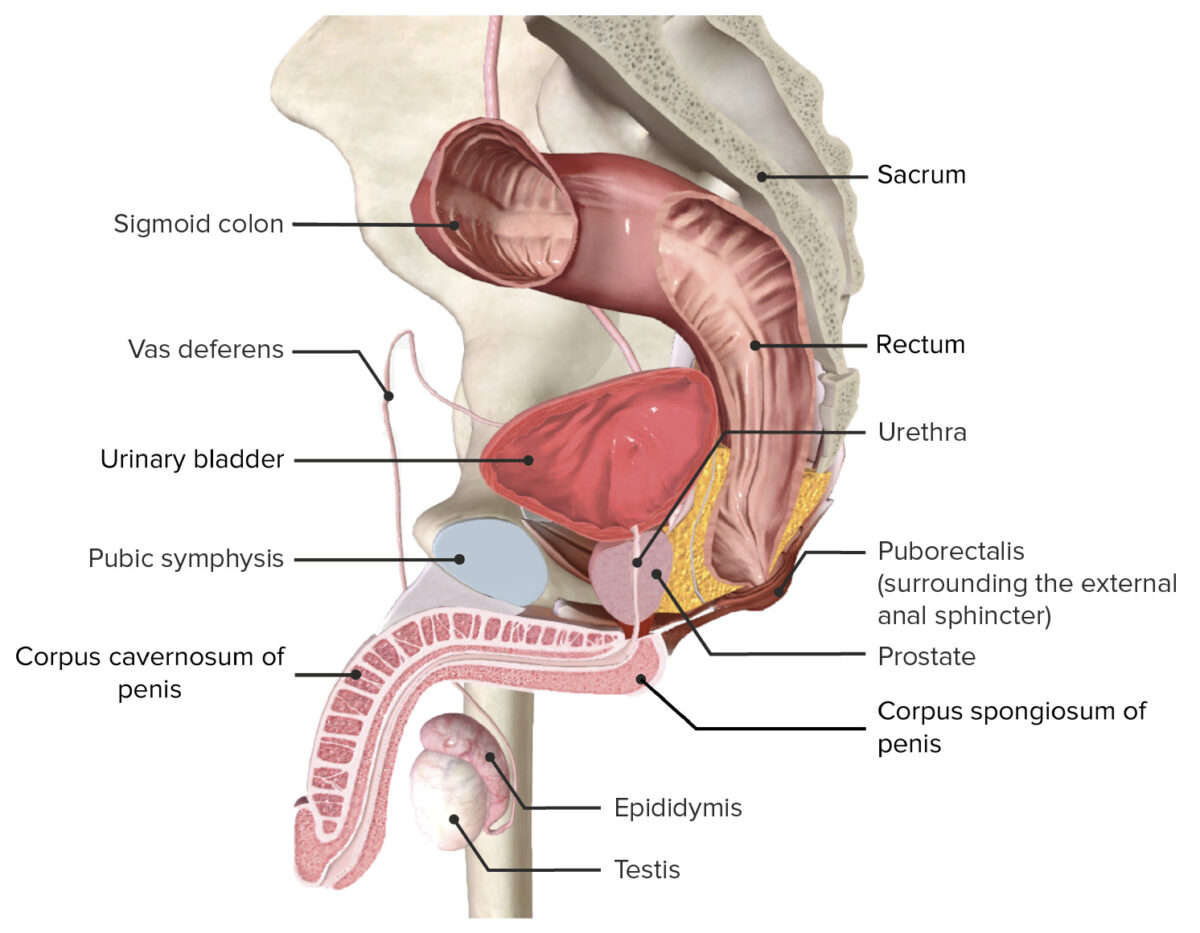
Peritoneal spaces within the male pelvis:
In the male pelvis, note the bladder’s close proximity to the rectum.
Vasculature and lymphatic drainage:
Innervation:
Microscopic description of the wall structure (from the lumen toward the outside):
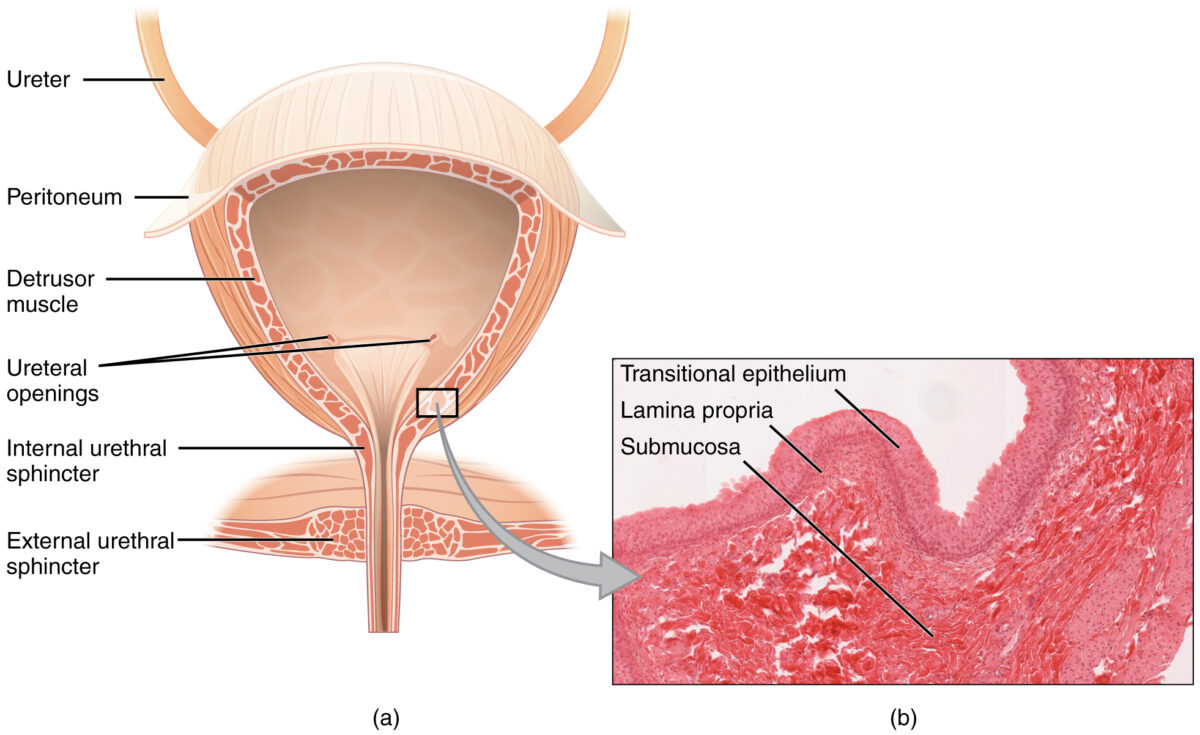
Coronal cross section of the bladder:
The magnified histologic section (b) illustrates the innermost transitional epithelium, lamina propria, and submucosa.
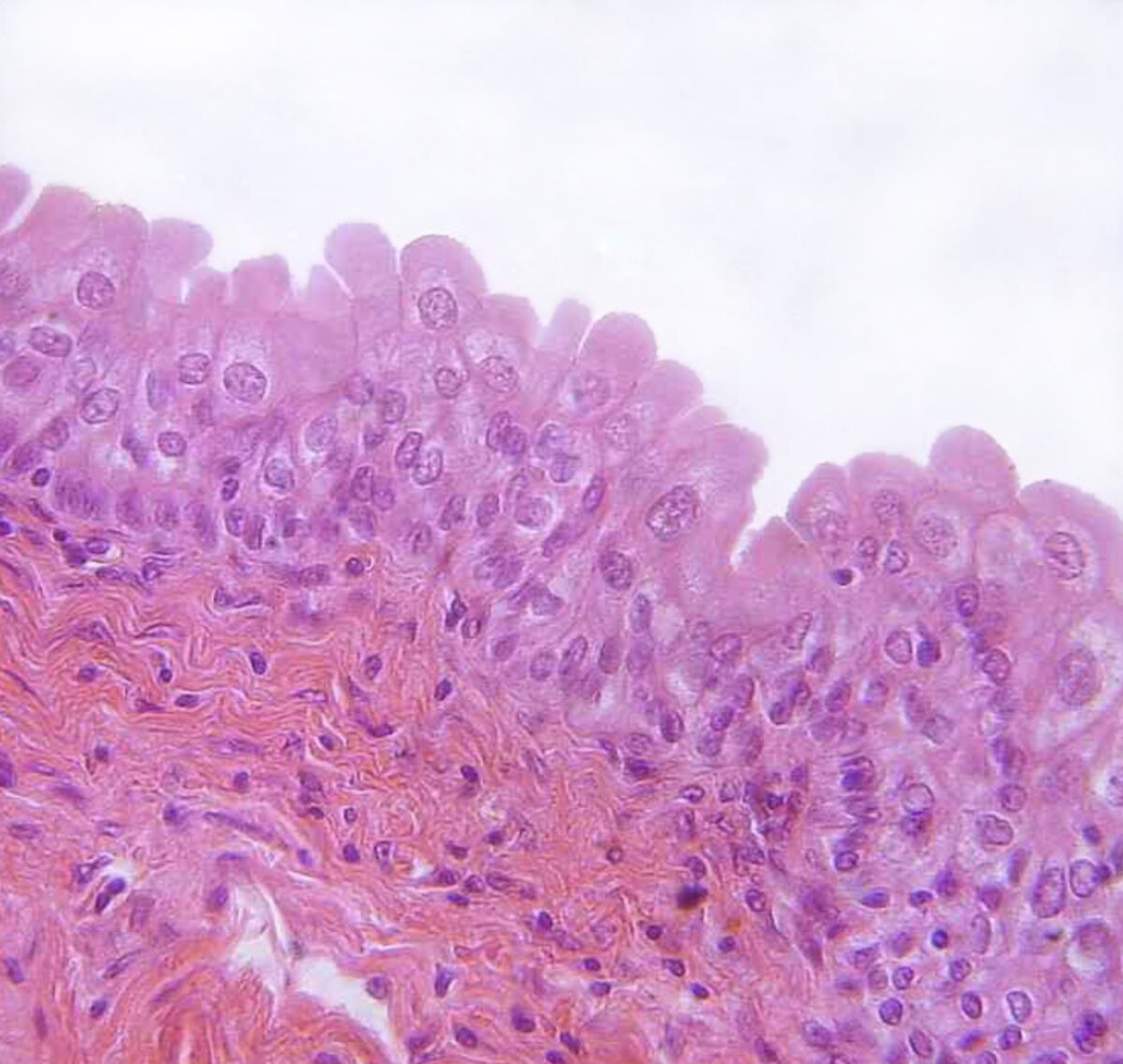
Transitional epithelium found in the urinary bladder
Image: “urinary bladder, urothelium, haemalum-eosin stain” by Polarlys. License: CC BY 2.5Description:
Structure segments:
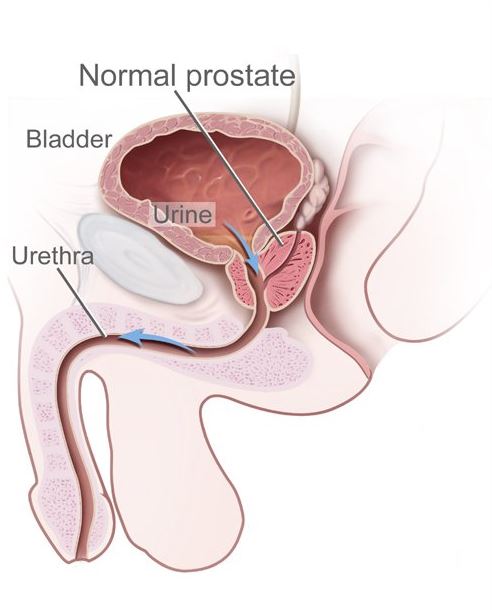
The male urethra extends from the internal urethral orifice in the bladder neck to the external urethral orifice of the penile glans and receives the ejaculatory ducts and the prostatic ducts.
Image: “Benign prostatic hyperplasia” by Unknown Illustrator. License: Public Domain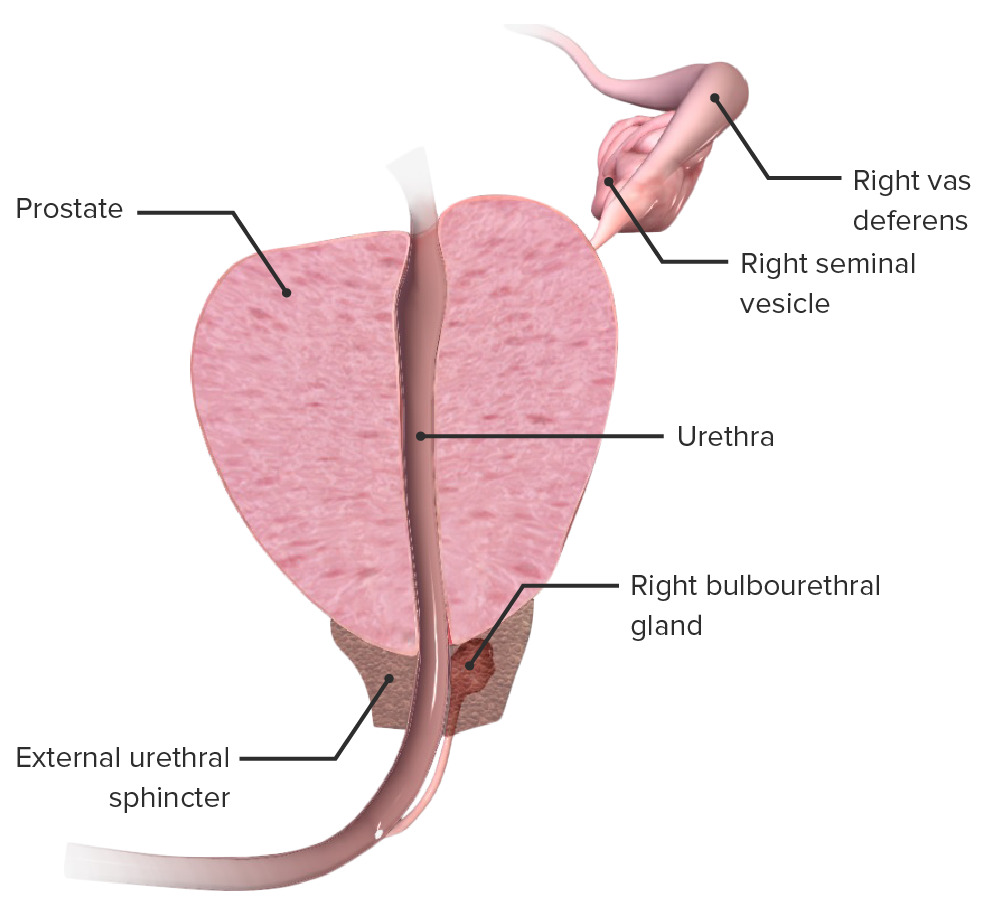
Cross section of the prostate demonstrating its relation to the prostatic urethra, urethral sphincter, seminal vesicles and bulbourethral gland
Image by BioDigital, edited by LecturioNeurovasculature and lymphatic drainage:
Histology:
Description:
Parts:
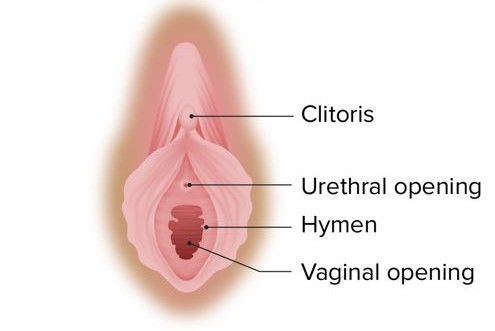
Female urethral opening, in relation to the vaginal area
Image by Lecturio.Neurovasculature and lymphatic drainage:
Histology:
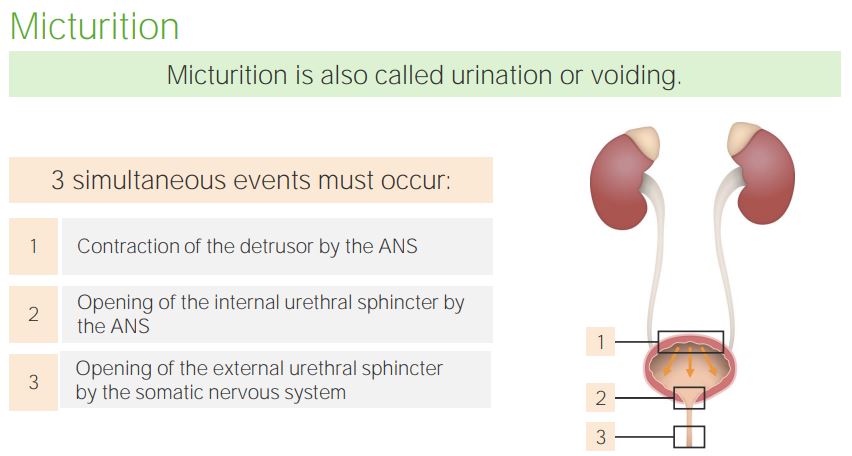
Events of micturition involves:
Detrusor muscle contraction (ANS, particularly the parasympathetic system), opening of the internal urethral sphincter (sympathetic innervation) and opening of the external urethral sphincter.