Urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy obstruction refers to the blockage of the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy, which can occur anywhere in the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy. Urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy obstruction can be acute or chronic, partial or complete, and unilateral or bilateral. Urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy obstruction can cause acute or chronic kidney disease Chronic Kidney Disease Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease. The etiology of a urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy obstruction may be congenital, acquired, and/or functional. Additionally, the cause may be intrinsic (e.g., kidney stones Kidney stones Nephrolithiasis is the formation of a stone, or calculus, anywhere along the urinary tract caused by precipitations of solutes in the urine. The most common type of kidney stone is the calcium oxalate stone, but other types include calcium phosphate, struvite (ammonium magnesium phosphate), uric acid, and cystine stones. Nephrolithiasis, transitional cell carcinoma, blood clots) or extrinsic (e.g., uterine leiomyomata). Clinical presentation depends on the location, degree, and acuteness of the obstruction. Signs and symptoms can include pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, change in urine output, hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma, and increased serum creatinine. Diagnosis is made by imaging, with ultrasound being the preferred initial modality. The mainstay of treatment is to relieve the cause of obstruction with a nephrostomy tube, ureteral stent, or catheterization. Renal function prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas after the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy obstruction is relieved is dependent on the severity and duration of the obstruction.
Last updated: Mar 25, 2025
Etiology can be congenital, acquired, or functional. Urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy obstruction can occur anywhere along the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy:
| Renal | Bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess inlet | Bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess outlet | Urethra Urethra A tube that transports urine from the urinary bladder to the outside of the body in both the sexes. It also has a reproductive function in the male by providing a passage for sperm. Urinary Tract: Anatomy | |
|---|---|---|---|---|
| Congenital |
|
|
|
|
| Acquired intrinsic defects |
|
|
|
|
| Acquired extrinsic defects |
|
|
Trauma | |
| Functional defects |
|
|||
| Hemodynamic effects | Tubule effects | |
|---|---|---|
| Acute obstruction |
|
|
| Chronic obstruction |
|
|
| Release of obstruction | Slow ↑ in GFR GFR The volume of water filtered out of plasma through glomerular capillary walls into Bowman’s capsules per unit of time. It is considered to be equivalent to inulin clearance. Kidney Function Tests, which is variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables |
|
Clinical presentation depends on the location, degree, and how quickly the obstruction develops.
Symptoms can include:
Classic laboratory findings:
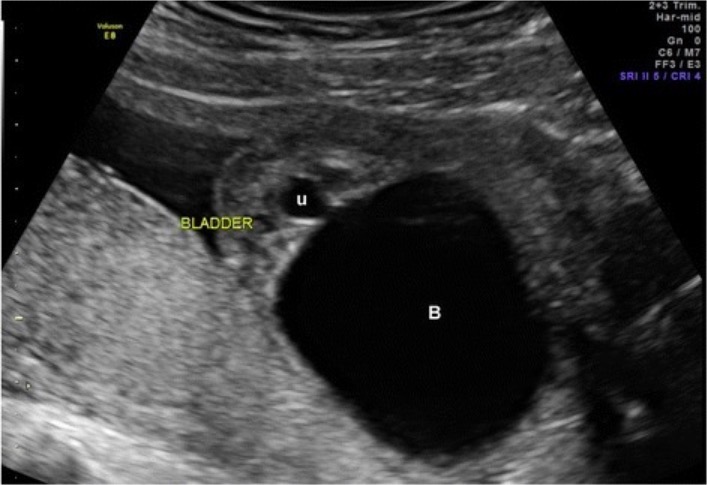
Fetal ultrasound revealing urinary tract obstruction with classic keyhole sign (B: bladder, U: urethra)
Image: “Ultrasound of fetal bladder obstruction” by St. David’s Women’s Center of Texas, Austin Maternal-Fetal Medicine, 12200 Renfert Way, G-3, Austin, Austin, TX 78758 USA. License: CC BY 4.0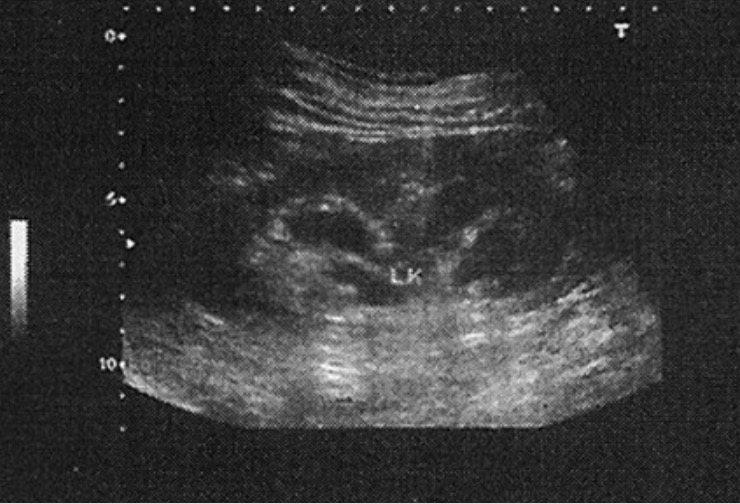
Ultrasonography revealing hydronephrosis (LK: left kidney)
Image: “Hydronephrosis” by Young Researchers Club, Tabriz Islamic Azad University, Tabriz, Iran. License: CC BY 2.0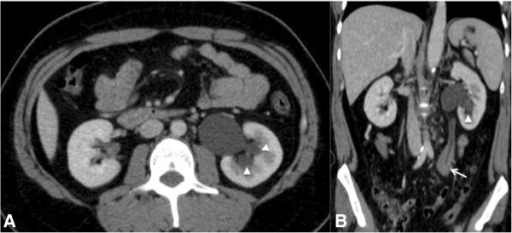
CT images of the abdomen of a 23-year-old man obtained after intravenous contrast administration:
A: Axial image showing mild hydronephrosis (arrowhead)
B: Coronal image showing a discrete delay in the concentration of intravenous contrast by the left kidney caused by a soft tissue density mass (lymphoma) involving the middle-3rd section of the left ureter (arrow)
Mainstay of treatment is to relieve the cause of obstruction.
After relief of obstruction:
With unrelieved obstruction: