Hydronephrosis is dilation of the renal collecting system as a result of the obstruction of urine outflow. Hydronephrosis can be unilateral or bilateral. Nephrolithiasis Nephrolithiasis Nephrolithiasis is the formation of a stone, or calculus, anywhere along the urinary tract caused by precipitations of solutes in the urine. The most common type of kidney stone is the calcium oxalate stone, but other types include calcium phosphate, struvite (ammonium magnesium phosphate), uric acid, and cystine stones. Nephrolithiasis is the most common cause of hydronephrosis in young adults, while prostatic hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation and neoplasm are seen in older patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Hydronephrosis is considered to be physiologic in pregnant women. Clinical presentation depends on the acuity and extent of the obstruction. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can present with flank pain Flank pain Pain emanating from below the ribs and above the ilium. Renal Cell Carcinoma, dysuria Dysuria Painful urination. It is often associated with infections of the lower urinary tract. Urinary Tract Infections (UTIs), urgency, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, a palpable abdominal mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, and hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension. Diagnosis includes imaging with ultrasonography, CT, or intravenous pyelography. Management is guided by the cause and degree of obstruction. Treatment includes pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways control, fluid replacement, and relief of the obstruction, which may require surgery, depending on the cause.
Last updated: May 17, 2024
Hydronephrosis is defined as the dilation of the renal pelvis Renal pelvis Kidneys: Anatomy and calyces due to obstruction of urine outflow.
Children:
Adults:
Clinical manifestations vary depending on the acuity of symptom onset, the degree, and the site of the obstruction. Possible presentations include:
The diagnosis of hydronephrosis is made by imaging, which also often identifies the cause. History, exam, and lab findings can help suggest the underlying etiology as well.
The following exam findings, if present, can help identify the cause of hydronephrosis:
Laboratory studies:
Diagnostic findings:
Imaging in adults:
Imaging in children:
| Grade | Characteristics |
|---|---|
| I | Renal pelvic dilation |
| II | Grade I + calyceal dilation |
| III | Grade II + thinning of the medulla |
| IV | Grade III + cortical thinning + no corticomedullary differentiation |
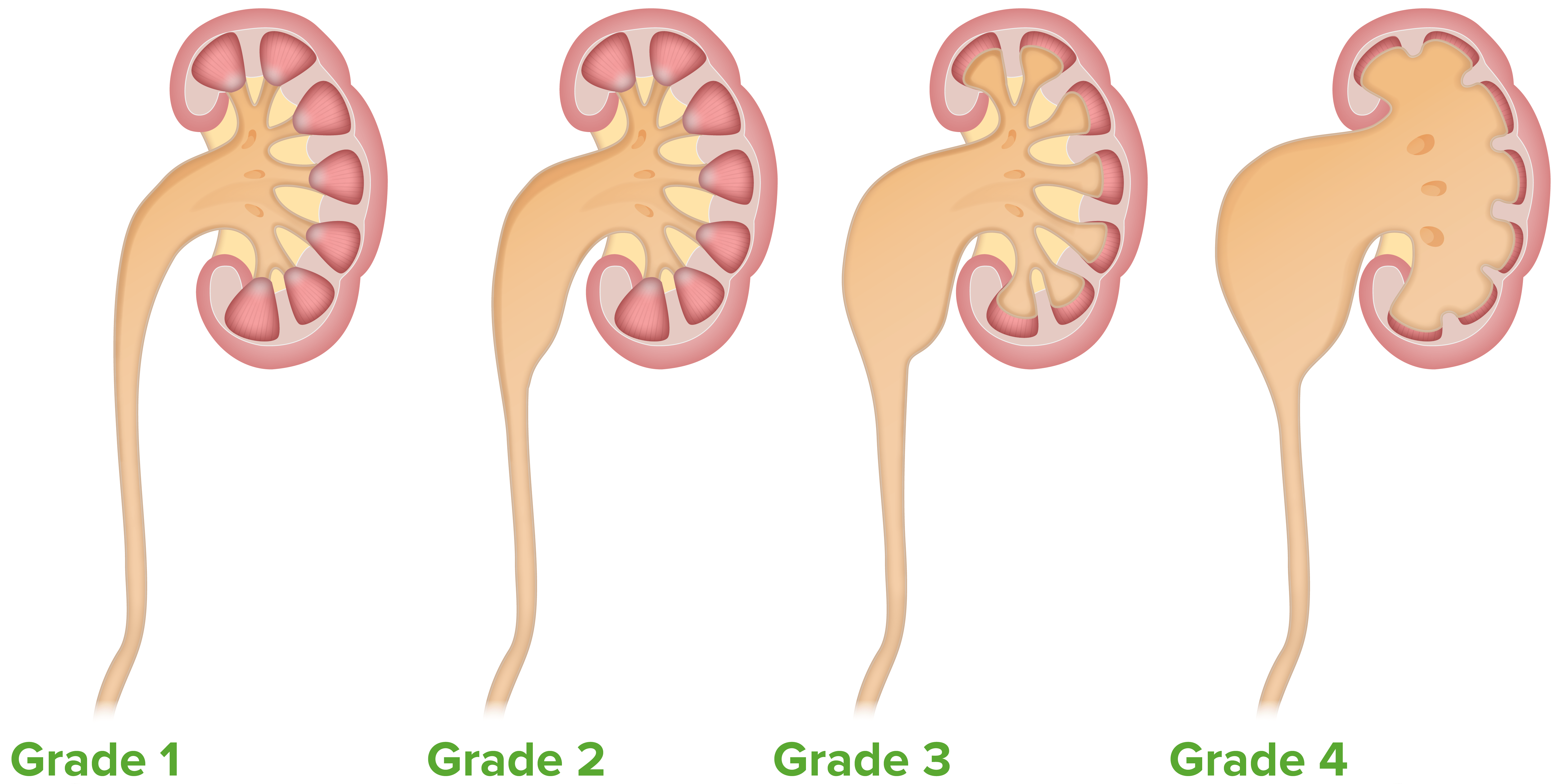
The Onen grading system of hydronephrosis
Image by Lecturio.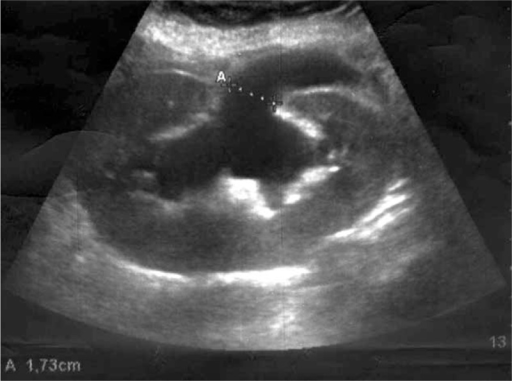
Renal ultrasound demonstrating severe hydronephrosis:
A: Calipers demonstrate dilation of the renal pelvis.
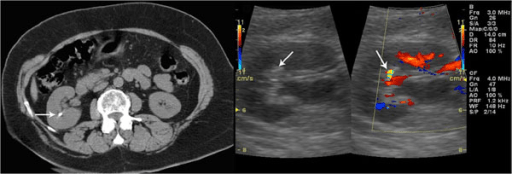
Unenhanced CT confirms the presence of a renal stone: Left: a grey-scale sonogram showing a small hyperechoic spot without posterior acoustic shadowing Right: a color Doppler sonogram showing a twinkling sign
Image: “F2: Unenhanced CT confirms the presence of renal stone. Grey-scale sonogram shows small hyperechoic spot without posterior acoustic shadowing. Color Doppler sonogram shows a twinkling sign.” by Gianfranco Vallone et al. License: CC BY 2.0
Anterograde pyelography demonstrates grade III left-sided hydronephrosis with obstruction at the ureterovesical junction.
Image: “Antegrade pyelogram of grade III hydronephrosis with obstruction at the ureterovesical junction” by Erkan Efe, Murat Bakacak, Salih Serin, Eyüp Kolus, Önder Ercan, and Sefa Resim. License: CC BY 4.0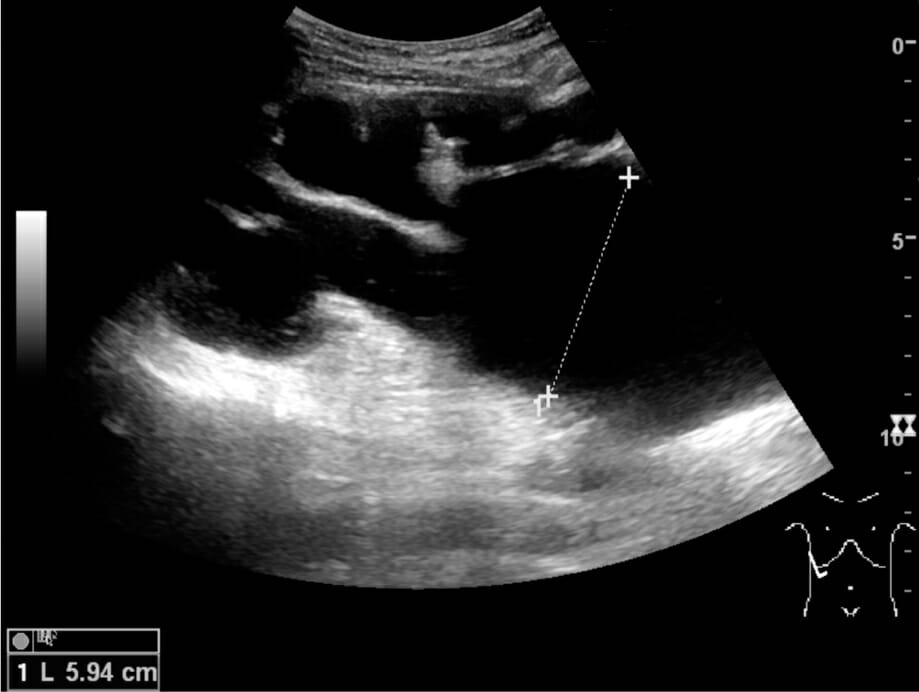
End-stage hydronephrosis with cortical thinning (grade IV): Measurement of pelvic dilatation on the US image is illustrated by ‘+’ and a dashed line.
Image: “Ultrasonography of end-stage hydronephrosis with cortical thinning” by Kristoffer Lindskov Hansen, Michael Bachmann Nielsen and Caroline Ewertsen. License: CC BY 4.0Management depends on the cause of obstruction, the degree of metabolic abnormality, and the presence of infection.
The goal is to decrease the pressure in the collecting system.