Antiadrenergic agents are drugs that block the activity of catecholamines Catecholamines A general class of ortho-dihydroxyphenylalkylamines derived from tyrosine. Adrenal Hormones, primarily norepinephrine Norepinephrine Precursor of epinephrine that is secreted by the adrenal medulla and is a widespread central and autonomic neurotransmitter. Norepinephrine is the principal transmitter of most postganglionic sympathetic fibers, and of the diffuse projection system in the brain that arises from the locus ceruleus. Receptors and Neurotransmitters of the CNS (NE). There are 2 major types of adrenergic receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors–alpha and beta receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors—and there are several subtypes of each. Antiadrenergic drugs can be classified according to their specificity for the different receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors, with the major classes including selective beta-1 receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blockers, nonselective beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers), mixed alpha- and beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers), selective alpha-1 receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blockers, and nonselective alpha-blockers. There are many beta receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors in the heart, so these medications are primarily used for cardiac indications, including MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, angina, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) (HF) (stable), and hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension (as an alternative agent). Alpha receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors are prominent in smooth muscle, especially in the vasculature. Alpha-blockers cause significant vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs and are indicated in hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension and benign Benign Fibroadenoma prostatic hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation ( BPH BPH Benign prostatic hyperplasia (bph) is a condition indicating an increase in the number of stromal and epithelial cells within the prostate gland (transition zone). Benign prostatic hyperplasia is common in men > 50 years of age and may greatly affect their quality of life. Benign Prostatic Hyperplasia). Significant adverse effects are possible.
Last updated: Apr 12, 2024
The ANS ANS The ans is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ans consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy is subdivided into the sympathetic and parasympathetic pathways. Both pathways contain 2 efferent Efferent Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology in series known as the preganglionic and postganglionic neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology.
Preganglionic neuron:
Postganglionic neuron:
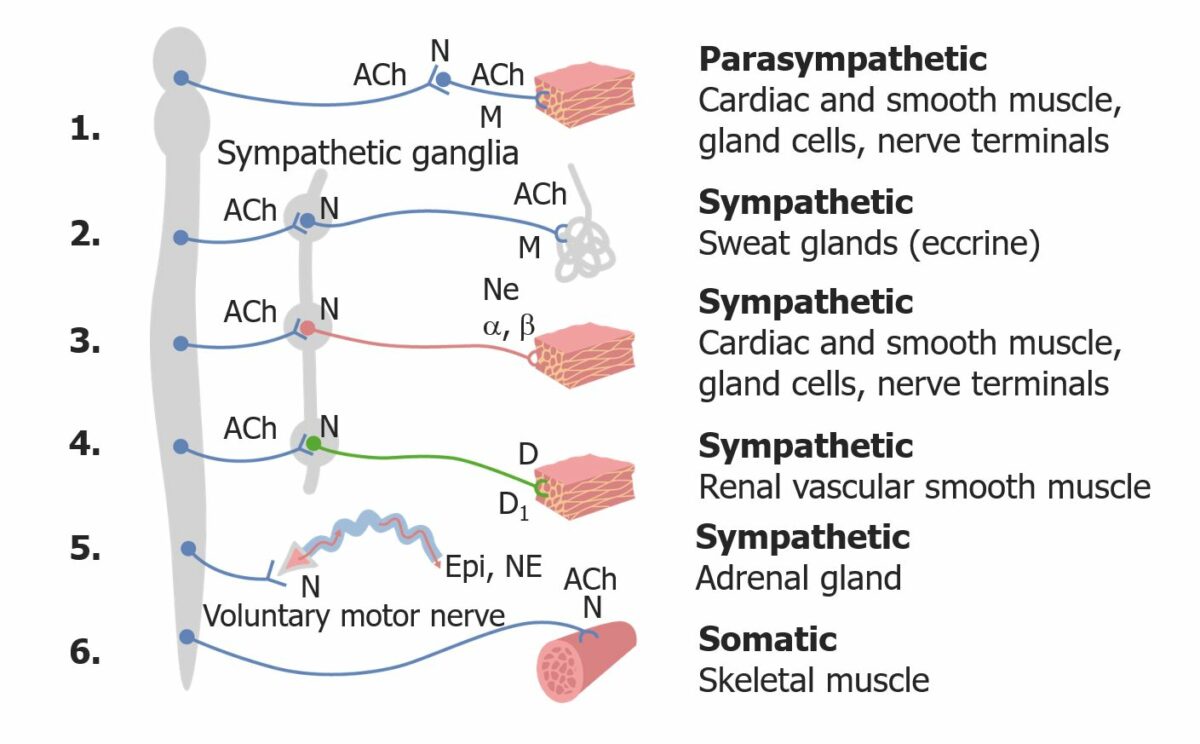
Overview of the ANS
ACh: acetylcholine
N: nicotinic receptor
M: muscarinic receptor
α and β: α and β adrenergic receptors
NE: norepinephrine
D: dopamine
D1: dopamine receptor
Epi: Epinephrine
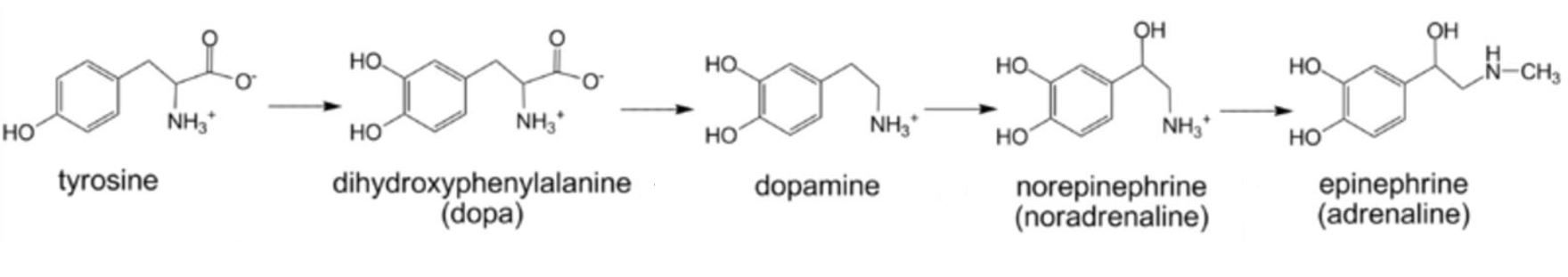
Chemical structure of the catecholamines
Image: “Catecholamine biosynthesis” by Michael Skovbo Windahl. License: CC0 1.0, cropped by Lecturio.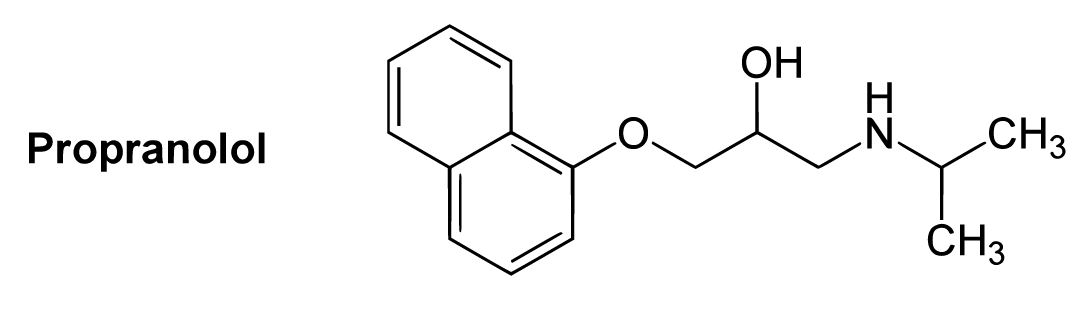
Chemical structure of propranolol
Image: “B1-selective beta blockers” by Yikrazuul. License: Public Domain, cropped by Lecturio.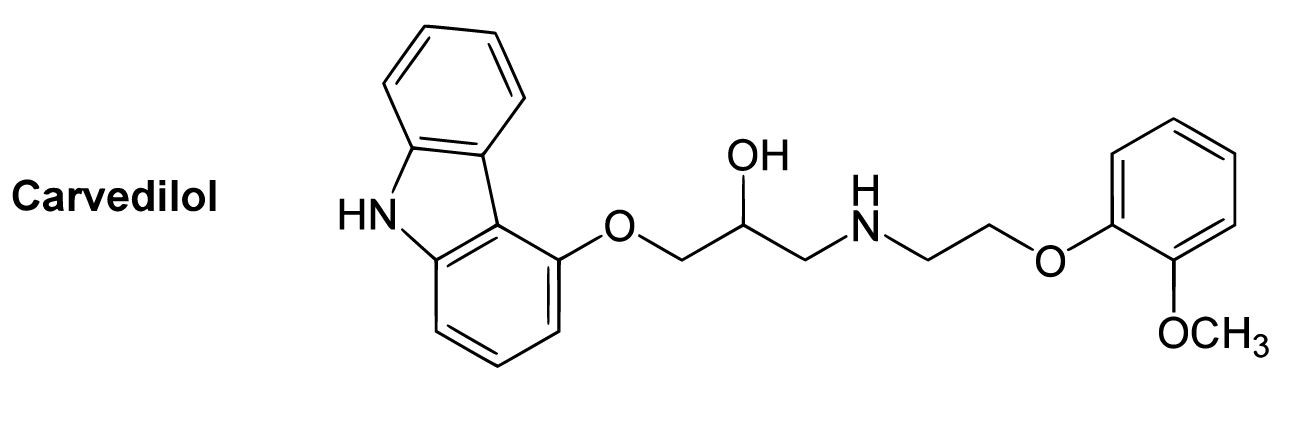
Chemical structure of carvedilol
Image: “B1-selective beta blockers” by Yikrazuul. License: Public Domain, cropped by Lecturio.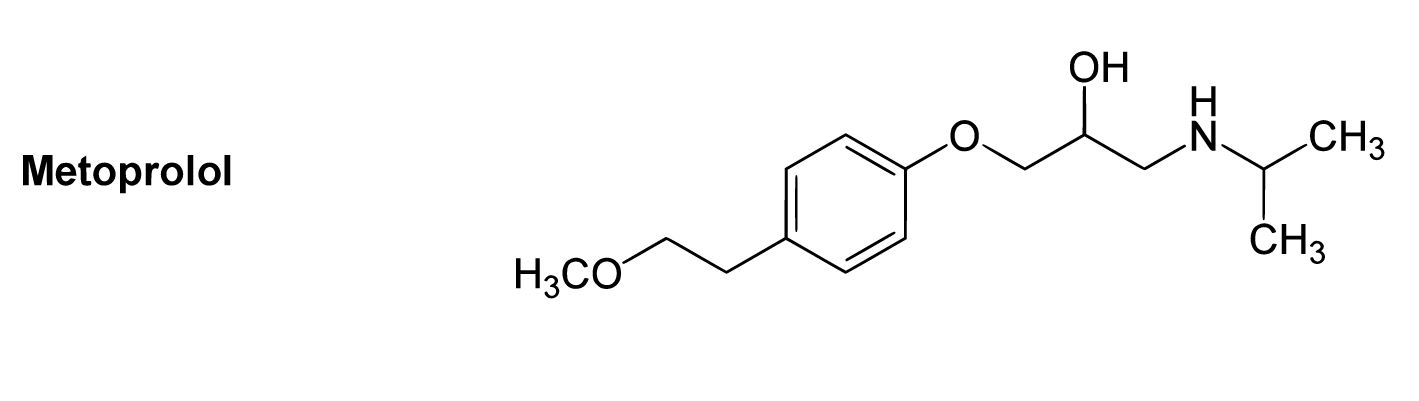
Chemical structure of metoprolol
Image: “B1-selective beta blockers” by Yikrazuul. License: Public Domain, cropped by Lecturio.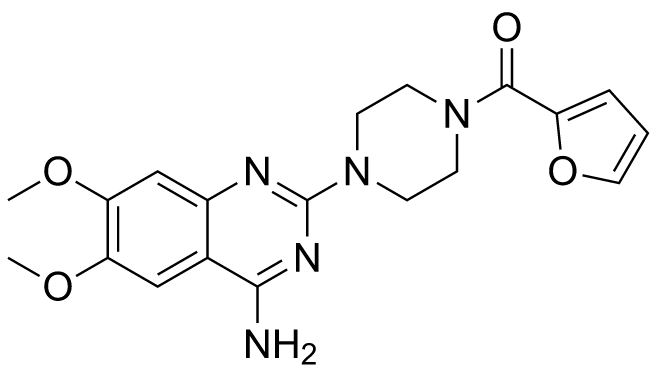
Chemical structure of prazosin
Image: “Prazosin” by Fvasconcellos. License: Public DomainAntiadrenergic drugs work by inhibiting the postganglionic adrenergic receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors. These are G-protein-coupled receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors.
Alpha receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors:
Beta receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors: beta-1, beta-2, and beta-3
Adrenergic receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors are located throughout the body and trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation a wide variety of effects. The physiologic effects of antiadrenergic agents are to block whatever the typical response is of that particular receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors.
| System | Organ | Receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors | Physiologic actions from receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors stimulation (agonism) | Physiologic effects from receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blockade (antagonism) |
|---|---|---|---|---|
| Eye | Iris radial muscle | α1 | Contraction → pupil Pupil The pupil is the space within the eye that permits light to project onto the retina. Anatomically located in front of the lens, the pupil’s size is controlled by the surrounding iris. The pupil provides insight into the function of the central and autonomic nervous systems. Pupil: Physiology and Abnormalities dilation | Relaxation → pupil Pupil The pupil is the space within the eye that permits light to project onto the retina. Anatomically located in front of the lens, the pupil’s size is controlled by the surrounding iris. The pupil provides insight into the function of the central and autonomic nervous systems. Pupil: Physiology and Abnormalities constriction |
| Ciliary muscle | β | Relaxes → flattens lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy → better for long-range focus | ↓ Relaxation → rounder lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy → short range focus | |
| Ciliary epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology | β | ↑ Production of aqueous humor Humor Defense Mechanisms | ↓ Secretion Secretion Coagulation Studies of aqueous humor Humor Defense Mechanisms → ↓ IOP | |
| Cardiovascular system | SA | β1, β2 | Acceleration (↑ HR) | ↓ HR |
| Ectopic pacemakers | β1, β2 | Acceleration (↑ HR) | ↓ HR | |
| Contractility of atria and ventricles | β1, β2 | ↑ Contractility | ↓ Contractility | |
| Vascular wall smooth muscle | α1 | Vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure | Vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs → may cause orthostatic hypotension Orthostatic hypotension A significant drop in blood pressure after assuming a standing position. Orthostatic hypotension is a finding, and defined as a 20-mm hg decrease in systolic pressure or a 10-mm hg decrease in diastolic pressure 3 minutes after the person has risen from supine to standing. Symptoms generally include dizziness, blurred vision, and syncope. Hypotension and reflex tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children | |
| β2 | Vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs | Vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure → ↑ peripheral resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing | ||
| Pulmonary smooth muscle | Bronchiolar smooth muscle | β2 | Bronchodilation | Bronchoconstriction (especially with asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma) |
| GI tract smooth muscle | Intestinal walls | α2, β2 | Relaxation (↓ motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility) | ↑ Motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility → may lead to diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea |
| Sphincter muscles | α1 | Contracts (prevents chyme Chyme Small Intestine: Anatomy from passing through) | Sphincter relaxation Sphincter relaxation Gastrointestinal Motility → ↑ risk of heartburn Heartburn Substernal pain or burning sensation, usually associated with regurgitation of gastric juice into the esophagus. Gastroesophageal Reflux Disease (GERD) | |
| Genitourinary smooth muscle | Bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess wall | β2, β3 | Relaxes | ↓ Resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing to urine flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure |
| Urethral sphincters | α1 | Contracts | ↓ Resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing to urine flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure → ↑ risk of incontinence | |
| Pregnant uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy | α | Uterine contraction | Uterine relaxation | |
| β2 | Uterine relaxation | Uterine contractions → labor/ preterm labor Preterm labor Preterm labor refers to regular uterine contractions leading to cervical change prior to 37 weeks of gestation; preterm birth refers to birth prior to 37 weeks of gestation. Preterm birth may be spontaneous due to preterm labor, preterm prelabor rupture of membranes (PPROM), or cervical insufficiency. Preterm Labor and Birth | ||
| Penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy and seminal vesicles Vesicles Female Genitourinary Examination | α | Ejaculation | Difficulty with ejaculation | |
| Metabolic functions | Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy | α, β2 | Gluconeogenesis Gluconeogenesis Gluconeogenesis is the process of making glucose from noncarbohydrate precursors. This metabolic pathway is more than just a reversal of glycolysis. Gluconeogenesis provides the body with glucose not obtained from food, such as during a fasting period. The production of glucose is critical for organs and cells that cannot use fat for fuel. Gluconeogenesis, glycogenolysis Glycogenolysis The release of glucose from glycogen by glycogen phosphorylase (phosphorolysis). The released glucose-1-phosphate is then converted to glucose-6-phosphate by phosphoglucomutase before entering glycolysis. Glycogenolysis is stimulated by glucagon or epinephrine via the activation of phosphorylase kinase. Glycogen Metabolism | ↓ Glycogenolysis Glycogenolysis The release of glucose from glycogen by glycogen phosphorylase (phosphorolysis). The released glucose-1-phosphate is then converted to glucose-6-phosphate by phosphoglucomutase before entering glycolysis. Glycogenolysis is stimulated by glucagon or epinephrine via the activation of phosphorylase kinase. Glycogen Metabolism → may impair recovery from hypoglycemia Hypoglycemia Hypoglycemia is an emergency condition defined as a serum glucose level ≤ 70 mg/dL (≤ 3.9 mmol/L) in diabetic patients. In nondiabetic patients, there is no specific or defined limit for normal serum glucose levels, and hypoglycemia is defined mainly by its clinical features. Hypoglycemia |
| Adipose tissue Adipose tissue Adipose tissue is a specialized type of connective tissue that has both structural and highly complex metabolic functions, including energy storage, glucose homeostasis, and a multitude of endocrine capabilities. There are three types of adipose tissue, white adipose tissue, brown adipose tissue, and beige or “brite” adipose tissue, which is a transitional form. Adipose Tissue: Histology | β3 | Lipolysis Lipolysis The metabolic process of breaking down lipids to release free fatty acids, the major oxidative fuel for the body. Lipolysis may involve dietary lipids in the digestive tract, circulating lipids in the blood, and stored lipids in the adipose tissue or the liver. A number of enzymes are involved in such lipid hydrolysis, such as lipase and lipoprotein lipase from various tissues. Metabolic Dysfunction-associated Steatotic Liver Disease (MASLD) | Inhibition of lipolysis Lipolysis The metabolic process of breaking down lipids to release free fatty acids, the major oxidative fuel for the body. Lipolysis may involve dietary lipids in the digestive tract, circulating lipids in the blood, and stored lipids in the adipose tissue or the liver. A number of enzymes are involved in such lipid hydrolysis, such as lipase and lipoprotein lipase from various tissues. Metabolic Dysfunction-associated Steatotic Liver Disease (MASLD) | |
| Kidney | β1 | Renin Renin A highly specific (leu-leu) endopeptidase that generates angiotensin I from its precursor angiotensinogen, leading to a cascade of reactions which elevate blood pressure and increase sodium retention by the kidney in the renin-angiotensin system. Renal Sodium and Water Regulation release | Suppression Suppression Defense Mechanisms of renin Renin A highly specific (leu-leu) endopeptidase that generates angiotensin I from its precursor angiotensinogen, leading to a cascade of reactions which elevate blood pressure and increase sodium retention by the kidney in the renin-angiotensin system. Renal Sodium and Water Regulation release |
These drugs have inhibitory effects at both the beta and alpha-1 receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors
Differences in pharmacokinetics Pharmacokinetics Pharmacokinetics is the science that analyzes how the human body interacts with a drug. Pharmacokinetics examines how the drug is absorbed, distributed, metabolized, and excreted by the body. Pharmacokinetics and Pharmacodynamics can help determine which medication in a particular class is optimal for a given clinical scenario.
| Drug | Absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption | Distribution | Metabolism | Excretion |
|---|---|---|---|---|
| Prazosin (selective α1-blocker) | Onset: 2‒4 hrs HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome |
|
Extensive hepatic via demethylation and conjugation Conjugation A parasexual process in bacteria; algae; fungi; and ciliate eukaryota for achieving exchange of chromosome material during fusion of two cells. In bacteria, this is a unidirectional transfer of genetic material; in protozoa it is a bi-directional exchange. In algae and fungi, it is a form of sexual reproduction, with the union of male and female gametes. Bacteriology |
|
| Phentolamine (nonselective α-blocker |
|
Widely distributed | Hepatic |
|
| Propranolol (nonselective β-blocker) |
|
|
Extensive 1st-pass hepatic metabolism |
|
| Atenolol Atenolol A cardioselective beta-1 adrenergic blocker possessing properties and potency similar to propranolol, but without a negative inotropic effect. Class 2 Antiarrhythmic Drugs (Beta Blockers) (β1-selective β-blocker) |
|
|
Minimal hepatic metabolism |
|
| Metoprolol (β1-selective β-blocker) |
|
|
Extensive 1st-pass hepatic metabolism |
|
| Carvedilol Carvedilol A carbazole and propanol derivative that acts as a non-cardioselective beta blocker and vasodilator. It has blocking activity for alpha 1 adrenergic receptors and, at higher doses, may function as a blocker of calcium channels; it also has antioxidant properties. Carvedilol is used in the treatment of hypertension; angina pectoris; and heart failure. It can also reduce the risk of death following myocardial infarction. Class 2 Antiarrhythmic Drugs (Beta Blockers) (mixed α and β blockade) |
|
|
Extensive 1st-pass hepatic metabolism |
|
Drug interactions are also important for several medications within this class.
While Alpha-2 antagonists have few clinical uses, alpha-1 and nonselective alpha antagonists are used for their ability to cause vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs and smooth muscle relaxation. They are frequently used in the treatment of:
Beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) have a variety of indications. They are frequently used for their negative inotropic and chronotropic effects in the heart.
Antiadrenergic medications must be used with caution and titrated slowly to avoid side effects.
| Drug | Adverse effects | Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation |
|---|---|---|
| Beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) |
|
|
| Alpha-1 blockers (prazosin) |
|
Known hypersensitivity to the drug |
| Nonselective alpha antagonists (phenoxybenzamine, phentolamine) |
|
|
Although beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) are generally safe, overdose can produce symptoms of toxicity Toxicity Dosage Calculation, typically within 2 hours (almost always within 6). Symptoms include:
| Medication | Mechanism | Physiologic effects | Indication |
|---|---|---|---|
| Metoprolol | Selective β1-blocker |
|
|
| Propranolol | Nonselective β-blocker |
|
|
| Carvedilol Carvedilol A carbazole and propanol derivative that acts as a non-cardioselective beta blocker and vasodilator. It has blocking activity for alpha 1 adrenergic receptors and, at higher doses, may function as a blocker of calcium channels; it also has antioxidant properties. Carvedilol is used in the treatment of hypertension; angina pectoris; and heart failure. It can also reduce the risk of death following myocardial infarction. Class 2 Antiarrhythmic Drugs (Beta Blockers) | Nonselective α- and β-blocker |
|
|
| Prazosin | Selective α1-blocker |
|
|
| Phentolamine | Nonselective α-adrenergic antagonist |
|
|