Preterm labor refers to regular Regular Insulin uterine contractions leading to cervical change prior to 37 weeks of gestation; preterm birth refers to birth prior to 37 weeks of gestation. Preterm birth may be spontaneous due to preterm labor, preterm prelabor rupture of membranes Prelabor Rupture of Membranes Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, refers to the rupture of the amniotic sac before the onset of labor. Prelabor rupture of membranes may occur in term or preterm pregnancies. Prelabor Rupture of Membranes (PPROM), or cervical insufficiency. Preterm birth may also be initiated by the provider for a variety of maternal or fetal indications. Diagnosis involves assessments to detect cervical change and monitoring for regular Regular Insulin uterine contractions. Management depends on gestational age Gestational age The age of the conceptus, beginning from the time of fertilization. In clinical obstetrics, the gestational age is often estimated as the time from the last day of the last menstruation which is about 2 weeks before ovulation and fertilization. Pregnancy: Diagnosis, Physiology, and Care, but typically includes administration of corticosteroids Corticosteroids Chorioretinitis (to improve fetal lung maturity), magnesium sulfate Magnesium Sulfate A small colorless crystal used as an anticonvulsant, a cathartic, and an electrolyte replenisher in the treatment of pre-eclampsia and eclampsia. It causes direct inhibition of action potentials in myometrial muscle cells. Excitation and contraction are uncoupled, which decreases the frequency and force of contractions. Laxatives (for fetal neuroprotection against cerebral palsy Palsy paralysis of an area of the body, thus incapable of voluntary movement Cranial Nerve Palsies), group B streptococcus Group B Streptococcus Meningitis in Children ( GBS GBS An acute inflammatory autoimmune neuritis caused by t cell- mediated cellular immune response directed towards peripheral myelin. Demyelination occurs in peripheral nerves and nerve roots. The process is often preceded by a viral or bacterial infection, surgery, immunization, lymphoma, or exposure to toxins. Common clinical manifestations include progressive weakness, loss of sensation, and loss of deep tendon reflexes. Weakness of respiratory muscles and autonomic dysfunction may occur. Polyneuropathy) prophylaxis Prophylaxis Cephalosporins, and 48 hours of tocolytics to help patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship complete a full course of steroids Steroids A group of polycyclic compounds closely related biochemically to terpenes. They include cholesterol, numerous hormones, precursors of certain vitamins, bile acids, alcohols (sterols), and certain natural drugs and poisons. Steroids have a common nucleus, a fused, reduced 17-carbon atom ring system, cyclopentanoperhydrophenanthrene. Most steroids also have two methyl groups and an aliphatic side-chain attached to the nucleus. Benign Liver Tumors.
Last updated: Mar 29, 2023
Preterm labor is defined as regular Regular Insulin uterine contractions that lead to cervical change in dilation and/or effacement prior to 37 weeks of gestation.
Preterm birth is defined as birth at a gestational age Gestational age The age of the conceptus, beginning from the time of fertilization. In clinical obstetrics, the gestational age is often estimated as the time from the last day of the last menstruation which is about 2 weeks before ovulation and fertilization. Pregnancy: Diagnosis, Physiology, and Care of 20–37 weeks.
Preterm labor:
Preterm birth:
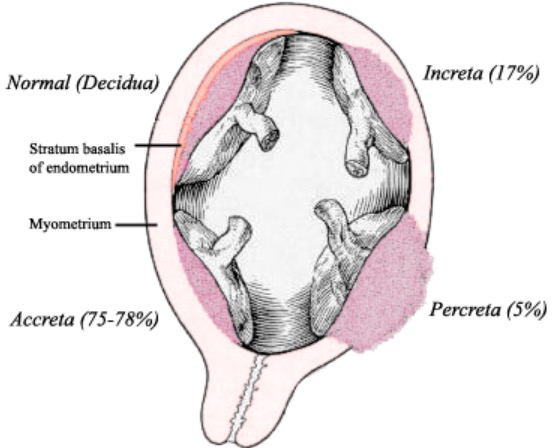
Placenta accreta:
A known etiology for indicated preterm birth, placenta accreta describes a placenta invading the myometrium to differing depths.
Because preterm labor is a major etiology of preterm birth, all risk factors for preterm labor are also risk factors for spontaneous preterm birth.
Common final pathway for initiating preterm labor:
Primary pathways (4) leading to the common final pathway:
All pathways leading to preterm labor (above) can progress to preterm birth.
Preterm birth may also be caused by cervical insufficiency:
Pregnant women < 37 weeks’ gestational age Gestational age The age of the conceptus, beginning from the time of fertilization. In clinical obstetrics, the gestational age is often estimated as the time from the last day of the last menstruation which is about 2 weeks before ovulation and fertilization. Pregnancy: Diagnosis, Physiology, and Care who present with:
The key to diagnosing preterm labor is to determine whether cervical change is occurring, and if regular Regular Insulin contractions are causing those changes. The cervical length is also important in helping to predict preterm birth regardless of contractions.
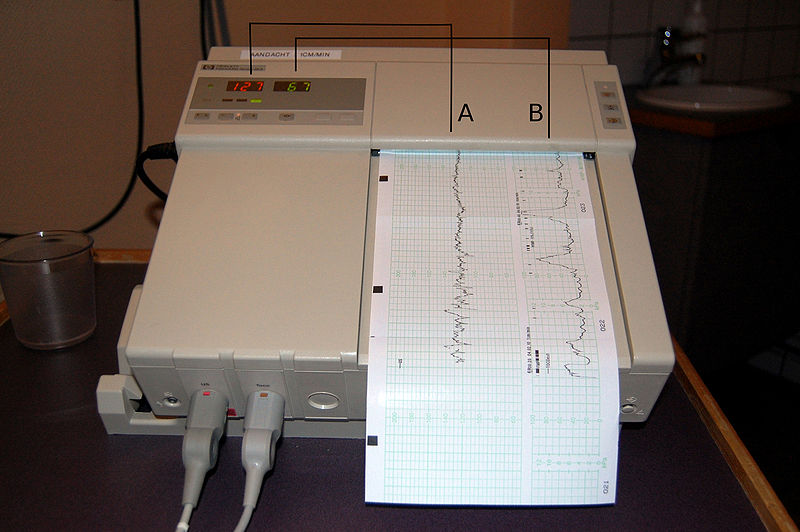
Fetal monitoring with tocometry:
A: Recording of the fetal heart rate determined by external ultrasound
B: Recording of the uterine contractions measured by an external pressure transducer
Values are recorded continually over time.
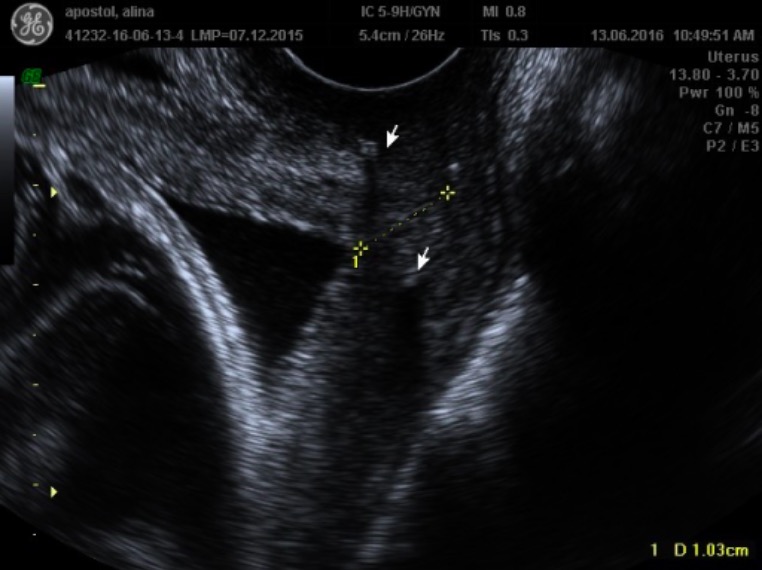
A transvaginal ultrasound image demonstrating a shortened cervix of 1.0 cm (dotted yellow line):
Arrows indicate the hyperechoic cerclage suture.
Diagnosing preterm labor requires uterine contractions plus cervical change:
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship diagnosed with preterm labor should be hospitalized for observation of progressing labor and for treatment.
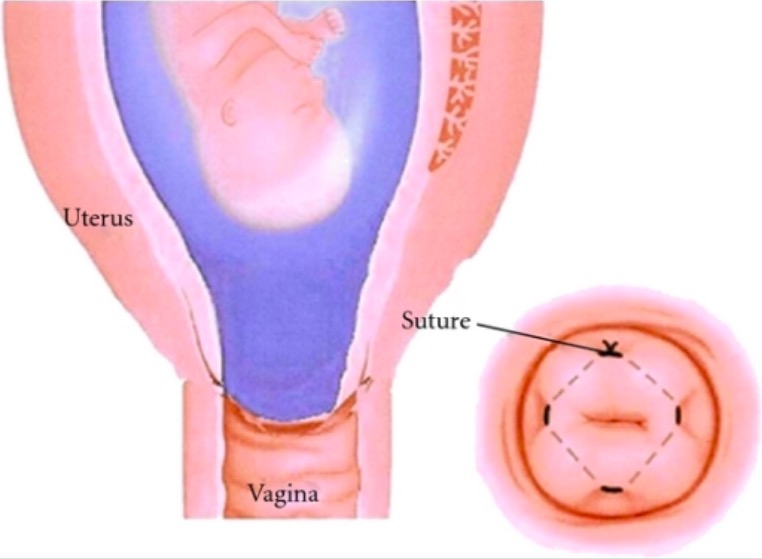
Cervical cerclage:
The larger image shows a dilated cervix with membranes visible on SSE. A cerclage suture is placed circumferentially in a purse-string fashion around the cervix.