Malaria is an infectious parasitic disease affecting humans and other animals Animals Unicellular or multicellular, heterotrophic organisms, that have sensation and the power of voluntary movement. Under the older five kingdom paradigm, animalia was one of the kingdoms. Under the modern three domain model, animalia represents one of the many groups in the domain eukaryota. Cell Types: Eukaryotic versus Prokaryotic. Most commonly transmitted via the bite of an infected female Anopheles mosquito, malaria is caused by single-celled microorganisms of the Plasmodium Plasmodium A genus of protozoa that comprise the malaria parasites of mammals. Four species infect humans (although occasional infections with primate malarias may occur). These are plasmodium falciparum; plasmodium malariae; plasmodium ovale, and plasmodium vivax. Species causing infection in vertebrates other than man include: plasmodium berghei; plasmodium chabaudi; p. Vinckei, and plasmodium yoelii in rodents; p. Brasilianum, plasmodium cynomolgi; and plasmodium knowlesi in monkeys; and plasmodium gallinaceum in chickens. Antimalarial Drugs genus. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, chills Chills The sudden sensation of being cold. It may be accompanied by shivering. Fever, myalgia Myalgia Painful sensation in the muscles. Ion Channel Myopathy, headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, and diaphoresis after a history of exposure in an area endemic to malaria, which is often cyclical. Prophylaxis Prophylaxis Cephalosporins is of utmost importance. Treatment with oral medications is available, but malaria can be severe and fatal without a timely diagnosis, especially in young children.
Last updated: Sep 19, 2022
Malaria is a parasitic disease caused by unicellular Unicellular Cell Types: Eukaryotic versus Prokaryotic parasites of the Plasmodium Plasmodium A genus of protozoa that comprise the malaria parasites of mammals. Four species infect humans (although occasional infections with primate malarias may occur). These are plasmodium falciparum; plasmodium malariae; plasmodium ovale, and plasmodium vivax. Species causing infection in vertebrates other than man include: plasmodium berghei; plasmodium chabaudi; p. Vinckei, and plasmodium yoelii in rodents; p. Brasilianum, plasmodium cynomolgi; and plasmodium knowlesi in monkeys; and plasmodium gallinaceum in chickens. Antimalarial Drugs genus and transmitted by mosquitoes of the Anopheles genus.
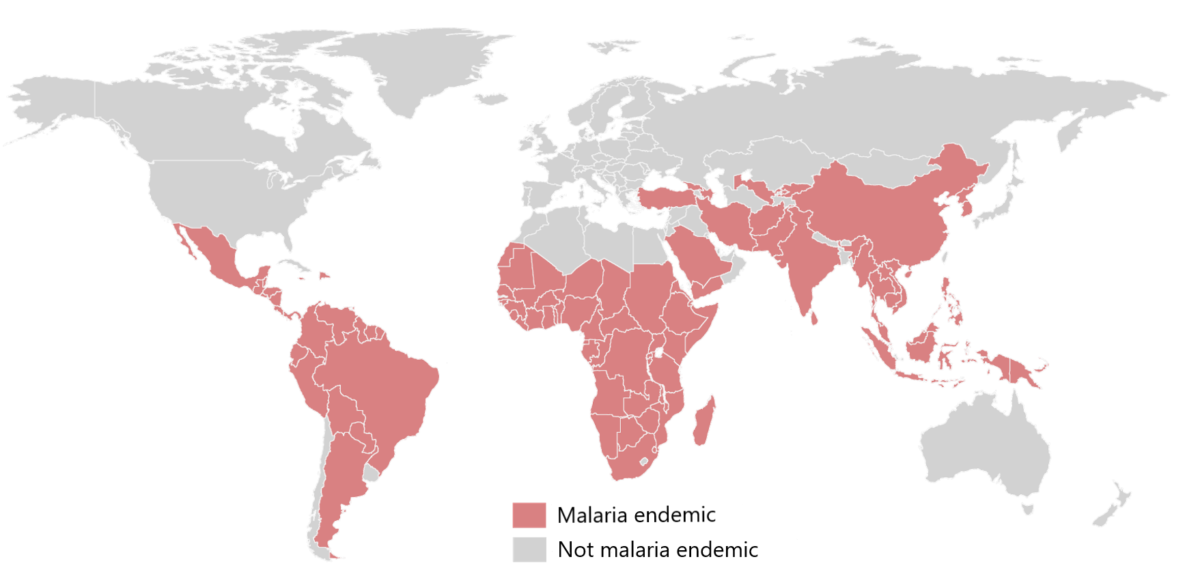
Worldwide endemic distribution of malaria
Image by Lecturio. License: CC BY-NC-SA 4.0
Anopheles stephensi mosquito is obtaining a blood meal from a human.
Image: “Anopheles stephensi” by Jim Gathany. License: Public DomainPlasmodium Plasmodium A genus of protozoa that comprise the malaria parasites of mammals. Four species infect humans (although occasional infections with primate malarias may occur). These are plasmodium falciparum; plasmodium malariae; plasmodium ovale, and plasmodium vivax. Species causing infection in vertebrates other than man include: plasmodium berghei; plasmodium chabaudi; p. Vinckei, and plasmodium yoelii in rodents; p. Brasilianum, plasmodium cynomolgi; and plasmodium knowlesi in monkeys; and plasmodium gallinaceum in chickens. Antimalarial Drugs is a genus of unicellular Unicellular Cell Types: Eukaryotic versus Prokaryotic eukaryotes, which are obligate parasites of vertebrates and insects.
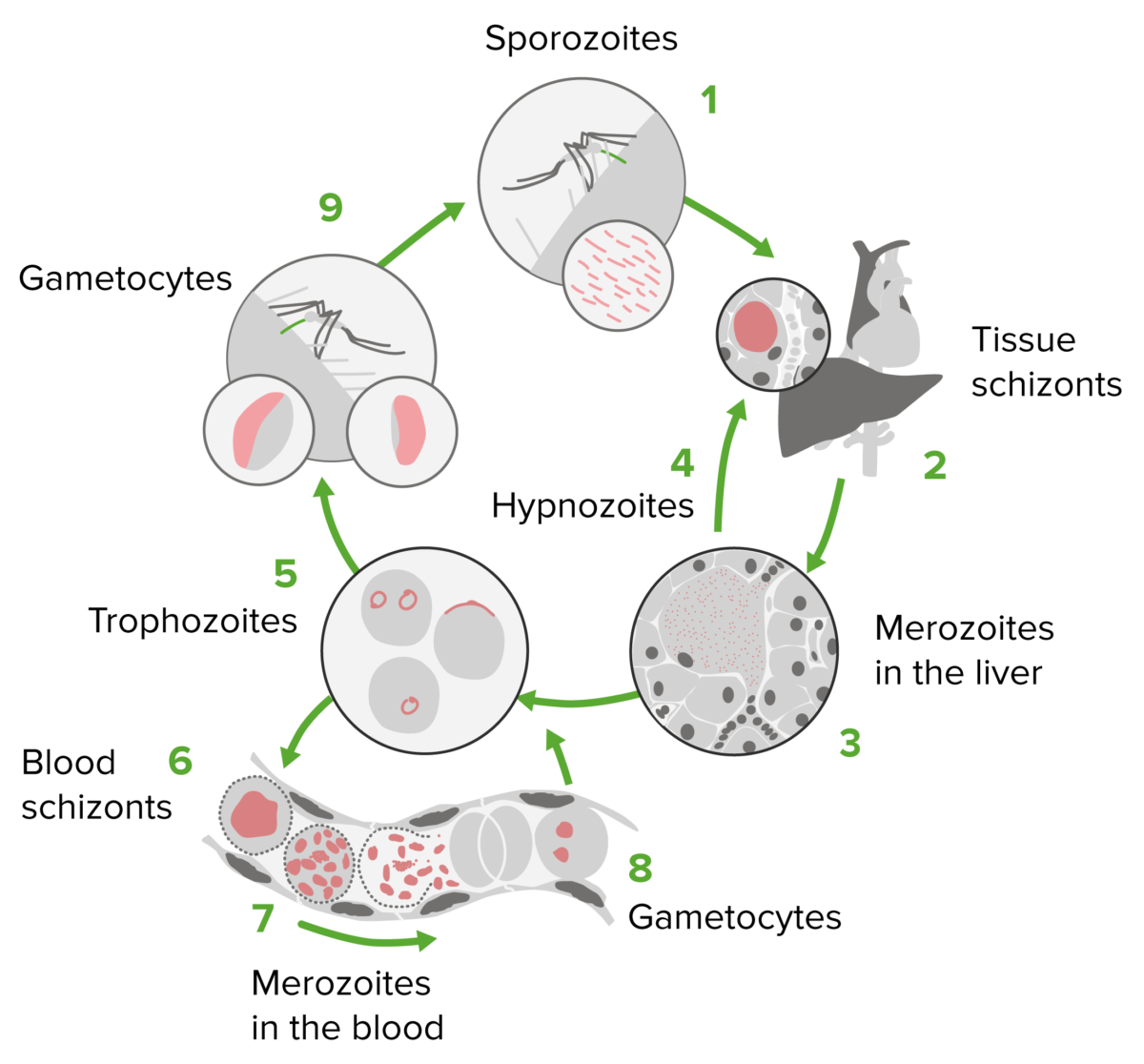
Plasmodium life cycle
Image by Lecturio. License: CC BY-NC-SA 4.0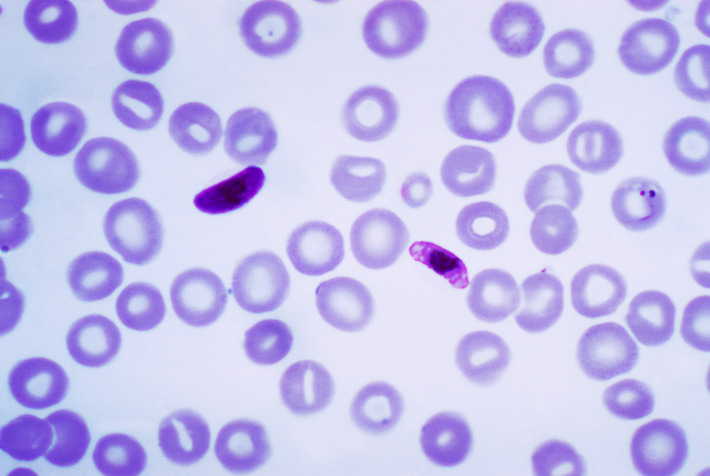
P. falciparum:
A thin film, Giemsa stained micrograph shows a macrogametocyte and a microgametocyte of the parasite.
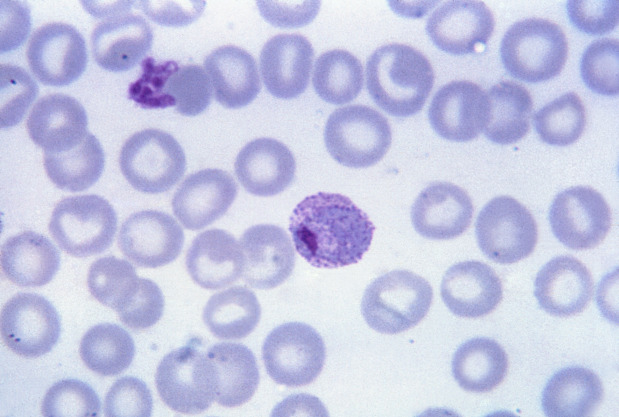
P. vivax:
A thin film, Giemsa stained micrograph shows a mature trophozoite with amoeboid cytoplasm, large chromatin dots (Schüffner’s granules), and fine, yellowish-brown pigment.
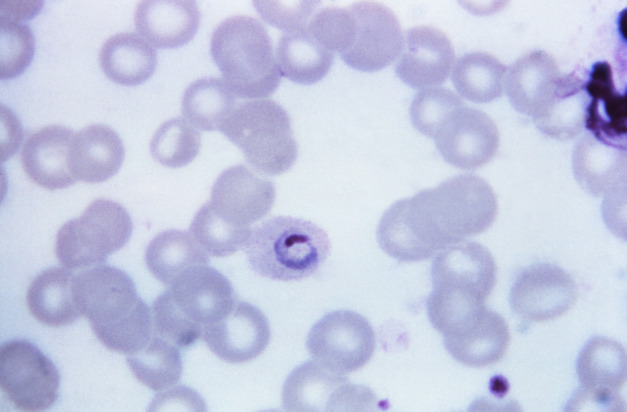
P. ovale:
A thin film, Giemsa stained micrograph shows ring-shaped trophozoite.
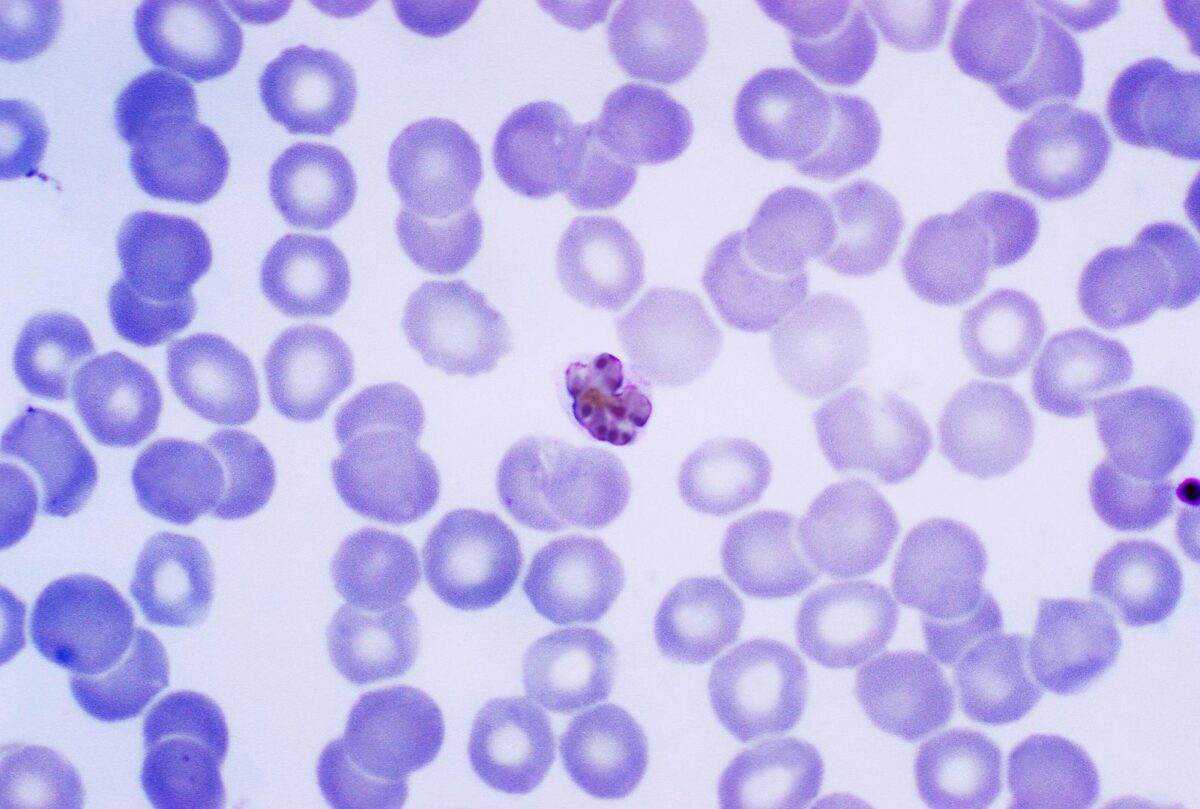
P. malariae:
A thin film, Giemsa stained micrograph shows a mature schizont within an infected RBC. The parasite contains 6–12 merozoites with large nuclei, and has a coarse, dark-brown pigment.