Zika virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology belongs to the genus Flavivirus Flavivirus A genus of flaviviridae containing several subgroups and many species. Most are arboviruses transmitted by mosquitoes or ticks. The type species is yellow fever virus. Tick-borne Encephalitis Virus and is primarily transmitted by Aedes aegypti mosquitoes, but can also be transmitted sexually and transplacentally. Although most infected patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are asymptomatic, some may present with low-grade fever Low-Grade Fever Erythema Infectiosum, pruritic rash Rash Rocky Mountain Spotted Fever, and conjunctivitis Conjunctivitis Conjunctivitis is a common inflammation of the bulbar and/or palpebral conjunctiva. It can be classified into infectious (mostly viral) and noninfectious conjunctivitis, which includes allergic causes. Patients commonly present with red eyes, increased tearing, burning, foreign body sensation, and photophobia. Conjunctivitis. Congenital Zika syndrome is the most severe complication of a Zika virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology infection, where transplacental fetal infection manifests with ocular defects, microcephaly Microcephaly A congenital abnormality in which the cerebrum is underdeveloped, the fontanels close prematurely, and, as a result, the head is small. (desk reference for neuroscience, 2nd ed. ). Fetal Alcohol Spectrum Disorder, spasticity Spasticity Spinal Disk Herniation, and seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures. The diagnosis is made either by RT-PCR RT-PCR A variation of the pcr technique in which cDNA is made from RNA via reverse transcription. The resultant cDNA is then amplified using standard pcr protocols. Polymerase Chain Reaction (PCR) or serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus. Since there is no definitive management for a Zika virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology infection, the treatment is mostly supportive. Prevention includes controlling the mosquito population, using insect repellants, and wearing protective clothing.
Last updated: Jan 9, 2025
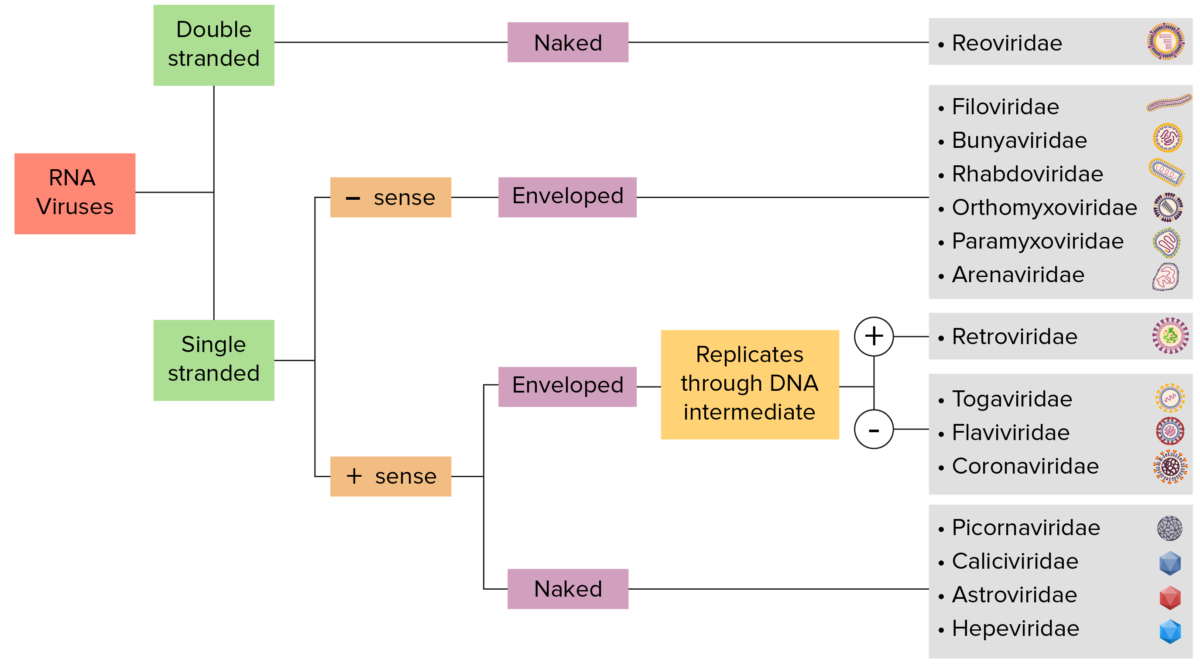
RNA virus identification:
Viruses can be classified in many ways. Most viruses, however, will have a genome formed by either DNA or RNA. RNA genome viruses can be further characterized by either a single- or double-stranded RNA. “Enveloped” viruses are covered by a thin coat of cell membrane (usually taken from the host cell). If the coat is absent, the viruses are called “naked” viruses. Viruses with single-stranded genomes are “positive-sense” viruses if the genome is directly used as messenger RNA (mRNA), which is translated into proteins. “Negative-sense,” single-stranded viruses use RNA-dependent RNA polymerase, a viral enzyme, to transcribe their genome into messenger RNA.
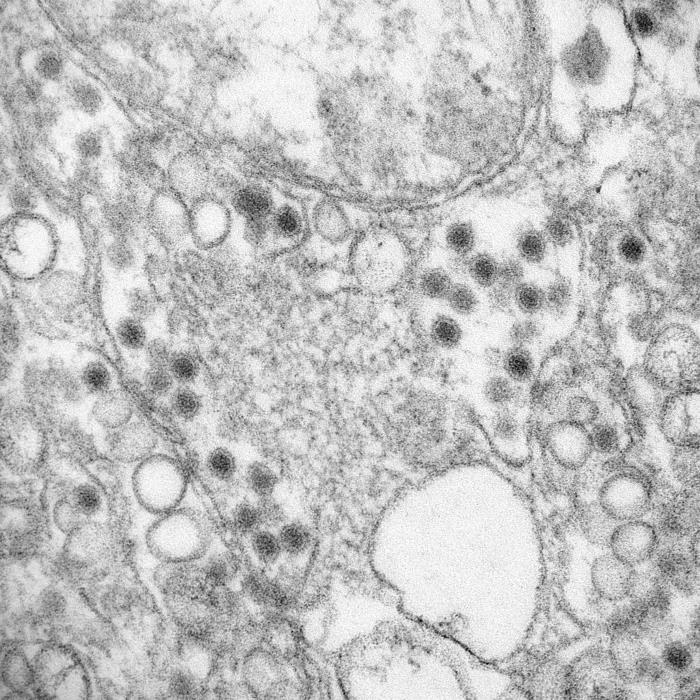
Transmission electron microscopic image of Zika virus:
A member of the family Flaviviridae, grown in LLC-MK2 culture cells. Virus particles are 40 nm in diameter, and have an outer envelope and inner dense core. Also note the smooth membrane vesicles, which are recognized as the replication complex for this virus family.
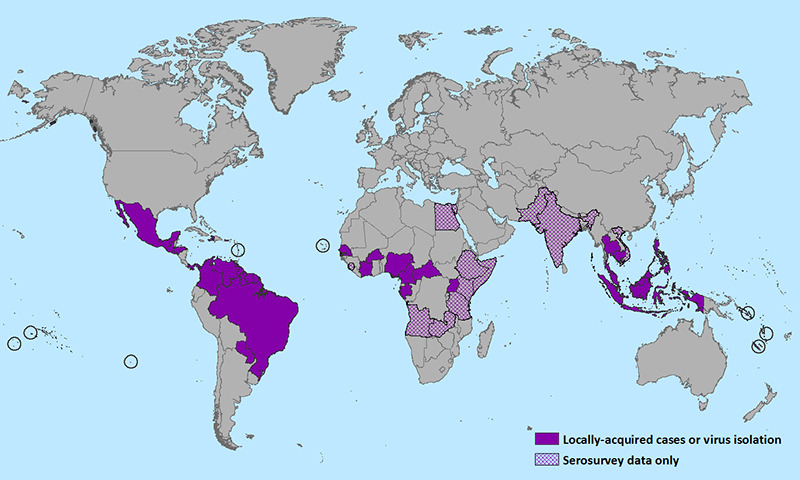
World map showing the distribution of Zika virus (2016)
Image: “CDC map of Zika virus distribution as of 15 January 2016” by CDC. License: Public Domain
Aedes aegypti feeding on human skin
Image: “Aedes aegypti bloodfeeding CDC Gathany” by James Gathany. License: Public Domain
A rash on the back due to zika virus infection.
Image: “Epidemiologic investigation of a family cluster of imported ZIKV cases in Guangdong, China: probable human-to-human transmission” by Yingxian Yin, et al. License: CC BY 4.0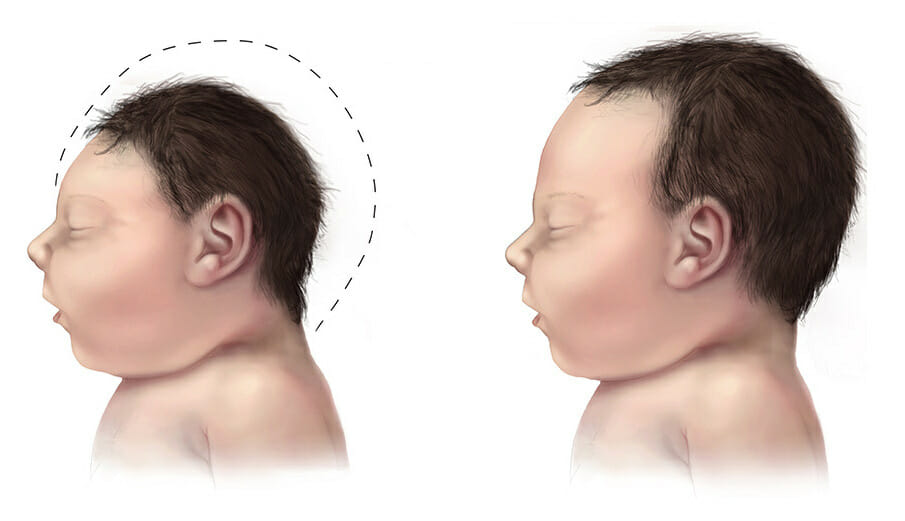
Microcephaly in a baby due to zika virus.
Image: “Microcephaly” by Brar_j- Flickr. License: CC BY 2.0| Zika virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology | West Nile virus West Nile Virus West Nile virus is an enveloped, positive-sense, single-stranded RNA virus of the genus Flavivirus. Birds are the primary hosts and the disease is most often transmitted by Culex mosquitoes. Most people infected with West Nile virus are asymptomatic. Some patients develop West Nile fever (a self-limited, febrile illness) and a very small proportion of patients develop West Nile neuroinvasive disease. West Nile Virus | Dengue Dengue An acute febrile disease transmitted by the bite of aedes mosquitoes infected with dengue virus. It is self-limiting and characterized by fever, myalgia, headache, and rash. Severe dengue is a more virulent form of dengue. Dengue Virus virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology | |
|---|---|---|---|
| Characteristics |
|
|
|
| Transmission |
|
Culex mosquitoes | Aedes mosquitoes |
| Clinical |
|
|
|
| Diagnosis |
|
|
|
| Management | Symptomatic treatment | ||
| Prevention |
|
|
|
The following conditions are differential diagnoses for congenital Zika syndrome: