Hepatitis C is an infection of the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy caused by the hepatitis C virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology (HCV). Hepatitis C virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology is an RNA RNA A polynucleotide consisting essentially of chains with a repeating backbone of phosphate and ribose units to which nitrogenous bases are attached. RNA is unique among biological macromolecules in that it can encode genetic information, serve as an abundant structural component of cells, and also possesses catalytic activity. RNA Types and Structure virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology and a member of the genus Hepacivirus and the family Flaviviridae. The infection can be transmitted through infectious blood or body fluids and may be transmitted during childbirth or through IV drug use or sexual intercourse. Hepatitis C virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology can cause both acute and chronic hepatitis, ranging from a mild to a serious, lifelong illness including liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis and hepatocellular carcinoma Hepatocellular carcinoma Hepatocellular carcinoma (HCC) typically arises in a chronically diseased or cirrhotic liver and is the most common primary liver cancer. Diagnosis may include ultrasound, CT, MRI, biopsy (if inconclusive imaging), and/or biomarkers. Hepatocellular Carcinoma (HCC) and Liver Metastases ( HCC HCC Hepatocellular carcinoma (HCC) typically arises in a chronically diseased or cirrhotic liver and is the most common primary liver cancer. Diagnosis may include ultrasound, CT, MRI, biopsy (if inconclusive imaging), and/or biomarkers. Hepatocellular Carcinoma (HCC) and Liver Metastases). Hepatitis C infection is diagnosed by testing for the presence of HCV antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions and HCV RNA RNA A polynucleotide consisting essentially of chains with a repeating backbone of phosphate and ribose units to which nitrogenous bases are attached. RNA is unique among biological macromolecules in that it can encode genetic information, serve as an abundant structural component of cells, and also possesses catalytic activity. RNA Types and Structure. Management is supportive but includes direct antiviral Antiviral Antivirals for Hepatitis B agents (DAAs) if infection does not resolve spontaneously.
Last updated: May 16, 2024
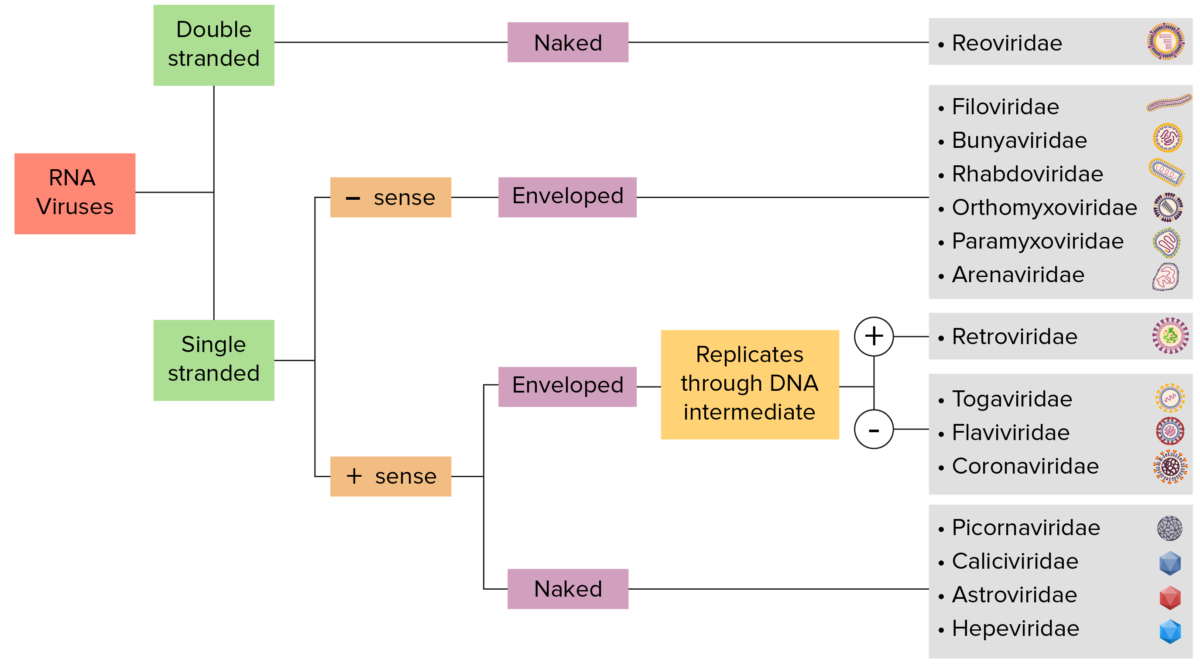
Flowchart RNA viruses
Image by Lecturio. License: CC BY-NC-SA 4.0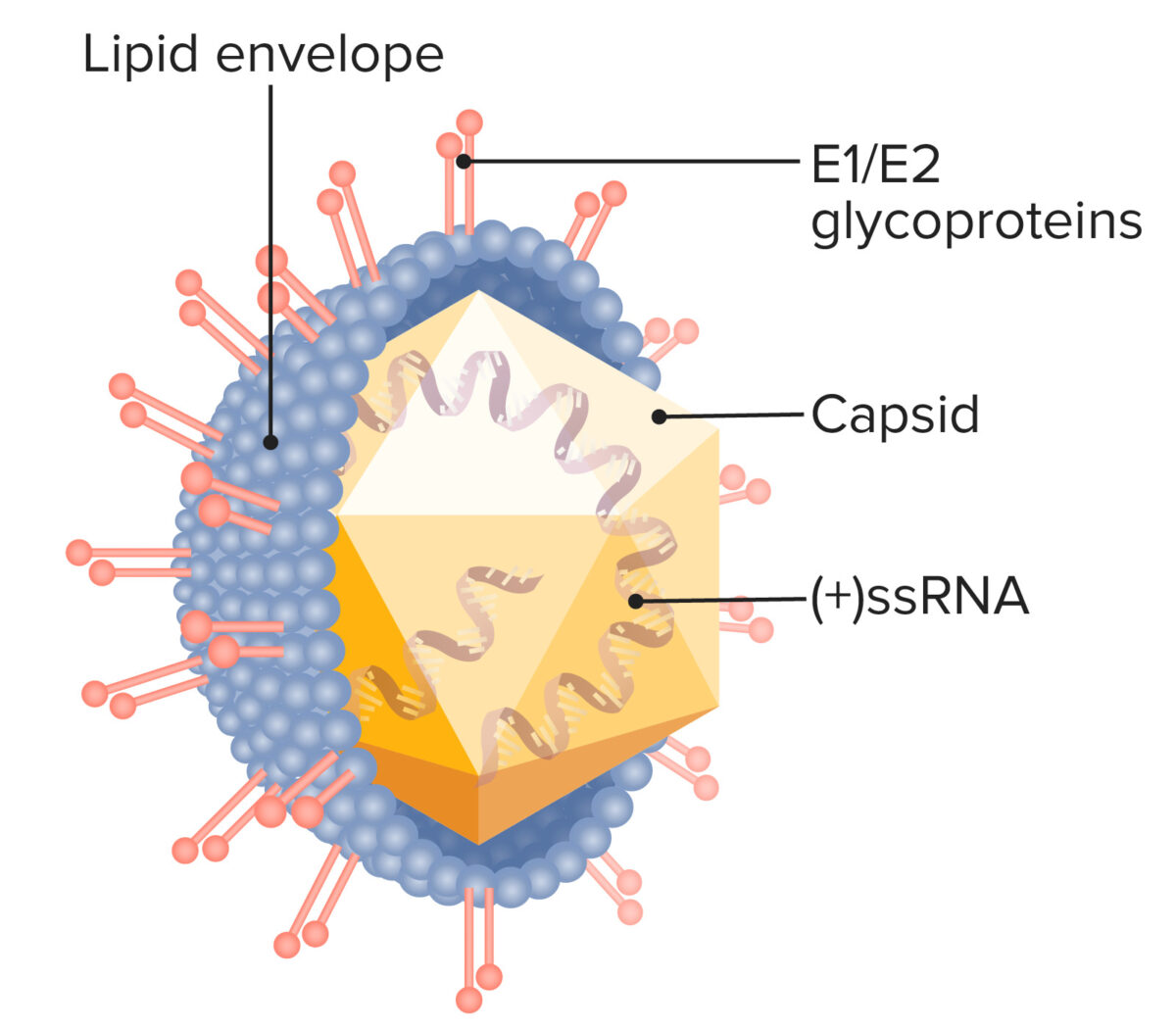
Structure of hepatitis C virus:
Note the positive-sense ssRNA and the glycoproteins embedded in the virus’s lipid envelope, which mediate cell entry.
Humans are the only reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli for the virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology. Modes of transmission include:
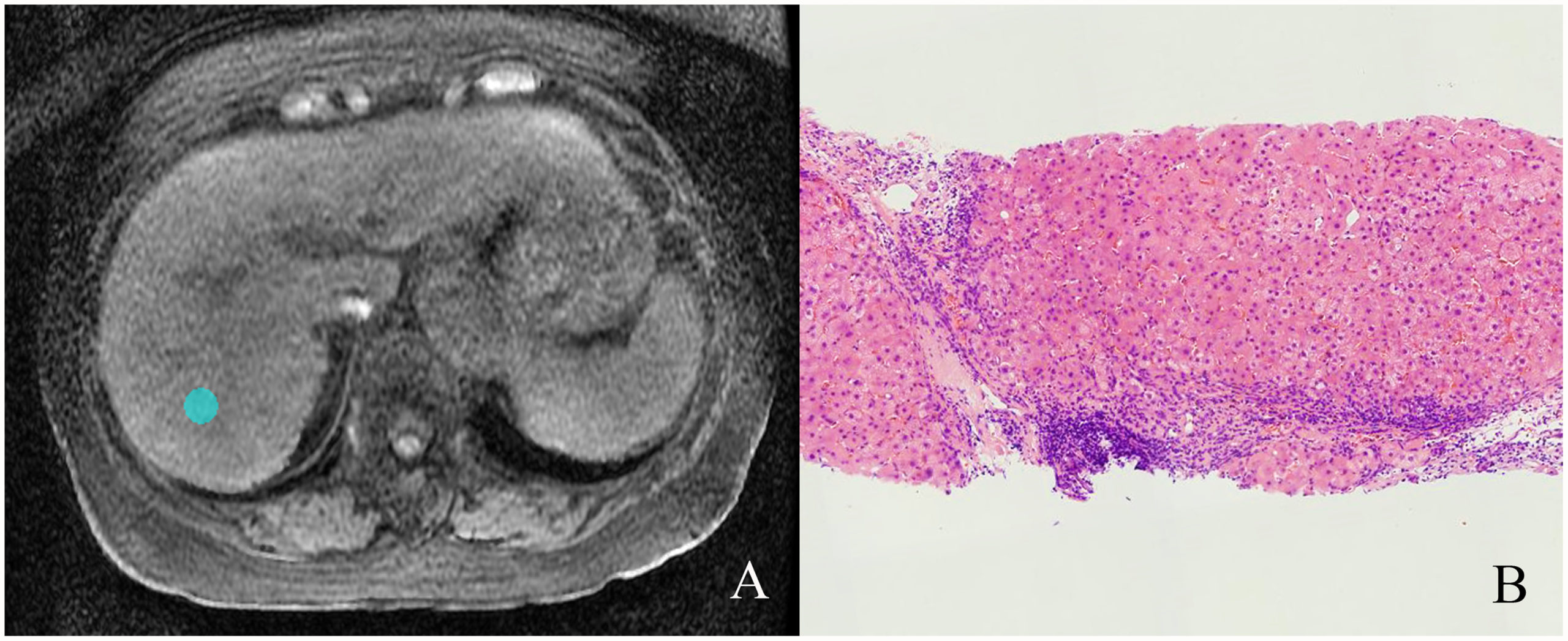
An individual with a chronic hepatitis C infection:
A) MRI showing liver fibrosis
B) Liver biopsy showing stage 4 liver fibrosis and grade 2 necroinflammatory activity

An individual with erythema nodosum due to chronic hepatitis C infection
Image: “Erythema nodosum – Kolkata 2012-01-03 7753” by Biswarup Ganguly. License: CC BY 3.0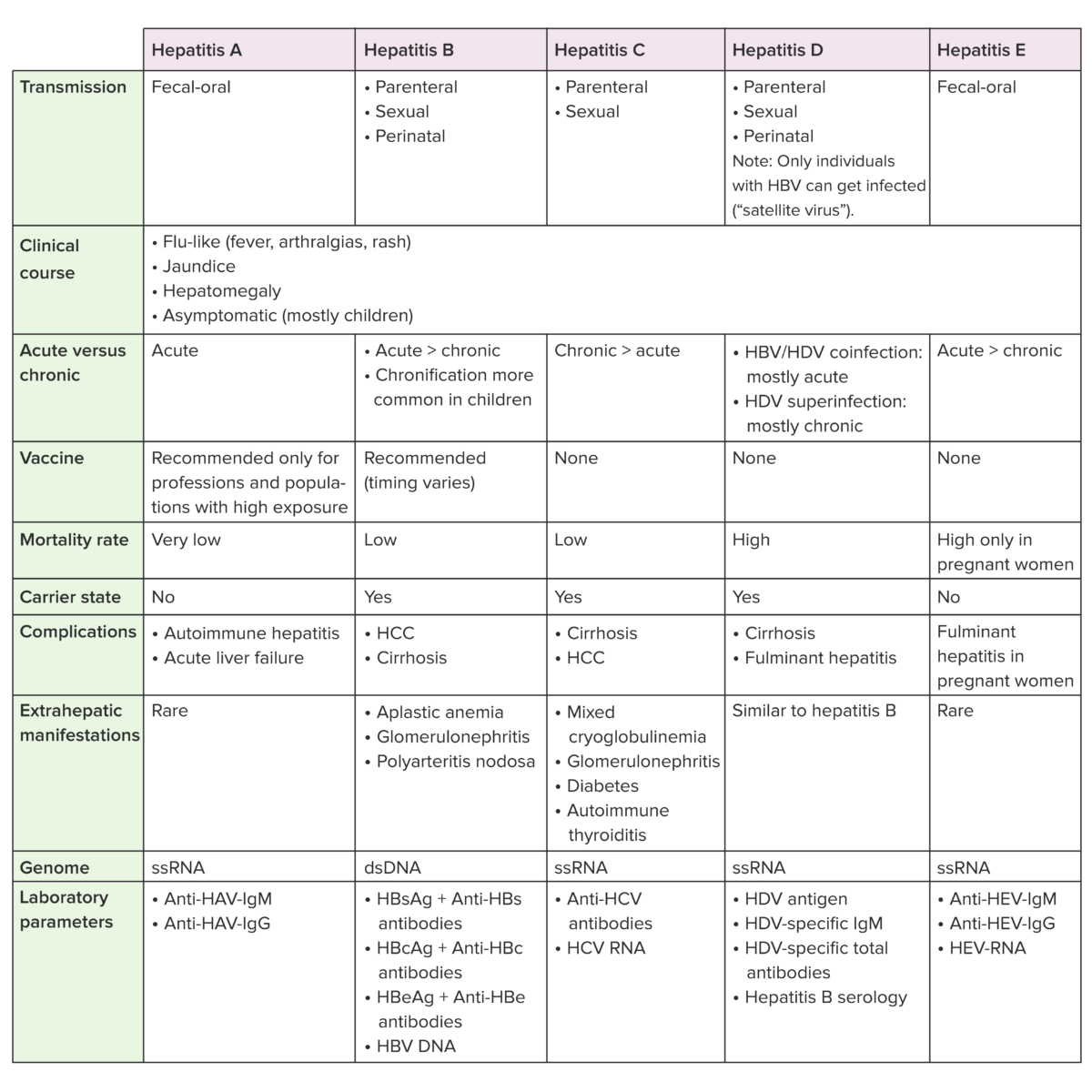
Anti-HBc: hepatitis B core antibody
Anti-HBs: hepatitis B surface antibody
HBcAg: hepatitis B core antigen
HBsAg: hepatitis B surface antigen
HBV: hepatitis B virus
HCC: hepatocellular carcinoma
HAV: hepatitis A virus
HCV: hepatitis C virus
HDV: hepatitis D virus