Lichen planus (LP) is an idiopathic Idiopathic Dermatomyositis, cell-mediated inflammatory skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions disease. It is characterized by pruritic, flat-topped, papular, purple skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions commonly found on the flexural surfaces of the extremities. Other areas affected include genitalia, nails, scalp, and mucous membranes. Exact etiology is unknown but has been found to be associated with hepatitis C Hepatitis C Hepatitis C is an infection of the liver caused by the hepatitis C virus (HCV). The infection can be transmitted through infectious blood or body fluids and may be transmitted during childbirth or through IV drug use or sexual intercourse. Hepatitis C virus can cause both acute and chronic hepatitis, ranging from a mild to a serious, lifelong illness including liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis C Virus infection, other diseases, and multiple drugs. Skin biopsy Skin Biopsy Secondary Skin Lesions of the most prominent lesion is used for confirmation of the diagnosis. Cutaneous LP usually resolves in 1–2 years. Other forms, however, are chronic and persistent. Topical corticosteroids Corticosteroids Chorioretinitis are the preferred treatment.
Last updated: Apr 14, 2023


Lichen planus of the back of an 11-year-old African American boy with a 6-year history of generalized LP. Note the presence of the Koebner phenomenon: the spread of LP lesions along areas of trauma, including scratches on the skin.
Image: “12186” by CDC. License: Public Domain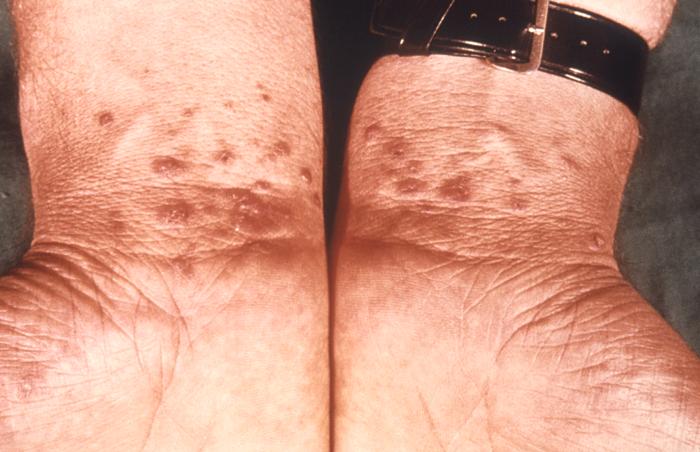
Lichen planus on bilateral wrists
Image: “6545” by CDC/ Susan Lindsley. License: Public Domain
Lichen planus presenting as Wickham’s striae on the oral mucosa
Image: “12632” by CDC/ Robert E. Sumpter. License: Public Domain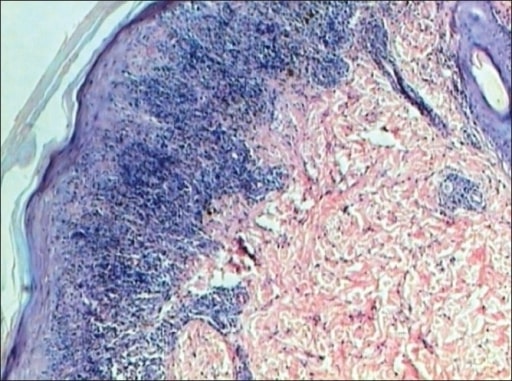
Lichen planus: epidermis shows hyperkeratosis, hypergranulosis, acanthosis, and saw-tooth rete ridges. Dermis shows a band-like lymphocytic infiltrate touching the epidermis (H&E stain, ×40).
Image: “Lichen planus” by Department of Pathology, JJ Hospital, Mumbai, India. License: CC BY 2.0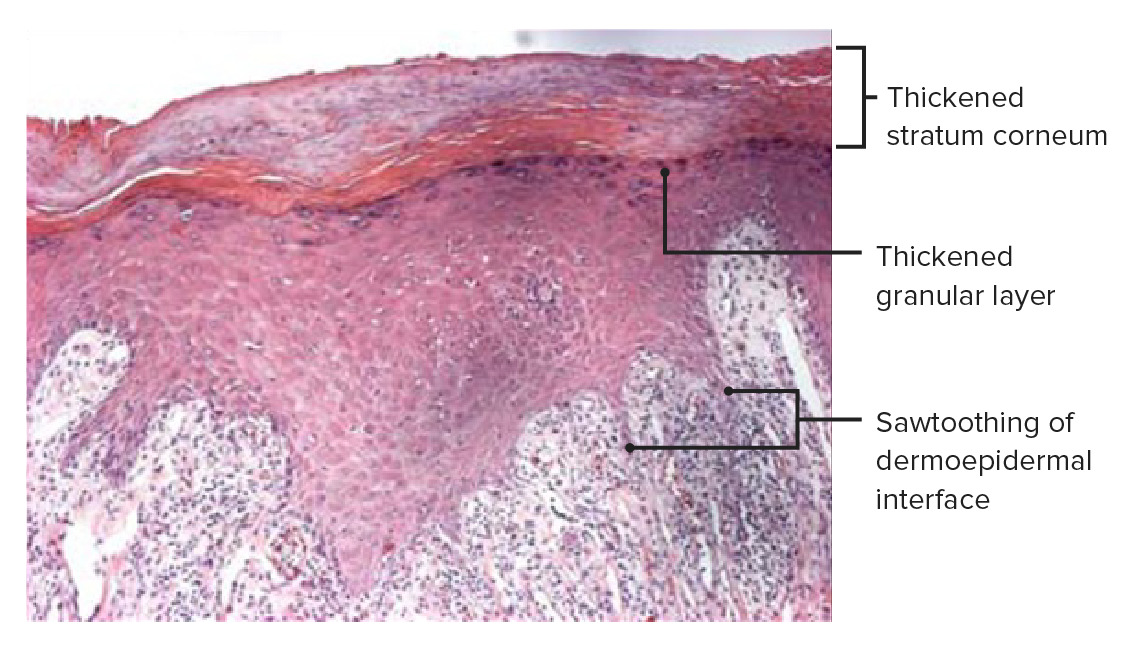
Histopathology of a skin biopsy of an LP plaque showing dense lichenoid inflammatory infiltrates underneath the lamina propria. Note the inflammation at the dermal–epidermal junction and an angulated zigzag lower contour, which gives it the saw-tooth appearance characteristic of LP. Note also the thickening of the granular cell layer (hypergranulosis) and the stratum corneum (hyperkeratosis), which are more pronounced in the white lines of Wickham’s striae.
Image: “Histopathology of lichen planus” by Shi G, Sohn KC et al. License: CC BY 4.0, edited by Lecturio.