The identification Identification Defense Mechanisms and classification of skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions in a patient are important steps in the diagnosis of any skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions disorder. Primary lesions represent the initial presentation of the disease process. Secondary lesions develop from irritated or manipulated primary lesions, and/or disease progression. Along with history, a comprehensive examination of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, appendages, and mucous membranes is required to differentiate between conditions. The key features noted during examination include the type, morphology, size, color, shape, arrangement, and distribution of the presenting lesions. At times, diagnostic procedures may be necessary.
Last updated: Dec 29, 2023

Hyperpigmented café-au-lait macules in a patient with neurofibromatosis type 1
Image: “Breast cancer associated with neurofibromatosis type 1: A case series and review of the literature” by Khalil J, Afif M, Elkacemi H, Benoulaid M, Kebdani T, Benjaafar N. License: CC BY 4.0
A patch of vitiligo in a person with dark skin
Image: “Vitiligo and the melanocyte reservoir” by Falabella, R. License: CC BY 2.0
Hyperpigmentation on the cheek of a patient with melasma
Image: “A study comparing chemical peeling using modified Jessner’s solution and 15% trichloroacetic acid versus 15% trichloroacetic acid in the treatment of melasma” by Safoury OS, Zaki NM, El Nabarawy EA, Farag EA. License: CC BY 2.0
Seborrheic keratosis
Image by Jeremy Greer, MD (Lecturio).
Two papules representing a basal cell carcinoma
Image: “Photodynamic Therapy and Non-melanoma Skin Cancer” by Cancers. License: CC BY 4.0, cropped by Lecturio.
A psoriatic lesion on the knee
Image: “Psoriatic lesion on the knee” by Department of Neurology, Wakayama Medical University, Japan. License: CC BY 2.0
Neurofibromas
Image: “Breast cancer associated with neurofibromatosis type 1: A case series and review of the literature” by Khalil J, Afif M, Elkacemi H, Benoulaid M, Kebdani T, Benjaafar N. License: CC BY 4.0, cropped by Lecturio.
Vesicles caused by herpes simplex virus
Image: “Transplant biology at a crossroads” by Sedwick C. License: CC BY 4.0, cropped by Lecturio.
Cutaneous findings in bullous pemphigoid:
Multiple large, tense vesicles and bullae in the groin on normal to mildly erythematous skin

Urticaria
Image: “Urticarial Vasculitis in a Teenage Girl” by McGuffin A, Vaughan A, Wolford J. License: CC BY 3.0
Bacterial folliculitis on the lower leg presenting as follicular pustules
Image: “Folliculitis on lower leg” by Da pacem Domine. License: Public Domain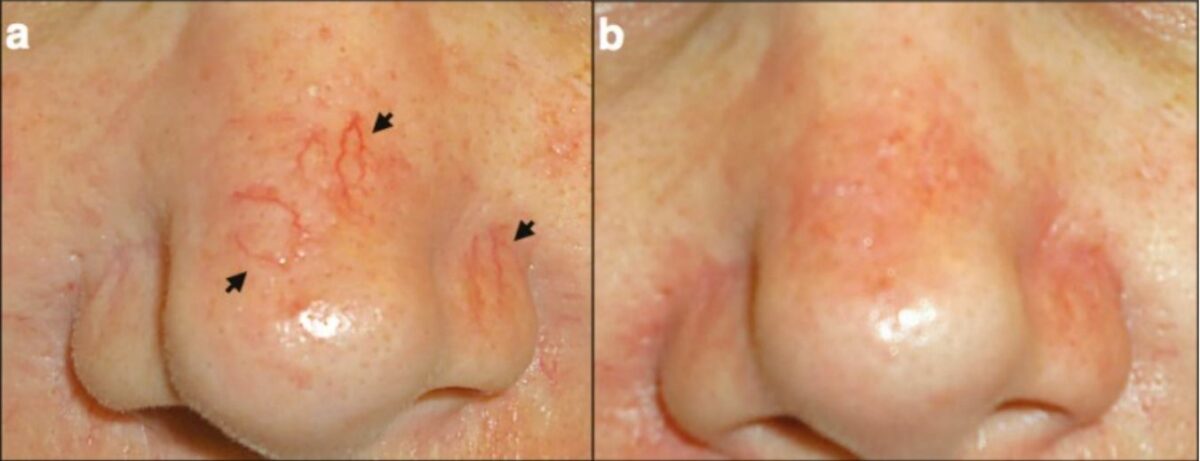
Nose telangiectasias:
a: Telangiectasias (arrows)
b: After treatment with cautery

Petechiae around intravenous site
Image by Jeremy Greer, MD (Lecturio).
Petechiae/purpura on the lower limb seen in Henoch-Schöenlein purpura
Image: “Henoch-Schönlein purpura in an older man presenting as rectal bleeding and IgA mesangioproliferative glomerulonephritis: A case report” by Cheungpasitporn W, Jirajariyavej T, Howarth CB, Rosen RM. License: CC BY 2.0A general physical examination as well as a focused dermatological examination should be performed:
Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions features and commonly associated skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions conditions and/or lesions to consider:
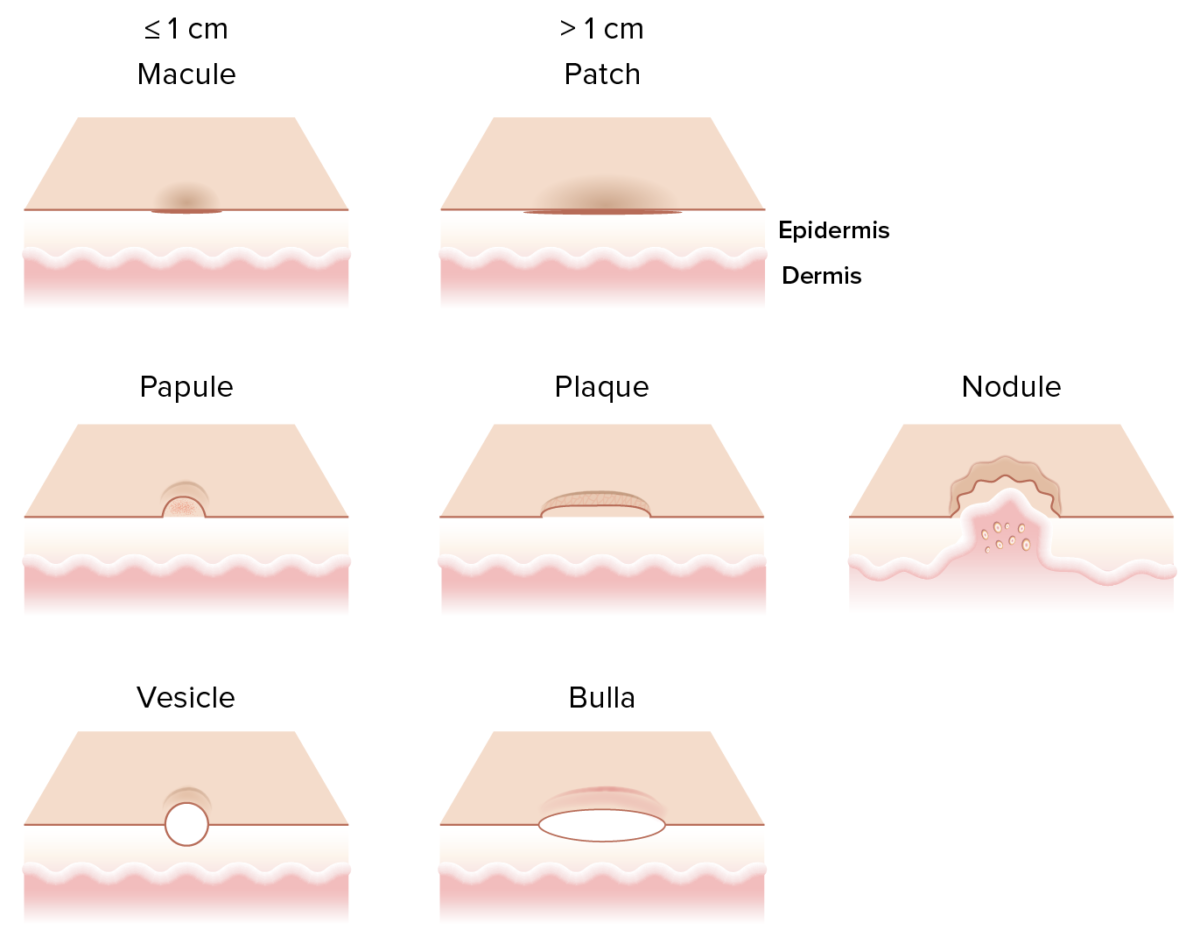
Different primary skin lesions:
A macule is a flat ≤ 1 cm non-palpable skin lesion.
A papule is a raised ≤ 1 cm palpable skin lesion.
A nodule is a large 1–5 cm firm raised lesion, usually extending into the dermis and subcutaneous tissue.
A plaque is a raised > 1 cm skin lesion with palpable surface change as it arises from the epidermis.
A vesicle is a small ≤ 1 cm fluid-containing blister while a bulla is a large > 1 cm clear fluid-containing blister.