Nevi (singular nevus), also known as “ moles Moles Primary Skin Lesions,” are benign Benign Fibroadenoma neoplasms Neoplasms New abnormal growth of tissue. Malignant neoplasms show a greater degree of anaplasia and have the properties of invasion and metastasis, compared to benign neoplasms. Benign Bone Tumors of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions. Nevus is a non-specific medical term because it encompasses both congenital and acquired lesions, hyper- and hypopigmented lesions, and raised or flat lesions. Additionally, nevi can be found within different depths of the layers of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and originate from various types of cells (e.g., melanocytic, connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology, vascular). Nevi also have a wide variety of characteristic forms, which must be well understood in order to differentiate nevi from malignant melanoma Melanoma Melanoma is a malignant tumor arising from melanocytes, the melanin-producing cells of the epidermis. These tumors are most common in fair-skinned individuals with a history of excessive sun exposure and sunburns. Melanoma. In this concept page, we will cover the basic classifications and most common types of nevi as well as the clinical criteria used to assess them.
Last updated: Jan 2, 2025
A nevus (plural nevi) is a benign Benign Fibroadenoma neoplasm of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions:
Nevi can be classified in various ways, according to several factors that are not mutually exclusive:
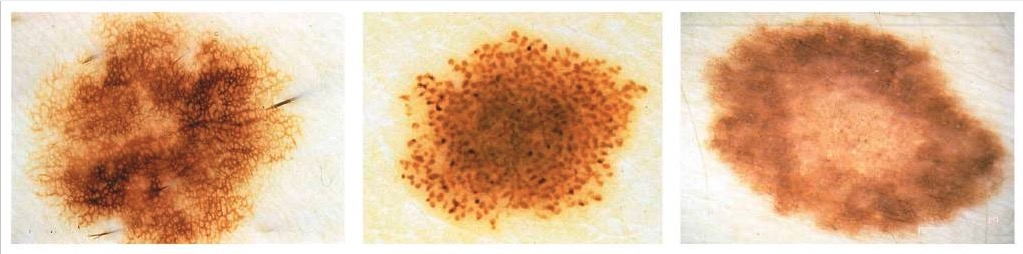
From left to right: reticular, starburst, and globular types of nevi
Image: “Clark nevus” by the Department of Automatics and Biomedical Engineering, AGH University of Science and Technology, Aleja Mickiewicza 30, 30-059 Krakow, Poland. License: CC BY 4.0.
Congenital melanocytic nevus: a brown well-circumscribed papule on the nose that developed shortly after birth
Image: “Congenital melanocytic nevus” by M. Sand et al. License: CC BY 2.0.
Mongolian spot or congenital dermal melanocytosis over the lumbar and gluteal regions
Image: “Enorme tache mongoloïde” by Service de Pédiatrie, Hôpital Militaire d’Instruction Mohamed V, Université Med V, Souissi, Maroc. License: CC BY 2.0.
Congenital nevus of Ito: blue-gray macule, representing a benign dermal melanocytosis that preferentially affects areas innervated by the posterior supraclavicular nerves
Image: “Nevus of Ito” by the U.S. National Library of Medicine. License: CC BY 4.0.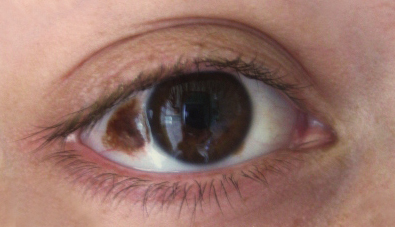
Congenital nevus of Ota: benign dermal melanocytosis that preferentially affects areas innervated by the 1st and 2nd division of the trigeminal nerve. A congenital nevus of Ota often affects the sclerae.
Image: “Nevus” by Luninsky. License: CC BY 3.0.| Type | Description | Presentation |
|---|---|---|
| Junctional nevi |
|
|
| Compound nevi | Nevus cells found at the dermo-epidermal junction and intradermally, smaller cells that produce less melanin Melanin Insoluble polymers of tyrosine derivatives found in and causing darkness in skin (skin pigmentation), hair, and feathers providing protection against sunburn induced by sunlight. Carotenes contribute yellow and red coloration. Seborrheic Keratosis |
|
| Intradermal nevi | Nevus cells found intradermally, small cells that produce little to no melanin Melanin Insoluble polymers of tyrosine derivatives found in and causing darkness in skin (skin pigmentation), hair, and feathers providing protection against sunburn induced by sunlight. Carotenes contribute yellow and red coloration. Seborrheic Keratosis |
|
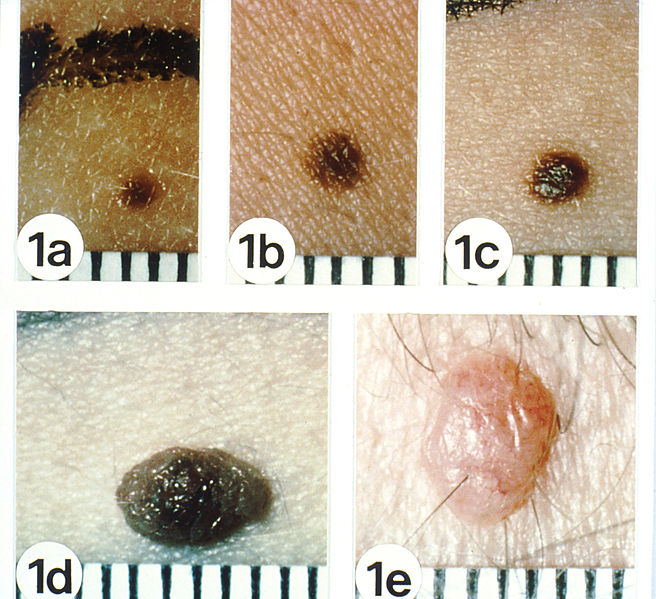
Natural history of acquired melanocytic nevi
Common nevi (“moles”) begin as uniformly tan or brown macules, 1 to 2 mm in diameter (a), expand to a larger macule (b), progress to a pigmented papule that may be minimally (c) or obviously (d) elevated above the surface of the skin, and terminate as a pink or flesh-colored papule (e).
Acquired melanocytic nevi are junctional (a, b), compound (c, d), and dermal (e) nevi, respectively. Note their smooth borders, uniform coloring, and clear demarcation from the surrounding skin with smooth borders.
Acquired melanocytic nevi are usually < 5 mm in diameter.
Based on clinical appearance, a typical benign Benign Fibroadenoma nevus should have the following characteristics:
A dysplastic or atypical nevus is a benign melanocytic nevus with an appearance that differs from common nevi or “ moles Moles Primary Skin Lesions” based on the ABCDE criteria ( asymmetry Asymmetry Examination of the Upper Limbs, border irregularity, color variation, diameter ≥ 6 mm, and evolution):
| Common ( benign Benign Fibroadenoma) nevi | Atypical nevi | Melanoma Melanoma Melanoma is a malignant tumor arising from melanocytes, the melanin-producing cells of the epidermis. These tumors are most common in fair-skinned individuals with a history of excessive sun exposure and sunburns. Melanoma (m.) | |
|---|---|---|---|
| Asymmetry Asymmetry Examination of the Upper Limbs (A) | Symmetric (a straight line drawn through the center of the lesion gives 2 mirror images) |
|
|
| Border (B) | Smooth, well-defined border | Irregular margin with ill-defined border | Irregular margin with ill-defined border |
| Color (C) | Uniform color or regular Regular Insulin color pattern (e.g., speckled or starburst) | Variegated color or varying shades of color | Variegated color or varying shades of color |
| Diameter (D) | < 5 mm | Often ≥ 5 mm | > 6 mm |
| Evolution (E) | Stable or slow growth |
|
|
| Location (not part of criteria, but an important factor) | Concentrated on sun-exposed sites |
|
Depends on type:
|

A dysplastic nevus presenting as a maculopapular lesion. The central portion is the papular area, barely perceptible in this photograph. Note the irregular and indistinct border and the variegated color pattern of brown and pink.
Image: “Dysplastic nevi” by the National Cancer Institute. License: Public domain.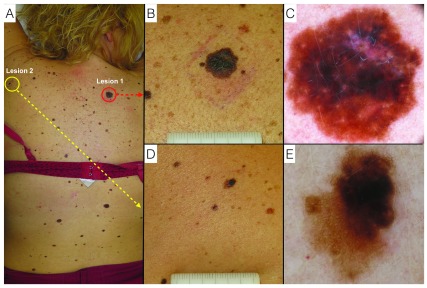
Melanoma and dysplastic nevus.
A: clinical overview of the patient;
B: lesion 1: melanoma, naked-eye clinical close-up;
C: lesion 1: melanoma, digital dermoscopy view;
D: lesion 2: dysplastic nevus, naked-eye clinical close-up;
E: lesion 2: dysplastic nevus, digital dermoscopy view.