Barrett esophagus is a consequence of chronic gastroesophageal reflux disease (GERD) that leads to metaplastic replacement of stratified squamous epithelium with gastric columnar epithelium in the esophagus. The condition is associated with an increased risk of esophageal adenocarcinoma. Workup includes an esophagogastroduodenoscopy (EGD) showing proximal displacement of the squamocolumnar junction (Z-line) from the gastroesophageal junction (GEJ). Diagnosis is made by biopsy revealing columnar epithelium and goblet cells in the distal esophagus. Treatment is primarily with proton pump inhibitors (PPIs) and lifestyle modification. Surveillance with repeat EGD and biopsy is necessary to monitor for early signs of dysplasia.
Last updated: Jun 3, 2025
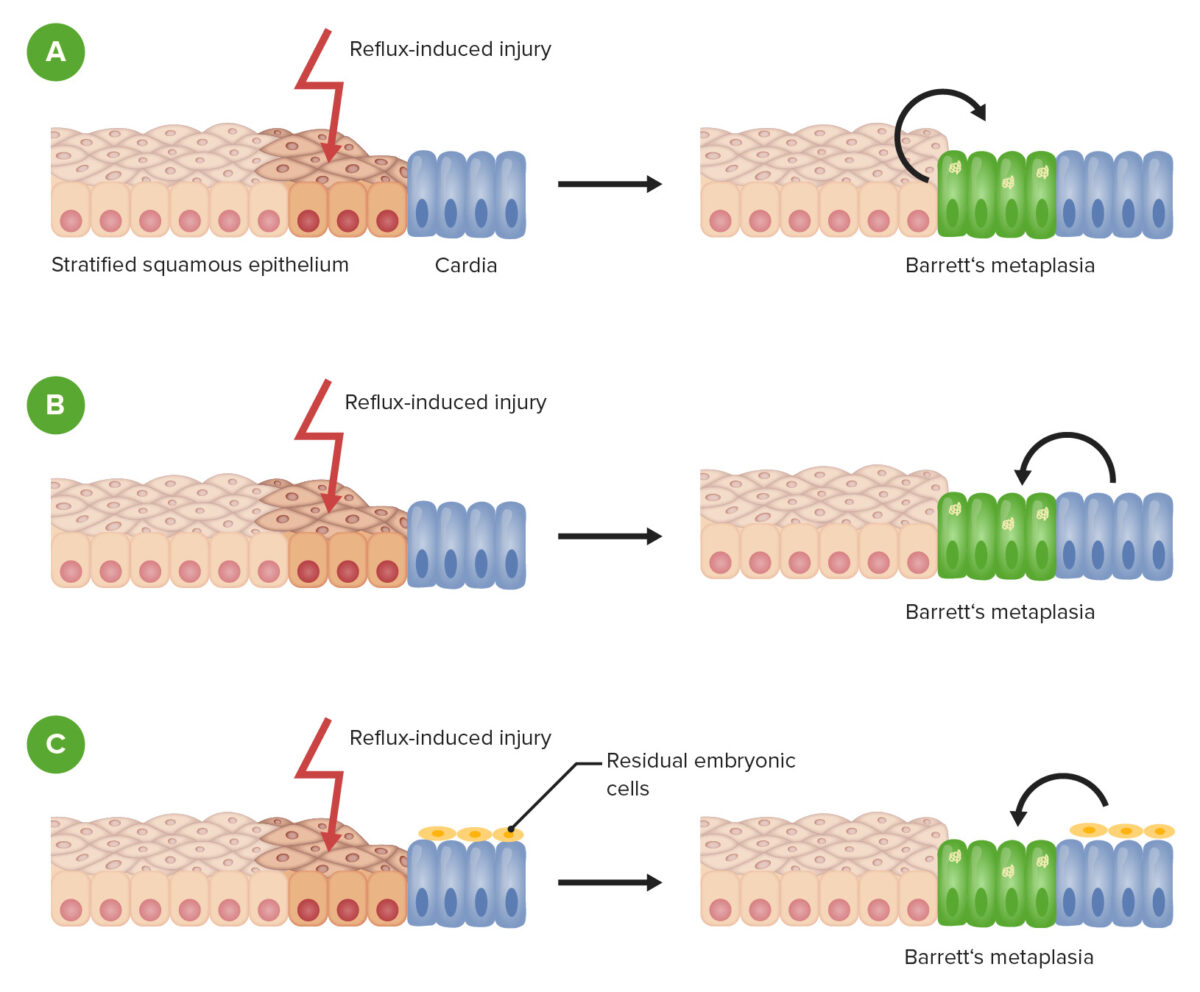
Barrett esophagus metaplasia.
Schematic demonstrating the development of metaplasia after injury to the esophageal epithelium in Barrett esophagus. There are several proposed mechanisms.
A: Repair of reflux-induced injury leads to transdifferentiation of esophageal epithelial cells.
B: Repair of damaged tissue results from progenitor cells of the gastric cardia.
C: Repair of damaged tissue results from residual embryonic cell migration from the gastroesophageal junction or gastric cardia.
Screening Screening Preoperative Care:
Esophagogastroduodenoscopy (EGD):
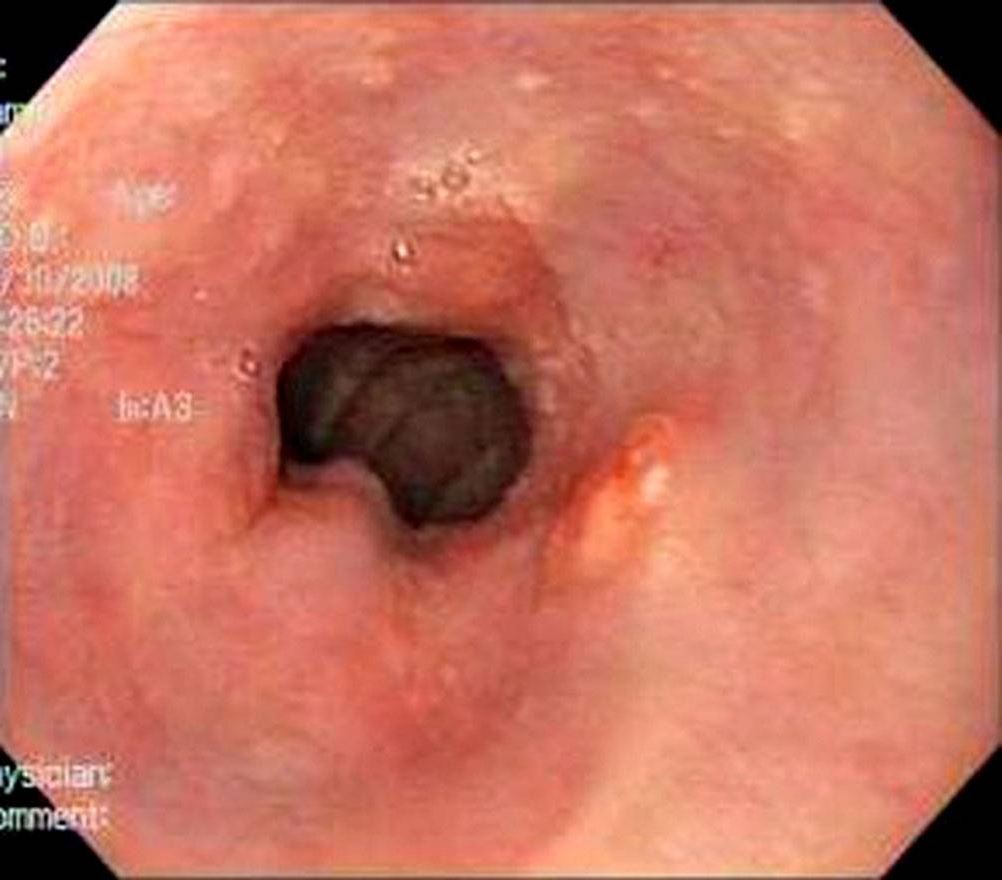
Esophagogastroduodenoscopy revealing erythematous epithelium in the distal esophagus, consistent with Barrett esophagus. Notice the difference between the erythema of the columnar epithelium and the pale, glossy squamous epithelium. This junction is known as the Z-line.
Image: “Esophageal granular cell tumor colliding with intramucosal adenocarcinoma” by Alkhoury F, Martin JT, Fiedler P, Jaffe PE. License: CC BY 3.0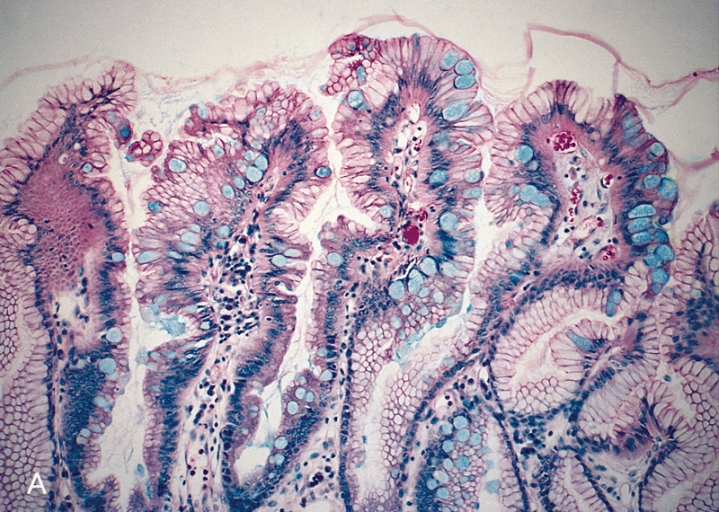
Esophageal mucosal biopsy showing columnar epithelium and numerous goblet cells (light-blue cells), consistent with Barrett esophagus.
Image: “Barrett’s mucosa” by The Armed Forces Institute of Pathology (AFIP). License: Public DomainThe goal is to treat underlying acid reflux to decrease the risk of cancer development.
| Endoscopy Endoscopy Procedures of applying endoscopes for disease diagnosis and treatment. Endoscopy involves passing an optical instrument through a small incision in the skin i.e., percutaneous; or through a natural orifice and along natural body pathways such as the digestive tract; and/or through an incision in the wall of a tubular structure or organ, i.e. Transluminal, to examine or perform surgery on the interior parts of the body. Gastroesophageal Reflux Disease (GERD) biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma findings | Management |
|---|---|
| Barrett esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy ( metaplasia Metaplasia A condition in which there is a change of one adult cell type to another similar adult cell type. Cellular Adaptation only) | PPIs and EGD every 2–3 years |
| Low-grade dysplasia | PPIs and EGD every 6–12 months |
| High-grade dysplasia | Endoscopic ablation or resection (endoscopic or surgical) |
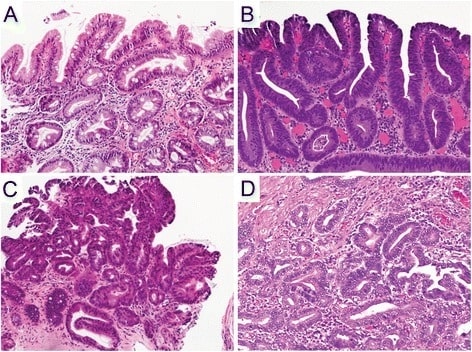
Hematoxylin and eosin staining of esophageal mucosal biopsies.
A: non-dysplastic Barrett mucosa characterized by uniform, bland nuclei arranged in a surface monolayer
B: low-grade dysplasia exhibiting nuclear hyperchromasia, elongation, and stratification extending up to the surface epithelium
C: high-grade dysplasia depicting increased architectural and cytologic complexity, including loss of nuclear polarity
D: intramucosal adenocarcinoma characterized by severe architectural distortion, including angulated glands. (a–d, 100×)
Esophageal adenocarcinoma Esophageal Adenocarcinoma Esophageal Cancer is the most significant morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status.