The salivary glands are exocrine glands Exocrine glands Glands of external secretion that release its secretions to the body's cavities, organs, or surface, through a duct. Glandular Epithelium: Histology positioned in and around the oral cavity. These glands are responsible for secreting saliva into the mouth, which aids in digestion Digestion Digestion refers to the process of the mechanical and chemical breakdown of food into smaller particles, which can then be absorbed and utilized by the body. Digestion and Absorption. Saliva helps keep the oral mucosa Oral mucosa Lining of the oral cavity, including mucosa on the gums; the palate; the lip; the cheek; floor of the mouth; and other structures. The mucosa is generally a nonkeratinized stratified squamous epithelium covering muscle, bone, or glands but can show varying degree of keratinization at specific locations. Stomatitis lubricated, and it provides antimicrobial protection. There are 3 major paired salivary glands: the sublingual, submandibular, and parotid glands Parotid glands The largest of the three pairs of salivary glands. They lie on the sides of the face immediately below and in front of the ear. Gastrointestinal Secretions. There are also hundreds of minor salivary glands found in patches Patches Vitiligo around the oral cavity.
Last updated: Nov 18, 2024
The 3 pairs of major salivary glands are the parotid, submandibular, and sublingual glands Sublingual glands A salivary gland on each side of the mouth below the tongue. Gastrointestinal Secretions.
Production of saliva, which is important in:
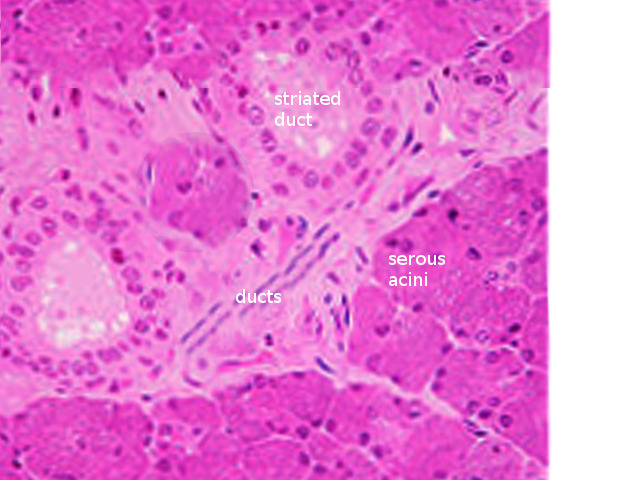
Salivary gland histology
Image: “Salivary gland histology” by S. Bhimji MD. License: CC BY 4.0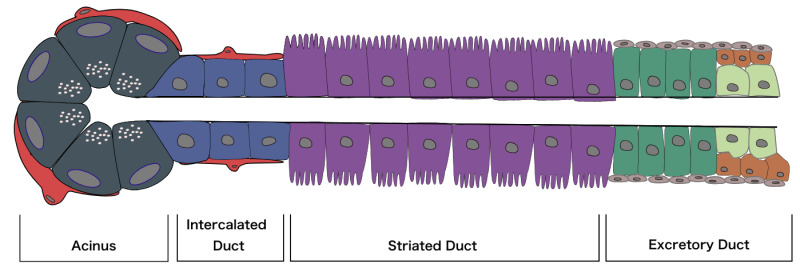
Diagram of an acinus, as well as the 3 main types of ducts through which the salivary fluid is secreted
Image: “Diagram of an acinus, as well as the three main types of duct through which the salivary fluid is secreted” by Mousa Ghannam. License: CC BY 4.0| Parotid | Submandibular | Sublingual | |
|---|---|---|---|
| Location | Anterior to the ear | Inferior and posterior to the mandible Mandible The largest and strongest bone of the face constituting the lower jaw. It supports the lower teeth. Jaw and Temporomandibular Joint: Anatomy | Inferior to the tongue Tongue The tongue, on the other hand, is a complex muscular structure that permits tasting and facilitates the process of mastication and communication. The blood supply of the tongue originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy |
| Development | Ectodermal | Endodermal | Endodermal |
| Size | Largest (15–30 g) | Smaller (10–20 g) | Smallest (3–4 g) |
| Shape | Pyramidal | J-shaped | Almond-shaped |
| Duct and opening site | Stensen duct: opens opposite 2nd maxillary molar |
Wharton duct: opens at the sublingual papilla (lateral to each side of the frenulum linguae) |
Series of ducts: floor of the oral cavity on sublingual fold |
| Nerve supply | Lesser petrosal nerve | Chorda tympani Chorda tympani A branch of the facial (7th cranial) nerve which passes through the middle ear and continues through the petrotympanic fissure. The chorda tympani nerve carries taste sensation from the anterior two-thirds of the tongue and conveys parasympathetic efferents to the salivary glands. Lips and Tongue: Anatomy | Chorda tympani Chorda tympani A branch of the facial (7th cranial) nerve which passes through the middle ear and continues through the petrotympanic fissure. The chorda tympani nerve carries taste sensation from the anterior two-thirds of the tongue and conveys parasympathetic efferents to the salivary glands. Lips and Tongue: Anatomy |
| Type of secretion Secretion Coagulation Studies | Serous | Serous and mucus | Mucus (mainly) and serous |
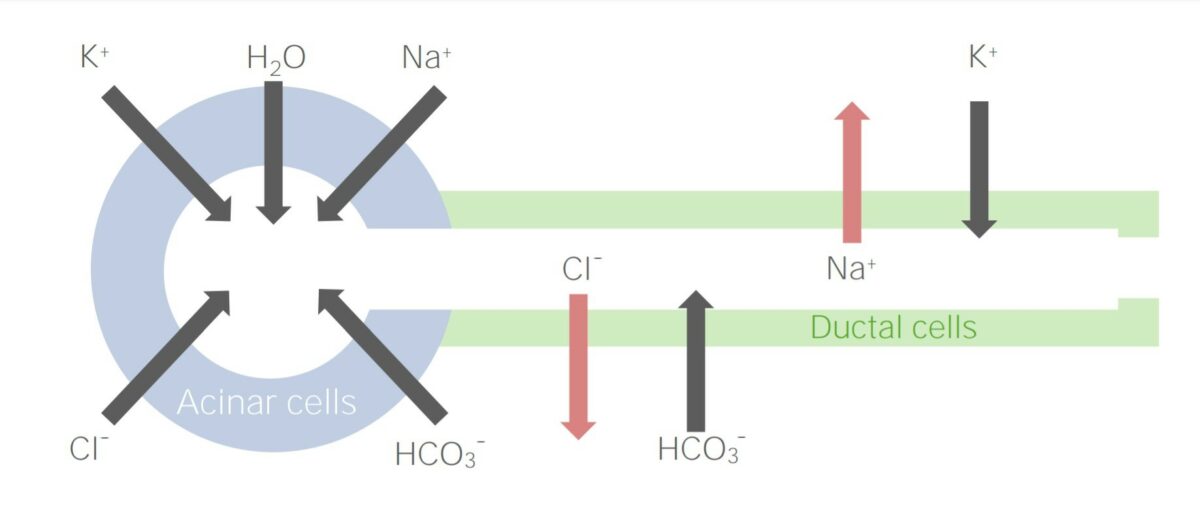
Ion movement during production of saliva and its transports through the salivary duct
Image by Lecturio.Located in the retromandibular fossa, the parotid gland:
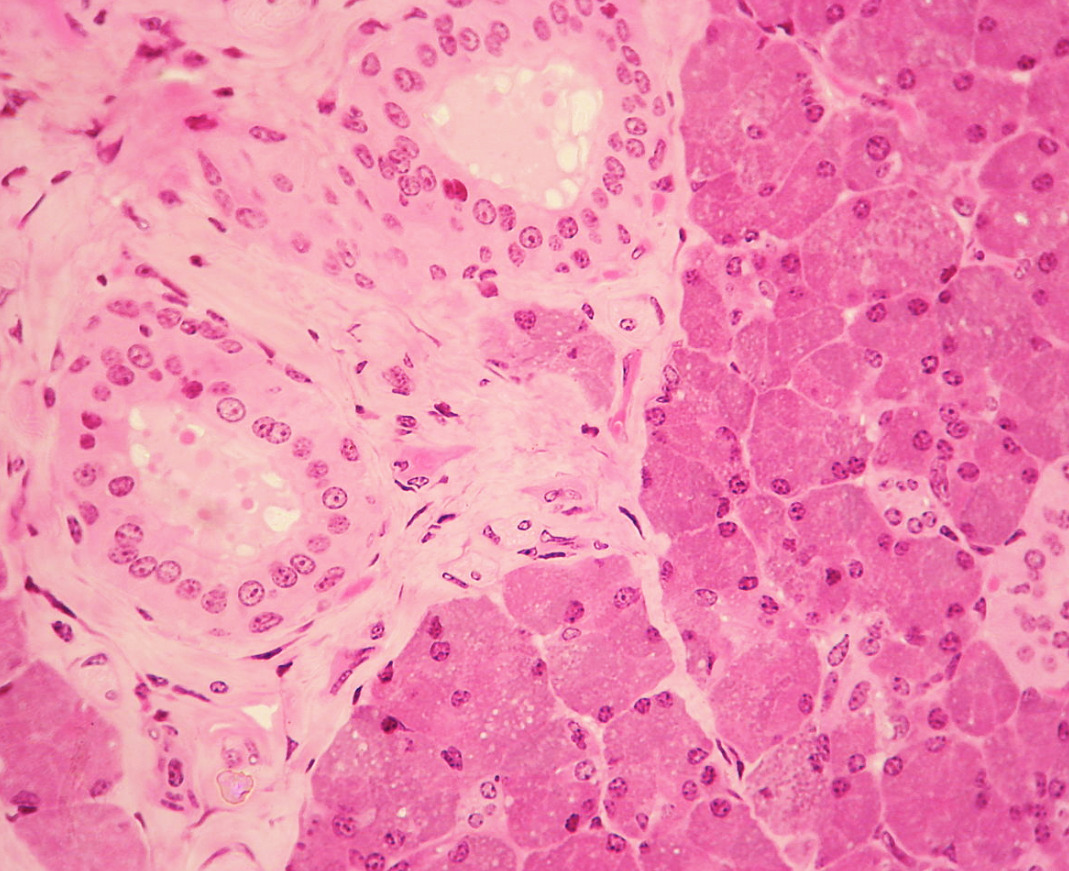
Histology of the parotid gland (serous acini)
Image: “Histology of the parotid gland” by Wbensmith. License: CC BY 3.0