Abdominal and cardiac evaluation with sonography Sonography The visualization of deep structures of the body by recording the reflections or echoes of ultrasonic pulses directed into the tissues. Use of ultrasound for imaging or diagnostic purposes employs frequencies ranging from 1. 6 to 10 megahertz. Diagnostic Procedures in Gynecology in shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock (ACES) and rapid ultrasound for shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock and hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension (RUSH) are point-of-care ultrasound Point-Of-Care Ultrasound Focused Assessment with Sonography for Trauma (FAST) ( POCUS POCUS Focused Assessment with Sonography for Trauma (FAST)) examinations indicated in cases of nontraumatic, undifferentiated hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, or shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock. In hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, early diagnosis and goal-directed therapy are essential for optimal outcomes and lead to decreased mortality Mortality All deaths reported in a given population. Measures of Health Status. Both ACES and RUSH protocols examine the chest and abdominal cavities by ultrasound in order to rapidly evaluate for reversible causes of shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock and improve an accurate diagnosis. Each of these protocols combines many of the same core ultrasound elements, differing mainly in the exam sequence.
Last updated: Apr 11, 2023
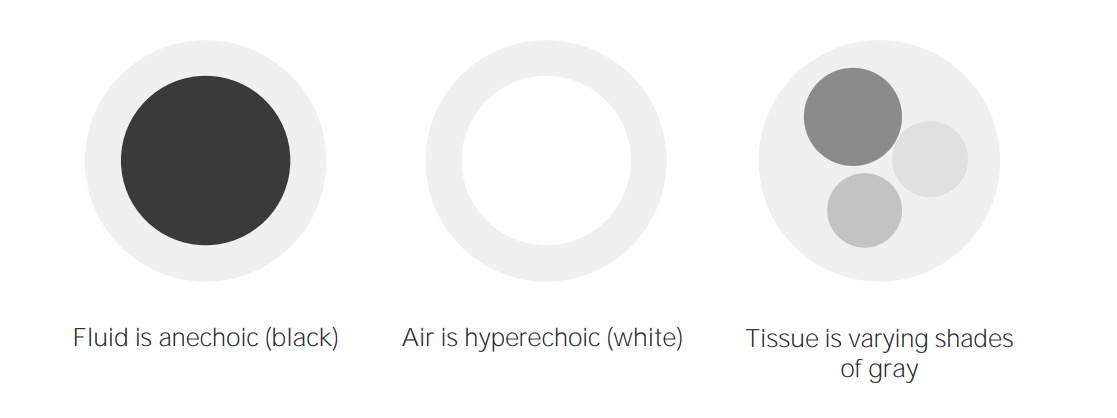
Imaging concepts of ultrasound
Image by Lecturio. License: CC BY-NC-SA 4.0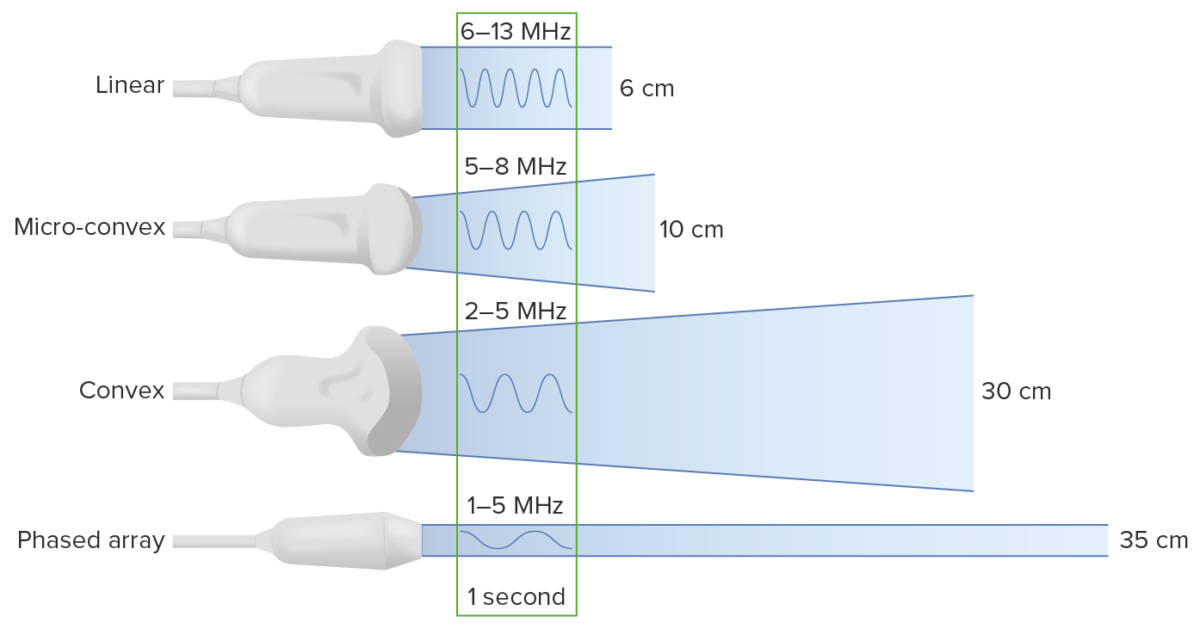
Types of transducers:
Note that decreasing the frequency increases the depth to which the ultrasound wave travels. However, this comes at the cost of image resolution.
Image showing the ultrasound machine and different probes
Image: “Photos of a sonography system and typical transducers.” by Kieran Maher. License: Public DomainAbdominal and cardiac evaluation with sonography Sonography The visualization of deep structures of the body by recording the reflections or echoes of ultrasonic pulses directed into the tissues. Use of ultrasound for imaging or diagnostic purposes employs frequencies ranging from 1. 6 to 10 megahertz. Diagnostic Procedures in Gynecology in shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock is a POCUS POCUS Focused Assessment with Sonography for Trauma (FAST) examination exam used in cases of nontraumatic undifferentiated hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension performed in the ER.

Abdominal and cardiac evaluation with sonography in shock (ACES) protocol:
1: 1 or more cardiac views
2: Inferior vena cava view
3: Screen of the abdominal aorta
4: Right and 5: Left flank views for pleural and peritoneal fluid
6: Pelvic view for bladder size and free fluid
| Type of shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock | Cardiac | IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy | Aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy | Peritoneal fluid/blood | Pleural fluid/blood |
|---|---|---|---|---|---|
| Septic | Hyperdynamic LV or hypodynamic in late sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock | Narrow/collapsed IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy | Normal | Surgical/gynecological sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock | Pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia, empyema Empyema Presence of pus in a hollow organ or body cavity. Pneumonia |
| Cardiogenic | Hypodynamic LV/↓ EF EF Cardiac Cycle | Normal | Normal | Normal | Normal |
| Hypovolemic | Hyperdynamic LV | Narrow/collapsed IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy | AAA AAA An aortic aneurysm is the abnormal dilation of a segment of the aorta. Abdominal aortic aneurysm is the most common aortic aneurysm, occurring frequently in the infrarenal area. Most aneurysms are asymptomatic, but can cause compression of surrounding structures or rupture, which is a life-threatening emergency. Abdominal Aortic Aneurysms | Spontaneous splenic rupture Splenic rupture Splenic rupture is a medical emergency that carries a significant risk of hypovolemic shock and death. Injury to the spleen accounts for nearly half of all injuries to intra-abdominal organs. The most common reason for a rupture of the spleen is blunt abdominal trauma, specifically, motor vehicle accidents. Rupture of the Spleen, perforated viscous, gynecological bleeding | Normal |
| Obstructive (cardiac) | Pericardial effusion Pericardial effusion Fluid accumulation within the pericardium. Serous effusions are associated with pericardial diseases. Hemopericardium is associated with trauma. Lipid-containing effusion (chylopericardium) results from leakage of thoracic duct. Severe cases can lead to cardiac tamponade. Pericardial Effusion and Cardiac Tamponade, cardiac tamponade Tamponade Pericardial effusion, usually of rapid onset, exceeding ventricular filling pressures and causing collapse of the heart with a markedly reduced cardiac output. Pericarditis | Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy | Normal | Normal | Normal |
| Obstructive (pulmonary) | Dilated RV, ↑ LV to RV ratio | Dilated IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy | Normal | Normal | Normal |
Rapid ultrasound for shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock and hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension is a POCUS POCUS Focused Assessment with Sonography for Trauma (FAST) examination protocol that focuses on assessment of the heart and major vessels that is divided into 3 steps: “pump,” “tank,” and “pipes.”

Probe placement for the rapid ultrasound for shock and hypotension (RUSH) exam
Image by Lecturio.| Type of shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock | Pump | Tank | Pipes |
|---|---|---|---|
| Cardiogenic | Hypodynamic LV, ↓ EF EF Cardiac Cycle, dilated heart | Dilated IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy, distended jugular veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology, lung rockets, pleural fluid, peritoneal fluid | Normal |
| Hypovolemic | Hyperdynamic LV, small chamber size | Narrow IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy, flat jugular veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology, peritoneal fluid, pleural fluid | Normal |
| Obstructive | Hyperdynamic LV, pericardial effusion Pericardial effusion Fluid accumulation within the pericardium. Serous effusions are associated with pericardial diseases. Hemopericardium is associated with trauma. Lipid-containing effusion (chylopericardium) results from leakage of thoracic duct. Severe cases can lead to cardiac tamponade. Pericardial Effusion and Cardiac Tamponade, cardiac tamponade Tamponade Pericardial effusion, usually of rapid onset, exceeding ventricular filling pressures and causing collapse of the heart with a markedly reduced cardiac output. Pericarditis, RV strain, cardiac thrombus | Dilated IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy, distended jugular veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology, absent lung sliding ( pneumothorax Pneumothorax A pneumothorax is a life-threatening condition in which air collects in the pleural space, causing partial or full collapse of the lung. A pneumothorax can be traumatic or spontaneous. Patients present with a sudden onset of sharp chest pain, dyspnea, and diminished breath sounds on exam. Pneumothorax) | DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis |
| Distributive | Hyperdynamic LV in early sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock, hypodynamic LV in late sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock | Normal/small IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy (early sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock), peritoneal fluid ( sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock), pleural fluid ( sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock) | Normal |