Pericarditis is an inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the pericardium Pericardium A conical fibroserous sac surrounding the heart and the roots of the great vessels (aorta; venae cavae; pulmonary artery). Pericardium consists of two sacs: the outer fibrous pericardium and the inner serous pericardium. The latter consists of an outer parietal layer facing the fibrous pericardium, and an inner visceral layer (epicardium) resting next to the heart, and a pericardial cavity between these two layers. Heart: Anatomy, often with fluid accumulation. It can be caused by infection (often viral), myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, drugs, malignancies, metabolic disorders, autoimmune disorders, or trauma. Acute, subacute, and chronic forms exist. Acute pericarditis is usually idiopathic Idiopathic Dermatomyositis and manifests as fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, pleuritic chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, and an audible pericardial rub by auscultation. Diffuse upwardly concave ST-segment elevations in the initial ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) and pericardial effusion Pericardial effusion Fluid accumulation within the pericardium. Serous effusions are associated with pericardial diseases. Hemopericardium is associated with trauma. Lipid-containing effusion (chylopericardium) results from leakage of thoracic duct. Severe cases can lead to cardiac tamponade. Pericardial Effusion and Cardiac Tamponade on echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA) confirm the diagnosis. Acute pericarditis is usually self-limiting Self-Limiting Meningitis in Children (2–6 weeks); therefore, management is conservative. If cardiac tamponade Cardiac tamponade Compression of the heart by accumulated fluid (pericardial effusion) or blood (hemopericardium) in the pericardium surrounding the heart. The affected cardiac functions and cardiac output can range from minimal to total hemodynamic collapse. Pericardial Effusion and Cardiac Tamponade or constrictive pericarditis develops, cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics can be severely reduced. Treatment depends on the cause, but general measures include analgesics, anti-inflammatory drugs, colchicine Colchicine A major alkaloid from colchicum autumnale l. And found also in other colchicum species. Its primary therapeutic use is in the treatment of gout. Gout Drugs, and rarely surgery.
For Clinical Practice Version: Click here
Last updated: May 16, 2024
Definition
Pericarditis is an inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the pericardium Pericardium A conical fibroserous sac surrounding the heart and the roots of the great vessels (aorta; venae cavae; pulmonary artery). Pericardium consists of two sacs: the outer fibrous pericardium and the inner serous pericardium. The latter consists of an outer parietal layer facing the fibrous pericardium, and an inner visceral layer (epicardium) resting next to the heart, and a pericardial cavity between these two layers. Heart: Anatomy, the double-layered sac surrounding the heart.
Clinical classification is based on duration.
| Idiopathic Idiopathic Dermatomyositis (most common) | After exclusion of other causes |
|---|---|
| Viral infection |
|
| Bacterial infection |
|
| Fungal infection (very rare) |
|
| Autoimmune disease |
|
| Metabolic |
|
| Cardiovascular |
|
| Cancer |
|
| Drugs |
|
| Features | Acute | Chronic | Constrictive |
|---|---|---|---|
| Pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways |
|
|
None |
| Other symptoms |
|
May have dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea |
|
| Physical examination |
|
|
|
| ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) |
|
Electrical alternans Electrical alternans Consecutive QRS complexes that alternate in height. A motion artifact due to the pendular swinging of the heart within the pericardial space. Seen in large pericardial effusion or cardiac tamponade. Pericardial Effusion and Cardiac Tamponade7 with a large effusion |
|
| Echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA)8 | Pleural effusion Pleural Effusion Pleural effusion refers to the accumulation of fluid between the layers of the parietal and visceral pleura. Common causes of this condition include infection, malignancy, autoimmune disorders, or volume overload. Clinical manifestations include chest pain, cough, and dyspnea. Pleural Effusion | Pleural effusion Pleural Effusion Pleural effusion refers to the accumulation of fluid between the layers of the parietal and visceral pleura. Common causes of this condition include infection, malignancy, autoimmune disorders, or volume overload. Clinical manifestations include chest pain, cough, and dyspnea. Pleural Effusion | Pericardial thickening |
| Tamponade9 | With rapid fluid accumulation | Uncommon | Never |
| Comments | Elevated cardiac biomarkers can occur, further simulating a diagnosis of acute MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction. |
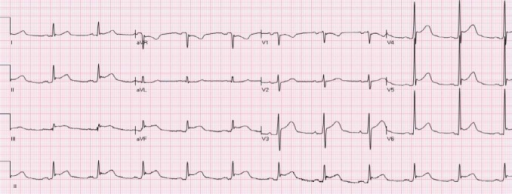
ECG showing diffuse ST-segment elevation with upward concavity without T-wave inversions in a patient with acute pericarditis
Image: “Diffuse STE in leads I, II, III, aVF, V2-V6 with ST depression in leads aVR and V1, compatible with acute pericarditis” by Department of Medicine, Baylor College of Medicine, Houston, Texas 77030, USA. License: CC BY 3.0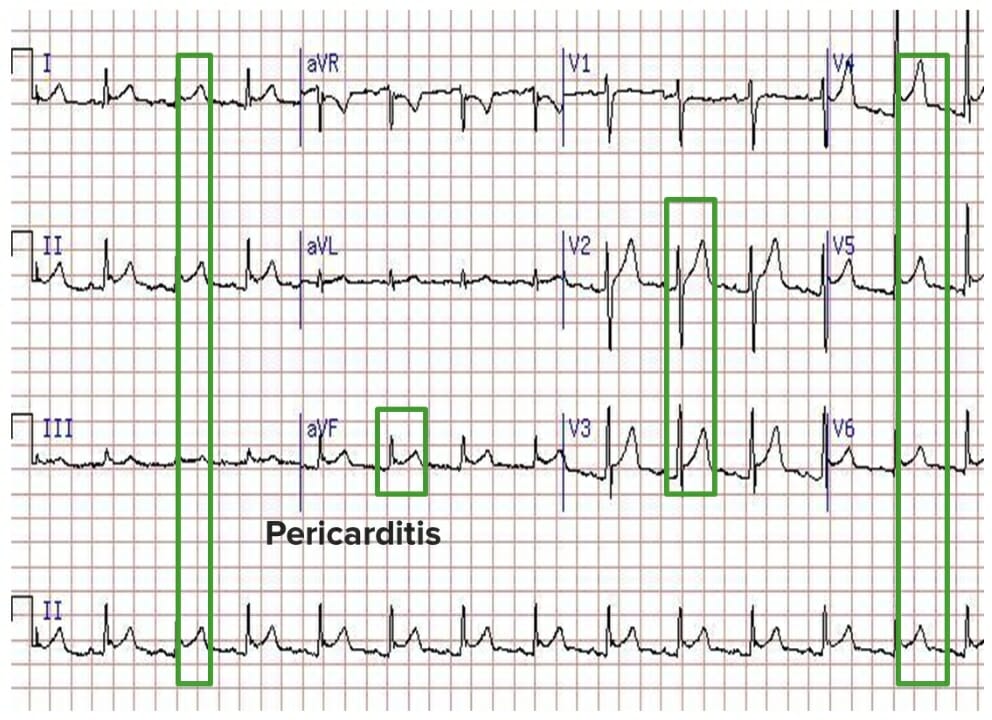
ECG showing diffuse ST segment elevation and the absence of reciprocal ST segment depression
Image by Lecturio.