Meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the membranes ( meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy) that surround the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy. The majority of cases occur during childhood and are predominantly viral or bacterial in etiology. Clinical presentation is influenced by the age of the child and the causative pathogen, but meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis typically presents with signs of meningeal irritation Meningeal Irritation Subarachnoid Hemorrhage, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, and lethargy Lethargy A general state of sluggishness, listless, or uninterested, with being tired, and having difficulty concentrating and doing simple tasks. It may be related to depression or drug addiction. Hyponatremia. Management varies depending on the pathogen isloated from the CSF. Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is dependent on the causative pathogen and appropriate timely intervention. Bacterial meningitis Bacterial meningitis Bacterial infections of the leptomeninges and subarachnoid space, frequently involving the cerebral cortex, cranial nerves, cerebral blood vessels, spinal cord, and nerve roots. Meningitis can be life-threatening and has severe complications that may result in long-term sequelae.
Last updated: Mar 29, 2023
Meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the membranes, or meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy, surrounding the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy and brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification.
| Bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology | Viruses Viruses Minute infectious agents whose genomes are composed of DNA or RNA, but not both. They are characterized by a lack of independent metabolism and the inability to replicate outside living host cells. Virology | Fungi Fungi A kingdom of eukaryotic, heterotrophic organisms that live parasitically as saprobes, including mushrooms; yeasts; smuts, molds, etc. They reproduce either sexually or asexually, and have life cycles that range from simple to complex. Filamentous fungi, commonly known as molds, refer to those that grow as multicellular colonies. Mycology |
|---|---|---|
Newborns:
|
|
|
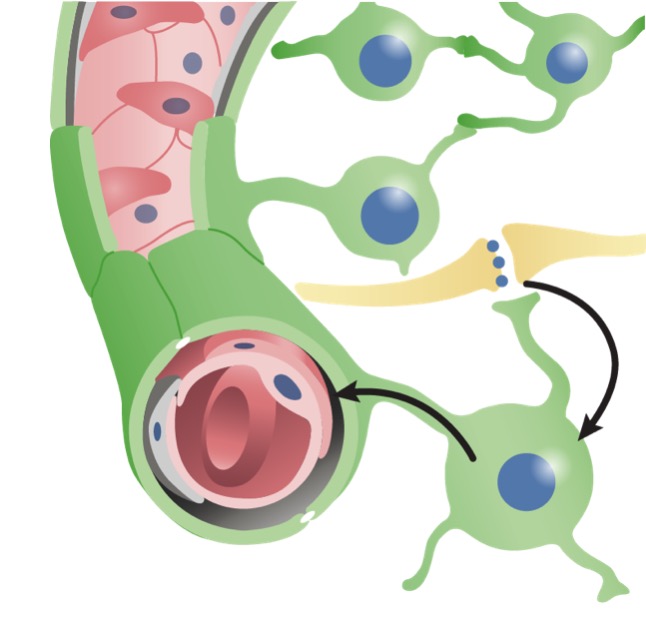
The blood–brain barrier:
Capillaries in the blood–brain barrier and how neurons connect to the vessels
Cell depiction of the blood–brain barrier:
Left: cell layers of the blood vessels
Right: axons of neural cell against the blood capillaries
Clinical presentation in infants and newborns tends to be very nonspecific; therefore, there should be a high index of suspicion for meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis in all infants and newborns who appear ill.
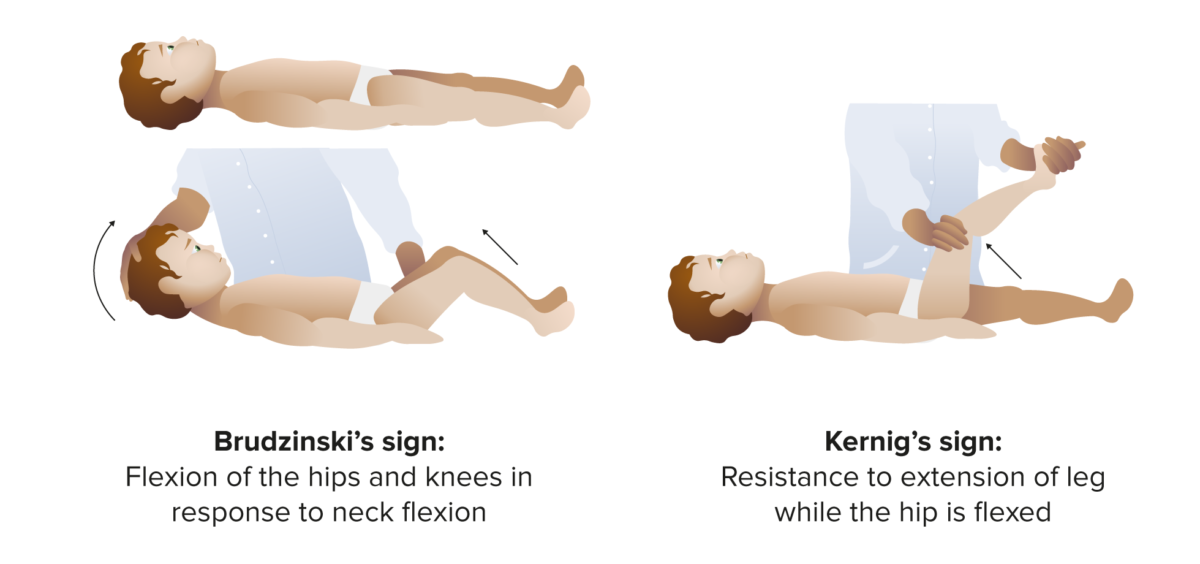
Positive clinical examination findings for meningitis
Image by Lecturio.A diagnosis of meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis is based on clinical findings and confirmed with positive findings in the CSF.
| CSF Gram stain Gram stain Klebsiella | High false-negatives, low false-positives |
|---|---|
| CSF protein | In bacterial disease, usually > 80 |
| CSF glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance | In bacterial disease, usually < ⅔ serum glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance |
| CSF cell count |
|
| Cells/ mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma3 | Type of cell | Protein (mg/dl) | Glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance (mg/dl) | |
|---|---|---|---|---|
| Normal CSF | < 10 | Mononuclear (MN) | < 45 | 35–100 |
| Bacterial meningitis Bacterial meningitis Bacterial infections of the leptomeninges and subarachnoid space, frequently involving the cerebral cortex, cranial nerves, cerebral blood vessels, spinal cord, and nerve roots. Meningitis | > 1000 | PMC | > 80 | ↓ or < ⅔ of serum glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance |
| Viral meningitis Viral meningitis Viral infections of the leptomeninges and subarachnoid space. Togaviridae infections; flaviviridae infections; rubella; bunyaviridae infections; orbivirus infections; picornaviridae infections; orthomyxoviridae infections; rhabdoviridae infections; arenaviridae infections; herpesviridae infections; adenoviridae infections; JC virus infections; and retroviridae infections may cause this form of meningitis. Clinical manifestations include fever, headache, neck pain, vomiting, photophobia, and signs of meningeal irritation. Meningitis | < 300 | First PMC, later MN | Normal or ↑ | Normal |

Inferior view of a brain infected with gram-negative Haemophilus influenzae bacteria
Image: “Haemophilus influenzae meningitis” by CDC. License: Public Domain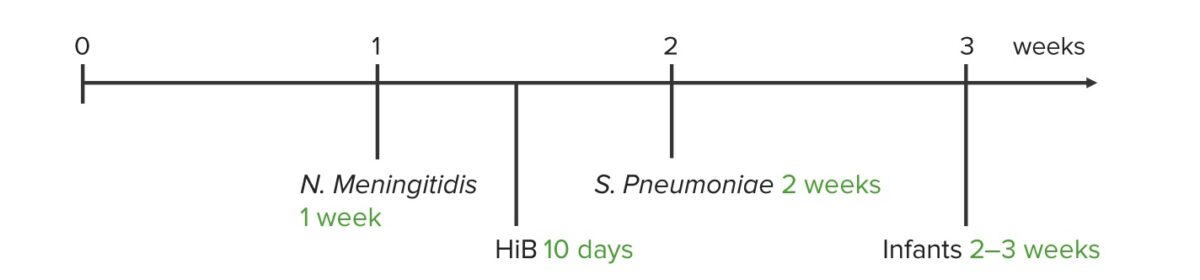
Usual time of antibiotic therapy required for different pathogens
Image by Lecturio.