Cryptococcosis is an opportunistic, fungal infection caused by the Cryptococcus species. The principal pathogens in humans are C. neoformans (primary) and C. gattii. Cryptococcus neoformans is typically found in pigeon droppings and acquired by inhaling dust from contaminated soil. The majority of affected patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with AIDS AIDS Chronic HIV infection and depletion of CD4 cells eventually results in acquired immunodeficiency syndrome (AIDS), which can be diagnosed by the presence of certain opportunistic diseases called AIDS-defining conditions. These conditions include a wide spectrum of bacterial, viral, fungal, and parasitic infections as well as several malignancies and generalized conditions. HIV Infection and AIDS, chronic steroid use, and organ transplant are particularly affected. The primary virulence Virulence The degree of pathogenicity within a group or species of microorganisms or viruses as indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. The pathogenic capacity of an organism is determined by its virulence factors. Proteus factor is an antiphagocytic capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides, consisting of repeating capsular polysaccharide antigens. The infection typically affects the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy and presents as a primary lesion or pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia. Dissemination can occur to involve the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, bones, and visceral organs. Treatment for cryptococcal meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis is usually amphotericin B Amphotericin B Macrolide antifungal antibiotic produced by streptomyces nodosus obtained from soil of the orinoco river region of venezuela. Polyenes and flucytosine Flucytosine Flucytosine is a pyrimidine analog that disrupts fungal DNA and RNA synthesis. Flucytosine is always used in combination with other antifungal agents and is primarily used to treat cryptococcal meningitis. Flucytosine, Griseofulvin, and Terbinafine, followed by fluconazole Fluconazole Triazole antifungal agent that is used to treat oropharyngeal candidiasis and cryptococcal meningitis in aids. Azoles. Cryptococcosis is an AIDS-defining illness and typically associated with CD4 count < 100 cells/μL.
Last updated: Mar 27, 2023
The most significant risk factor for infection is an immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis state. In decreasing frequency, the following conditions are most frequently associated with infection:
Clinical presentation varies depending on the affected area and immune status of the host:

Cutaneous cryptococcosis: Papulonodular lesions (some showing crusts and umbilicated center) are on the face and upper dorsum. Cryptococcus infection is confirmed in the skin lesions.
Image: “Disseminated cryptococcosis with cutaneous involvement in an immunocompetent patient” by Gabriely Lessa Sacht et al. License: CC BY 4.0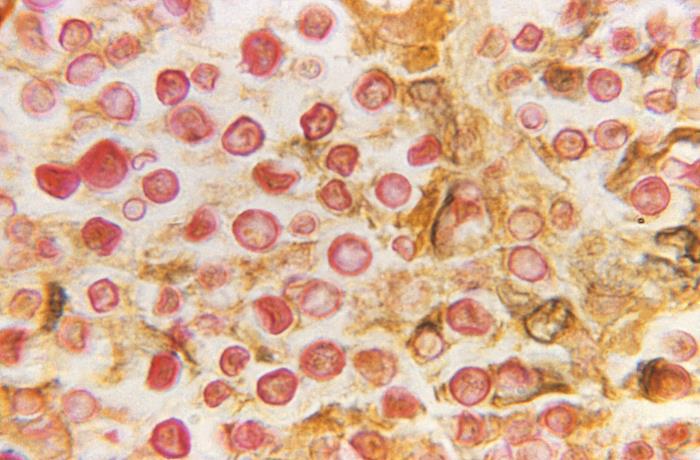
Photomicrograph of Cryptococcus neoformans processed using the mucicarmine stain:
The polysaccharide in the C. neoformans capsule created a prominent red stain.
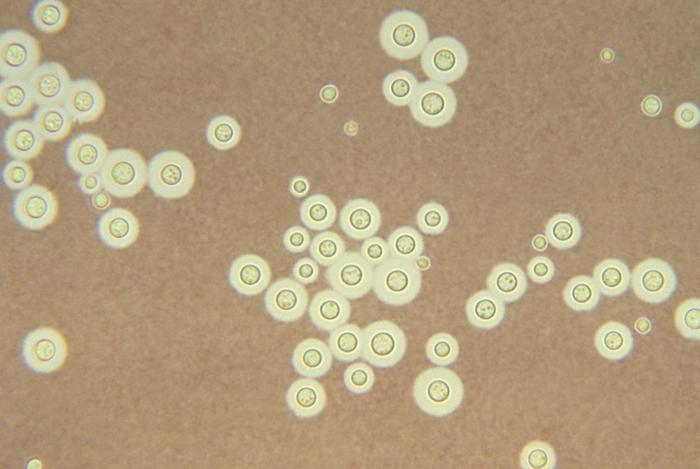
Histological image showing Cryptococcus neoformans stained with India ink: The appearance of a halo surrounding each yeast cell represents the observable capsule.
Image: “Cryptococcus neoformans” by CDC/ Dr. Leanor Haley. License: Public Domain
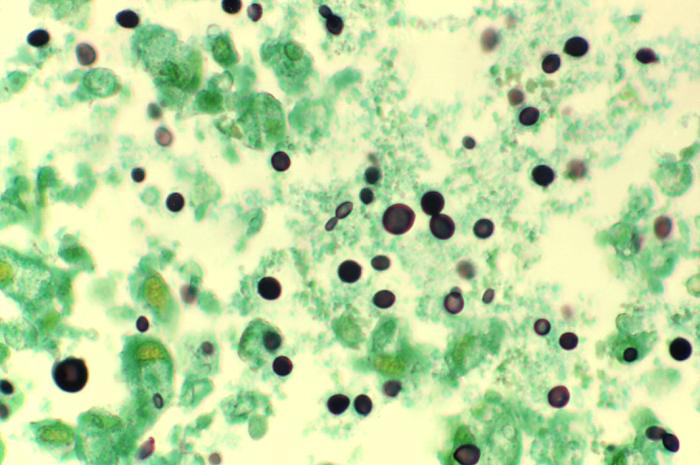
Photomicrograph of a methenamine-stained lung tissue specimen harvested from a patient with acquired immunodeficiency syndrome (AIDS) infected with Cryptococcus:
Histopathology reveals numerous extracellular C. neoformans yeast-form organisms within the alveolar space. Some of the yeast organisms show narrow-base budding and characteristic variation in size.
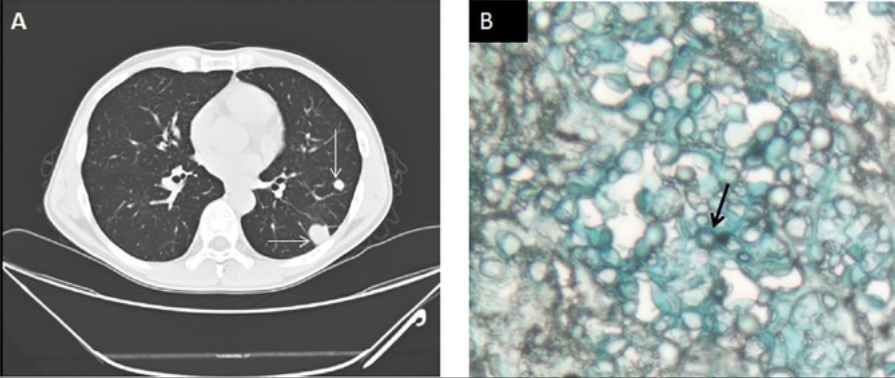
Pulmonary cryptococcosis:
A 49-year-old man presenting to the hospital with lymphadenopathy for 3 months, fever for 1 month, and HIV infection with a CD4 count of 108 cells/μL. Serum cryptococcal antigen titer was 1:40. Serum galactomannan assay was negative.
A: chest CT scan demonstrating multiple pulmonary nodules (arrow)
B: lung biopsy showing encapsulated, yeast-like fungal cells consistent with cryptococcal infection (arrow) in alcian blue stain
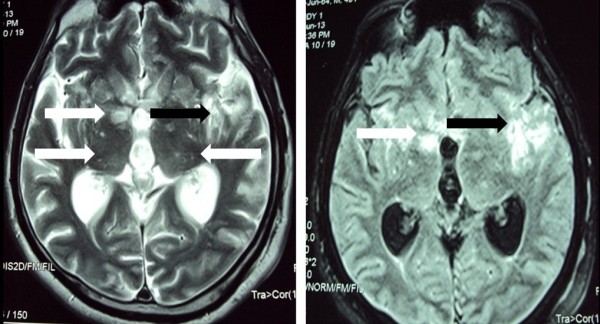
Magnetic resonance imaging (MRI) of the brain showing T2-weighted images (left) and fluid attenuated inversion recovery (FLAIR) (right): bilateral, multiple nodular lesions in the basal ganglia and thalamus (white arrows), and ill-defined area of signal intensity change in the left temporoparietal region (black arrows)
Image: “Cryptococcal meningitis presenting with bilateral complete ophthalmoplegia: a case report” by Liyanage DS et al. License: CC BY 2.0| Condition | Treatment |
|---|---|
| CNS infection | Amphotericin B Amphotericin B Macrolide antifungal antibiotic produced by streptomyces nodosus obtained from soil of the orinoco river region of venezuela. Polyenes + flucytosine Flucytosine Flucytosine is a pyrimidine analog that disrupts fungal DNA and RNA synthesis. Flucytosine is always used in combination with other antifungal agents and is primarily used to treat cryptococcal meningitis. Flucytosine, Griseofulvin, and Terbinafine, followed by consolidation Consolidation Pulmonary Function Tests and maintenance therapy |
| Immunocompetent and immunosuppressed with mild pulmonary infection (focal) | Fluconazole Fluconazole Triazole antifungal agent that is used to treat oropharyngeal candidiasis and cryptococcal meningitis in aids. Azoles |
| Immunocompetent and immunosuppressed with severe pulmonary infection | CNS infection treatment |
| Immunocompetent and immunosuppressed with extrapulmonary, non-CNS infection (≥ 2 noncontiguous sites) | CNS infection treatment |