Type IV hypersensitivity reaction, or delayed-type hypersensitivity, is a cell-mediated response to antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination exposure. The reaction involves T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified - cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions, not antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions, and develops over several days. Presensitized T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified - cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions initiate the immune defense, leading to tissue damage. A cytokine-mediated process is activated by T-helper cells while cytotoxic Cytotoxic Parvovirus B19 T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified - cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions directly release cytotoxins Cytotoxins Substances that are toxic to cells; they may be involved in immunity or may be contained in venoms. These are distinguished from cytostatic agents in degree of effect. Some of them are used as cytotoxic antibiotics. The mechanism of action of many of these are as alkylating agents or mitosis modulators. Helicobacter to infected or dysfunctional cells, causing cell lysis. Clinical manifestations depend on the system involved, so diagnostic tests Diagnostic tests Diagnostic tests are important aspects in making a diagnosis. Some of the most important epidemiological values of diagnostic tests include sensitivity and specificity, false positives and false negatives, positive and negative predictive values, likelihood ratios, and pre-test and post-test probabilities. Epidemiological Values of Diagnostic Tests rely on history and findings. Treatment includes controlling the effects of the immune response with glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids and immunosuppressive therapy while managing the associated disease complications.
Last updated: Nov 23, 2024
Sensitization phase
Effector phase
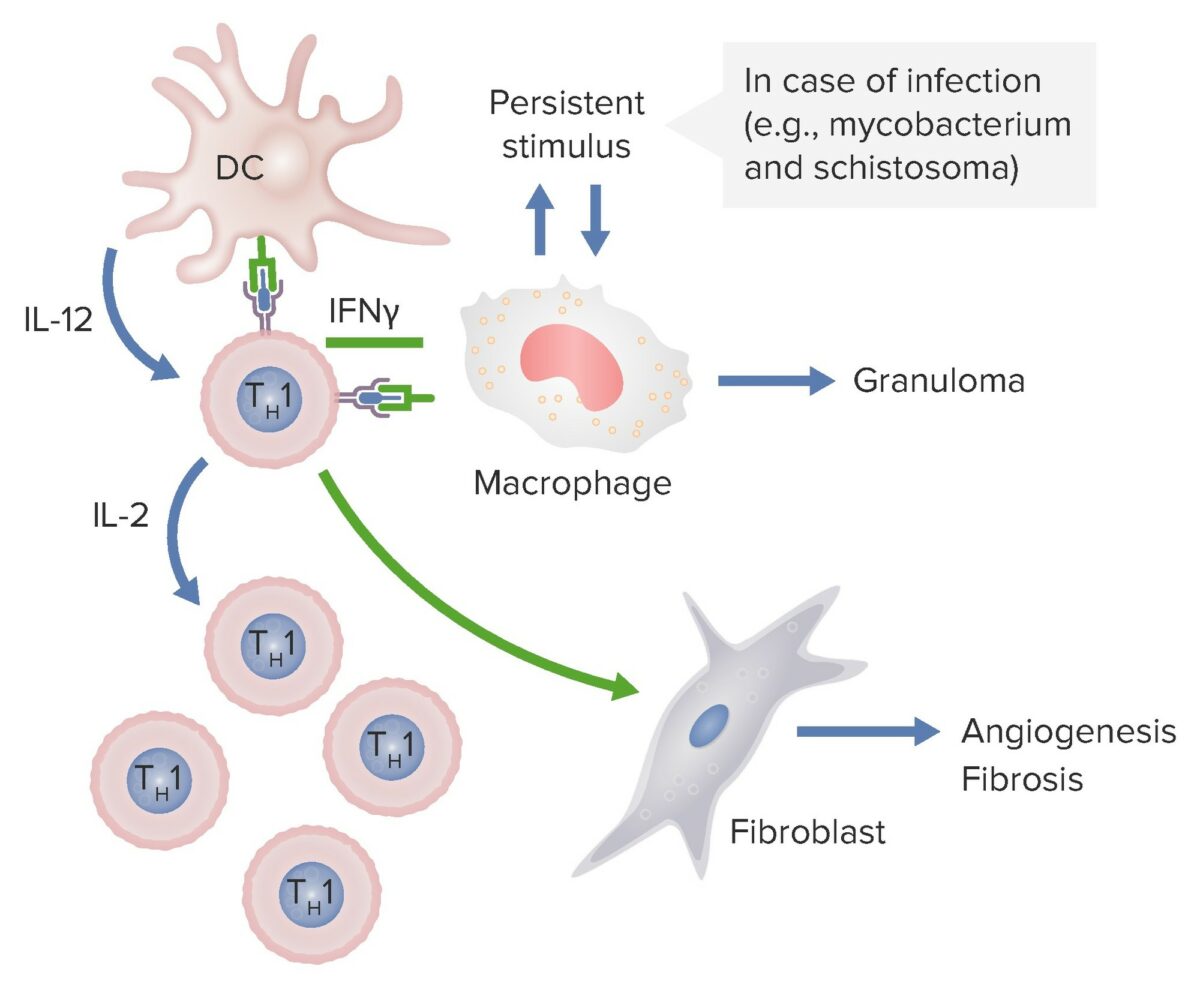
In the above diagram, dendritic cells are releasing IL-12 which activates CD4 Th1 cells. These Th1 cells produce IL-2 stimulating production of more Th1 T cell subsets. Th cells also release IFN-γ which activates macrophages and activates fibroblasts to cause angiogenesis and fibrosis. If these macrophages are persistently stimulated by pathogens such as mycobacterium and schistosoma, granulomas are formed.
Image by Lecturio.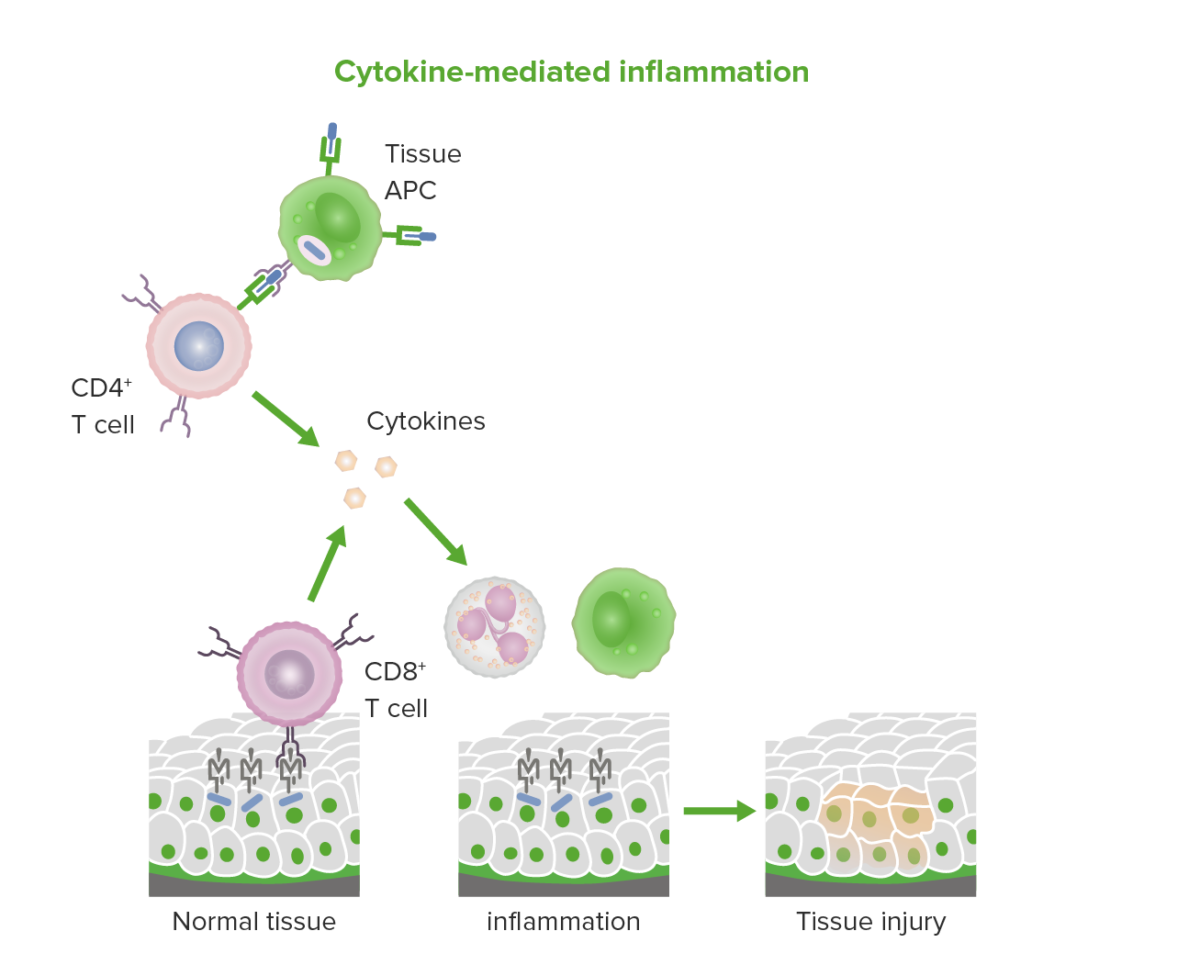
Cytokine-mediated and cytotoxic T cell-mediated inflammation in type IV hypersensitivity.
Image by Lecturio.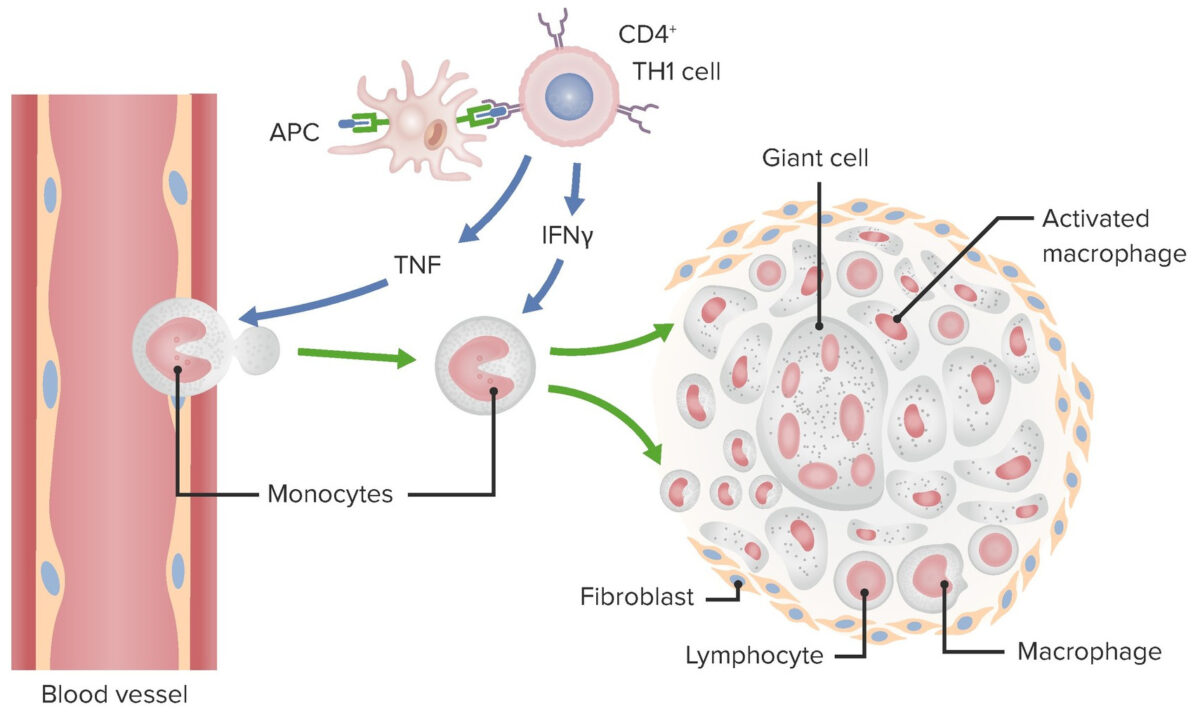
Granuloma Mechanism in Type IV hypersensitivity.
Image by Lecturio.| Disease | Target antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination | Effects |
|---|---|---|
| Allergic contact dermatitis Contact dermatitis A type of acute or chronic skin reaction in which sensitivity is manifested by reactivity to materials or substances coming in contact with the skin. It may involve allergic or non-allergic mechanisms. Male Genitourinary Examination | Environmental chemicals such as urushiol Urushiol Toxicology of Plants (from poison ivy and poison oak), metals (e.g., nickel), topical medication | Epidermal necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage, inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions rash Rash Rocky Mountain Spotted Fever, and blisters |
| Autoimmune myocarditis Myocarditis Myocarditis is an inflammatory disease of the myocardium, which may occur alone or in association with a systemic process. There are numerous etiologies of myocarditis, but all lead to inflammation and myocyte injury, most often leading to signs and symptoms of heart failure. Myocarditis | Myosin Myosin A diverse superfamily of proteins that function as translocating proteins. They share the common characteristics of being able to bind actins and hydrolyze mgATP. Myosins generally consist of heavy chains which are involved in locomotion, and light chains which are involved in regulation. Within the structure of myosin heavy chain are three domains: the head, the neck and the tail. The head region of the heavy chain contains the actin binding domain and mgATPase domain which provides energy for locomotion. The neck region is involved in binding the light-chains. The tail region provides the anchoring point that maintains the position of the heavy chain. The superfamily of myosins is organized into structural classes based upon the type and arrangement of the subunits they contain. Skeletal Muscle Contraction heavy chain protein | Cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types |
| Diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus type I | Pancreatic beta cell proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis (possibly insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin, glutamate Glutamate Derivatives of glutamic acid. Included under this heading are a broad variety of acid forms, salts, esters, and amides that contain the 2-aminopentanedioic acid structure. Synthesis of Nonessential Amino Acids decarboxylase) | Insulitis, beta cell destruction |
| Granulomas Granulomas A relatively small nodular inflammatory lesion containing grouped mononuclear phagocytes, caused by infectious and noninfectious agents. Sarcoidosis | Various, depending on the underlying disease | Walled-off lesion containing macrophages Macrophages The relatively long-lived phagocytic cell of mammalian tissues that are derived from blood monocytes. Main types are peritoneal macrophages; alveolar macrophages; histiocytes; kupffer cells of the liver; and osteoclasts. They may further differentiate within chronic inflammatory lesions to epithelioid cells or may fuse to form foreign body giant cells or langhans giant cells. Innate Immunity: Phagocytes and Antigen Presentation and other cells |
| Some peripheral neuropathies Neuropathies Chédiak-Higashi Syndrome | Schwann cell Schwann Cell Neuroglial cells of the peripheral nervous system which form the insulating myelin sheaths of peripheral axons. Nervous System: Histology antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination | Neuritis, paralysis |
| Hashimoto’s thyroiditis Thyroiditis Thyroiditis is a catchall term used to describe a variety of conditions that have inflammation of the thyroid gland in common. It includes pathologies that cause an acute illness with severe thyroid pain (e.g., subacute thyroiditis and infectious thyroiditis) as well as conditions in which there is no clinically evident inflammation and the manifestations primarily reflect thyroid dysfunction or a goiter (e.g., painless thyroiditis and fibrous Riedel’s thyroiditis). Thyroiditis | Thyroglobulin Thyroglobulin Thyroid Hormones antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination | Hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto’s disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism, hard goiter Goiter A goiter is a chronic enlargement of the thyroid gland due to nonneoplastic growth occurring in the setting of hypothyroidism, hyperthyroidism, or euthyroidism. Morphologically, thyroid enlargement can be diffuse (smooth consistency) or nodular (uninodular or multinodular). Goiter, follicular thymitis |
| Inflammatory bowel disease | Enteric microbiota and/or self-antigens | Hyperactivation of T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions, cytokine release, recruitment Recruitment Skeletal Muscle Contraction of macrophages Macrophages The relatively long-lived phagocytic cell of mammalian tissues that are derived from blood monocytes. Main types are peritoneal macrophages; alveolar macrophages; histiocytes; kupffer cells of the liver; and osteoclasts. They may further differentiate within chronic inflammatory lesions to epithelioid cells or may fuse to form foreign body giant cells or langhans giant cells. Innate Immunity: Phagocytes and Antigen Presentation and other immune cells, inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation |
| Multiple sclerosis Sclerosis A pathological process consisting of hardening or fibrosis of an anatomical structure, often a vessel or a nerve. Wilms Tumor | Myelin antigens (e.g., myelin basic protein) | Myelin destruction, inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation |
| Rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis | Possibly collagen Collagen A polypeptide substance comprising about one third of the total protein in mammalian organisms. It is the main constituent of skin; connective tissue; and the organic substance of bones (bone and bones) and teeth (tooth). Connective Tissue: Histology and/or citrullinated self-proteins | Chronic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis, inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, destruction of articular cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology and bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types |
| Tuberculin reaction (Mantoux test) | Tuberculin | Induration Induration Dermatologic Examination and erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion around injection site indicates previous exposure |

A case of Stevens-Johnson syndrome after antibiotic use, showing erythematous rash with flaccid blisters
Image: “Erythematous rash with flaccid blisters affecting the trunk” by Neila Fathallah et al. License: CC BY 4.0Allergic contact dermatitis Contact dermatitis A type of acute or chronic skin reaction in which sensitivity is manifested by reactivity to materials or substances coming in contact with the skin. It may involve allergic or non-allergic mechanisms. Male Genitourinary Examination (ACD)
Tuberculosis Tuberculosis Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis complex bacteria. The bacteria usually attack the lungs but can also damage other parts of the body. Approximately 30% of people around the world are infected with this pathogen, with the majority harboring a latent infection. Tuberculosis spreads through the air when a person with active pulmonary infection coughs or sneezes. Tuberculosis
Leprosy Leprosy Leprosy, also known as Hansen’s disease, is a chronic bacterial infection caused by Mycobacterium leprae complex bacteria. Symptoms primarily affect the skin and peripheral nerves, resulting in cutaneous manifestations (e.g., hypopigmented macules) and neurologic manifestations (e.g., loss of sensation). Leprosy
Sarcoidosis Sarcoidosis Sarcoidosis is a multisystem inflammatory disease that causes noncaseating granulomas. The exact etiology is unknown. Sarcoidosis usually affects the lungs and thoracic lymph nodes, but it can also affect almost every system in the body, including the skin, heart, and eyes, most commonly. Sarcoidosis
Crohn’s disease
Autoimmune myocarditis Myocarditis Myocarditis is an inflammatory disease of the myocardium, which may occur alone or in association with a systemic process. There are numerous etiologies of myocarditis, but all lead to inflammation and myocyte injury, most often leading to signs and symptoms of heart failure. Myocarditis
Diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus type I
Drug hypersensitivity
Guillain-Barré syndrome Guillain-Barré syndrome Guillain-Barré syndrome (GBS), once thought to be a single disease process, is a family of immune-mediated polyneuropathies that occur after infections (e.g., with Campylobacter jejuni). Guillain-Barré Syndrome