Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion multiforme (EM) is an acute hypersensitivity reaction characterized by targetoid skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions with multiple rings and dusky centers. Lesions may be accompanied by systemic symptoms (e.g., fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever) and mucosal lesions (e.g., bullae). The majority of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with EM have a history of recent viral (especially herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology) or bacterial infection (usually Mycoplasma pneumoniae Mycoplasma pneumoniae Short filamentous organism of the genus mycoplasma, which binds firmly to the cells of the respiratory epithelium. It is one of the etiologic agents of non-viral primary atypical pneumonia in man. Mycoplasma). Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion multiforme is diagnosed clinically and treatment is directed toward removing the causative agent and alleviation of symptoms.
Last updated: May 17, 2024
Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion multiforme (EM) is a cell-mediated immune reaction (type IV reaction) directed against the antigens of the offending agent, which deposit in the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions.
| Classification | Etiologies | Examples |
|---|---|---|
| Infectious causes (most common, 90% of cases) | Bacterial |
|
| Viral |
|
|
| Fungal |
|
|
| Noninfectious causes | Drugs |
|
| Malignancy Malignancy Hemothorax |
|
|
| Miscellaneous |
|
Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion multiforme is classified based on the presence of mucosal lesions and systemic symptoms into EM minor and major.
| Cutaneous lesions | Mucosal involvement | Systemic symptoms | |
|---|---|---|---|
| EM minor | ✔ | ||
| EM major | ✔ | ✔ | ✔ |
Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion multiforme usually resolves spontaneously within 1 month, with no long-term sequelae. Rarely, EM may recur, up to 6 times/year for 10 years (usually associated with HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2 infection).

Target lesions with a regular, round shape and 3 concentric zones: a central, darker-red area; a paler pink zone; and a peripheral red ring
Image: “Erythema multiforme” by Pediatric Unit, Maternal & Infant Department, S. Chiara University-Hospital, Via Roma 67, Pisa 56126, Italy. License: CC BY 2.0, edited by Lecturio.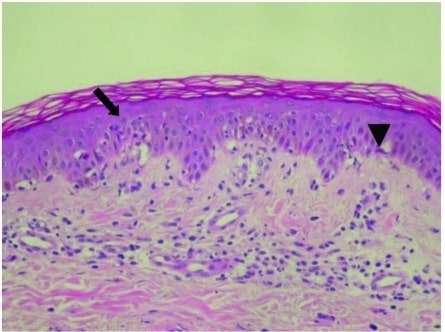
Epidermal changes in EM with vacuolated degeneration of basal cells (arrow) and scattered individual keratinocyte necrosis (arrowhead)
Image: “Epidermal Changes in Erythema Multiforme” by Division of Gastroenterology and Hepatology, Department of Internal Medicine, Taipei Medical University Hospital, Taipei, Taiwan. License: CC BY 2.5