Typhoid (or enteric) fever is a severe, systemic bacterial infection classically caused by the facultative intracellular and Gram-negative bacilli Salmonella enterica serotype Typhi (S. Typhimurium, formerly S. typhi). S. enterica serotype Paratyphi A, B, or C can cause a similar syndrome. Up to 20 million new cases of typhoid fever occur each year worldwide, most commonly in undeveloped areas with poor sanitation. Transmission occurs through the fecal-oral route, and humans are the only known reservoir. Complications of typhoid fever include intestinal hemorrhage, pericarditis, visceral abscesses, and septicemia. Treatment is dependent on patterns of antimicrobial resistance, but options include azithromycin and fluoroquinolones. Prevention of typhoid fever is available through vaccination, hand hygiene, and safe food and water practices.
Last updated: May 16, 2024
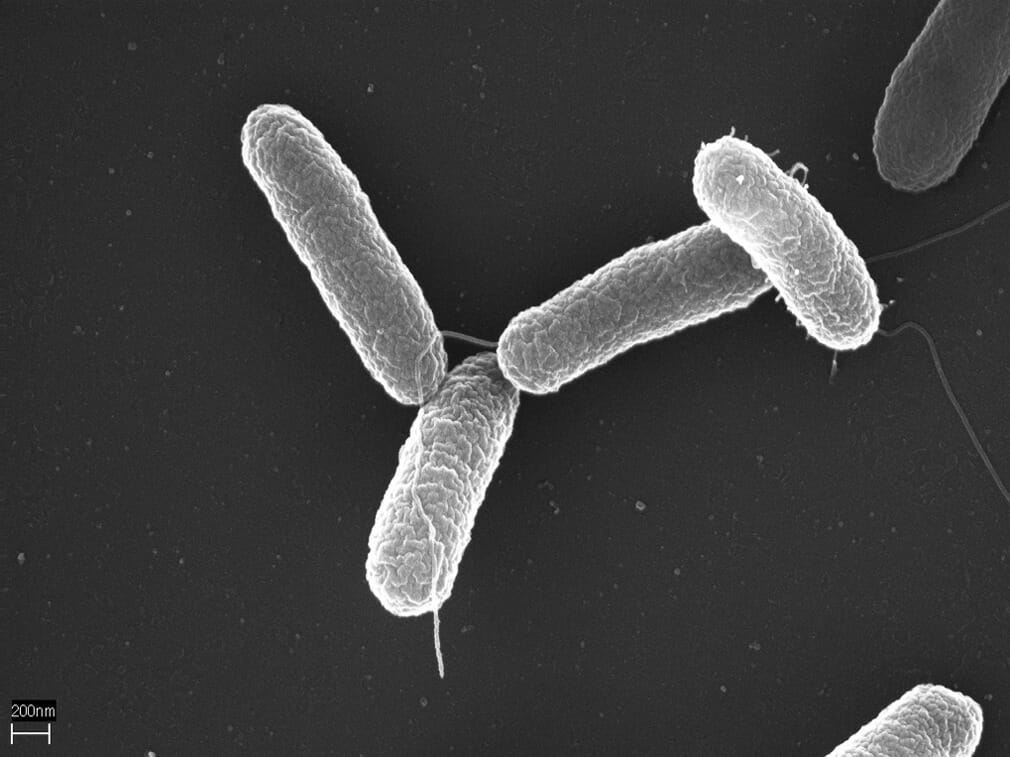
S. Typhimurium
Image: “Salmonella typhimurium“ by Volker Brinkmann, Max Planck Institute for Infection Biology, Berlin, Germany. License: CC BY 2.5After ingestion of Salmonella Salmonella Salmonellae are gram-negative bacilli of the family Enterobacteriaceae. Salmonellae are flagellated, non-lactose-fermenting, and hydrogen sulfide-producing microbes. Salmonella enterica, the most common disease-causing species in humans, is further classified based on serotype as typhoidal (S. typhi and paratyphi) and nontyphoidal (S. enteritidis and typhimurium). Salmonella Typhi:
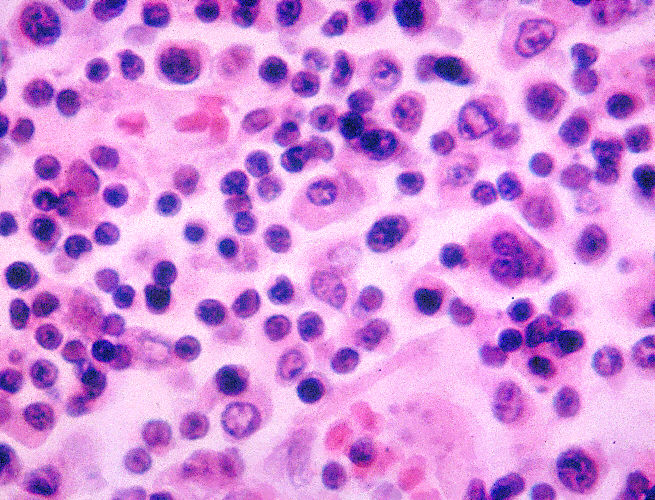
This photomicrograph reveals some of the histopathology exhibited in a lymph node tissue specimen in a case of typhoid fever. Macrophages are present amongst the normal lymphocytes. Note, S. Typhi bacterial invasion of macrophages. These macrophages also contain erythrocytes and degenerated lymphocytes.
Image: “2213” by CDC/ Armed Forces Institute of Pathology, Charles N. Farmer. License: Public DomainInfection with S. Typhi results in typhoid (or enteric ) fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever. Typhoid fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever is a severe systemic illness associated with fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever and abdominal pain Abdominal Pain Acute Abdomen.
The incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period is 5–21 days.
| Clinical course | Findings | |
|---|---|---|
| Week 1 | Bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides |
|
| Week 2 |
|
|
| Week 3 |
|
Clinical features of week 2 plus:
|

Rose-spot rash on the trunk of a patient with typhoid fever
Image: “2214” by CDC/Armed Forces Institute of Pathology, Charles N. Farmer. License: Public Domain
Rose-spot rash on the nose of a patient with typhoid fever
Image: “Nevus araneus (spider nevus)” by M. Sand, D. Sand et al. License: CC BY 2.0
Multiple ileal perforations in a patient with typhoid fever
Image: “Multiple typhoid ileal perforations” by Caronna R, Boukari AK et al. License: CC BY 2.0Diagnosis is dependent on a high degree of suspicion as cultures are often negative, take many days, and may not be available in resource-poor areas.
Complications of typhoid are typically associated with untreated infection in the 3rd phase (or week) of infection. The most common complications include:
Another complication, usually associated with asymptomatic infection, is developing a chronic carrier Carrier Vaccination state:
References