The anterior abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen is anatomically delineated as a hexagonal area defined superiorly by the xiphoid process Xiphoid process Chest Wall: Anatomy, laterally by the midaxillary lines, and inferiorly by the pubic symphysis Pubic Symphysis A slightly movable cartilaginous joint which occurs between the pubic bones. Vagina, Vulva, and Pelvic Floor: Anatomy. From the superficial to deep order, the anterior abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen consists of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, subcutaneous tissue Subcutaneous tissue Loose connective tissue lying under the dermis, which binds skin loosely to subjacent tissues. It may contain a pad of adipocytes, which vary in number according to the area of the body and vary in size according to the nutritional state. Soft Tissue Abscess, muscle, transversalis fascia Fascia Layers of connective tissue of variable thickness. The superficial fascia is found immediately below the skin; the deep fascia invests muscles, nerves, and other organs. Cellulitis, and peritoneum Peritoneum The peritoneum is a serous membrane lining the abdominopelvic cavity. This lining is formed by connective tissue and originates from the mesoderm. The membrane lines both the abdominal walls (as parietal peritoneum) and all of the visceral organs (as visceral peritoneum). Peritoneum: Anatomy. The lateral abdominal muscles include the external and internal obliques and the transversus abdominis. Anterior abdominal muscles include the rectus abdominis and pyramidalis muscles. The abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen is primarily supplied by epigastric arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology and innervated by thoracoabdominal nerves.
Last updated: Nov 18, 2024
The abdomen can be divided into 4 quadrants with the transverse and sagittal Sagittal Computed Tomography (CT) planes.
The abdomen can also be divided into 9 regions using the following planes:
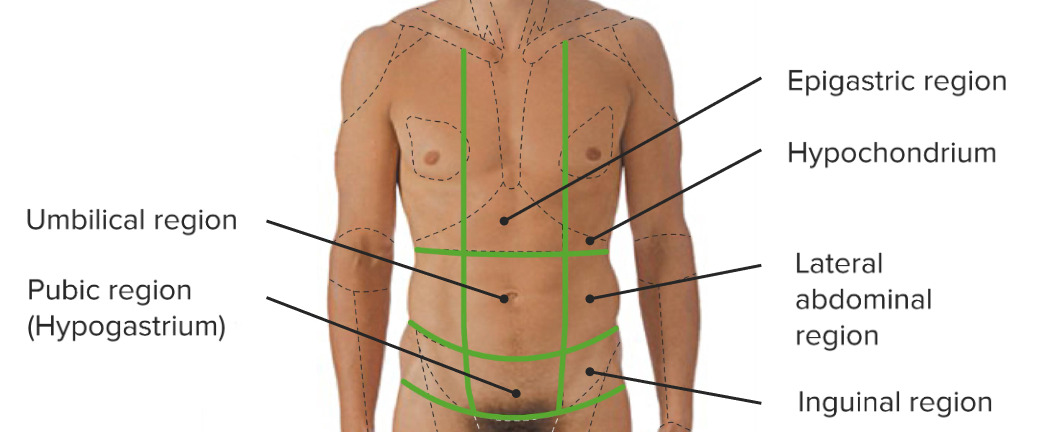
The 9 regions of the abdomen created by the vertical midclavicular and horizontal subcostal and transtubercular planes:
Note that the hypochondrium, lateral abdominal region, and inguinal region are present on both the left and right sides of the abdomen.
The layers of the anterior abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen from superficial to deep are:
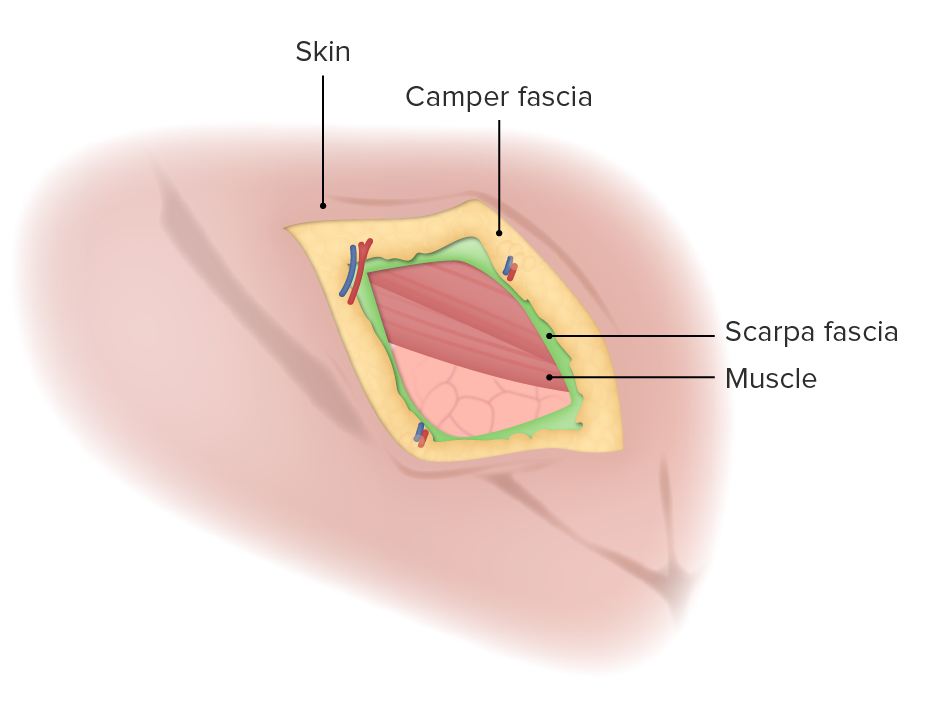
Layers of the anterolateral abdominal wall
Image by Lecturio.External oblique:
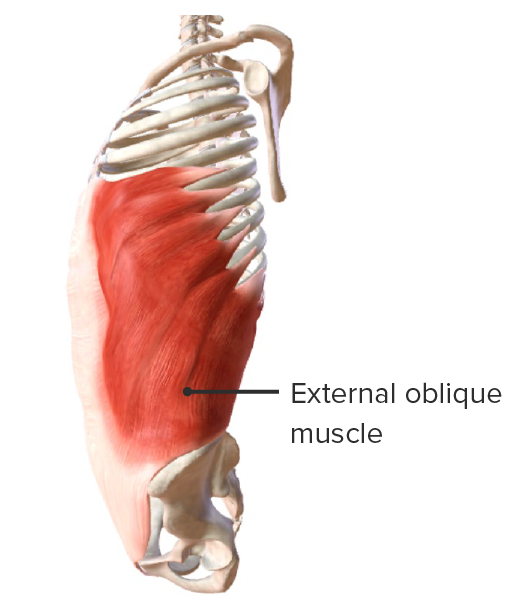
External oblique muscle
Image by BioDigital, edited by LecturioInternal oblique:
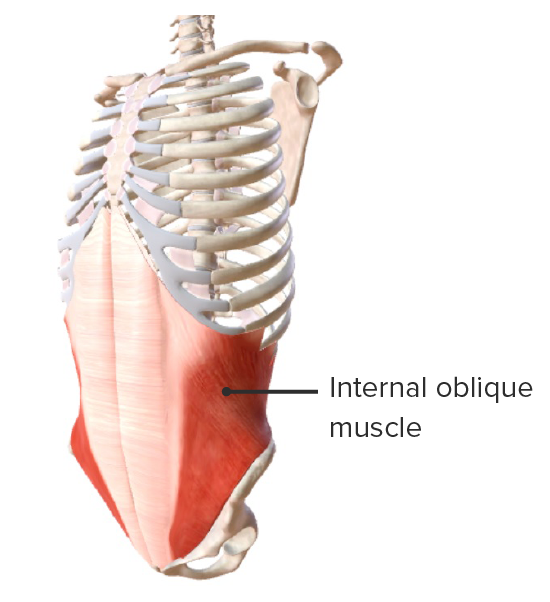
Internal oblique muscle
Image by BioDigital, edited by LecturioTransversus abdominis:
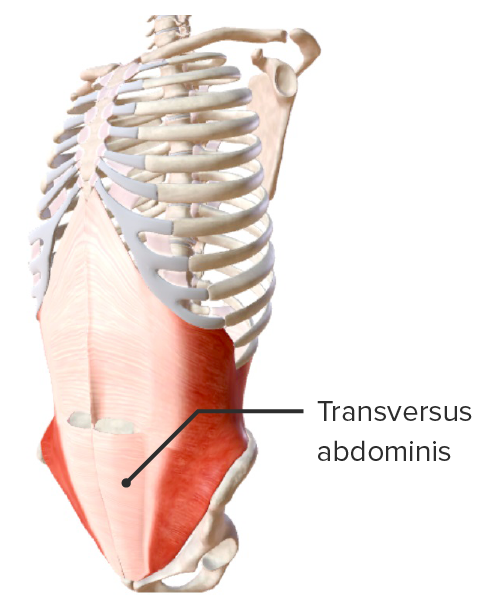
Transversus abdominis
Image by BioDigital, edited by LecturioRectus abdominis:
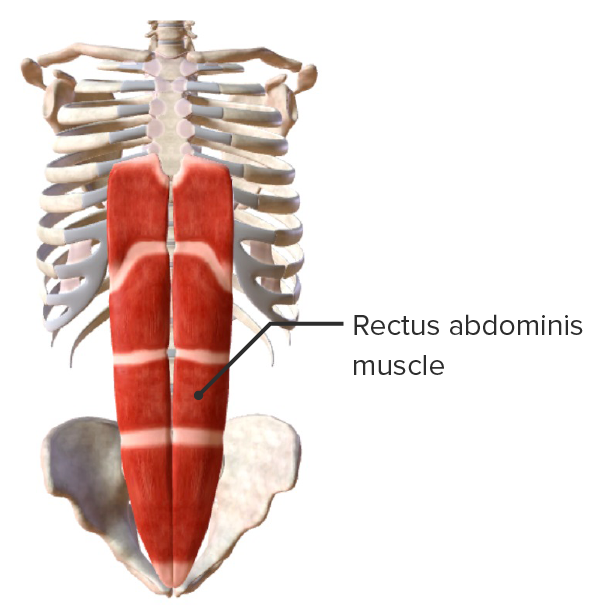
Rectus abdominis muscle
Image by BioDigital, edited by LecturioPyramidalis muscle:
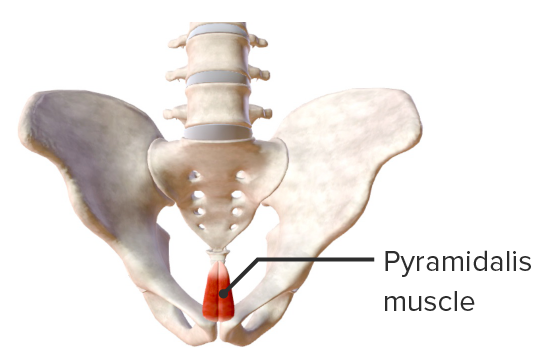
Pyramidalis muscle
Image by BioDigital, edited by Lecturio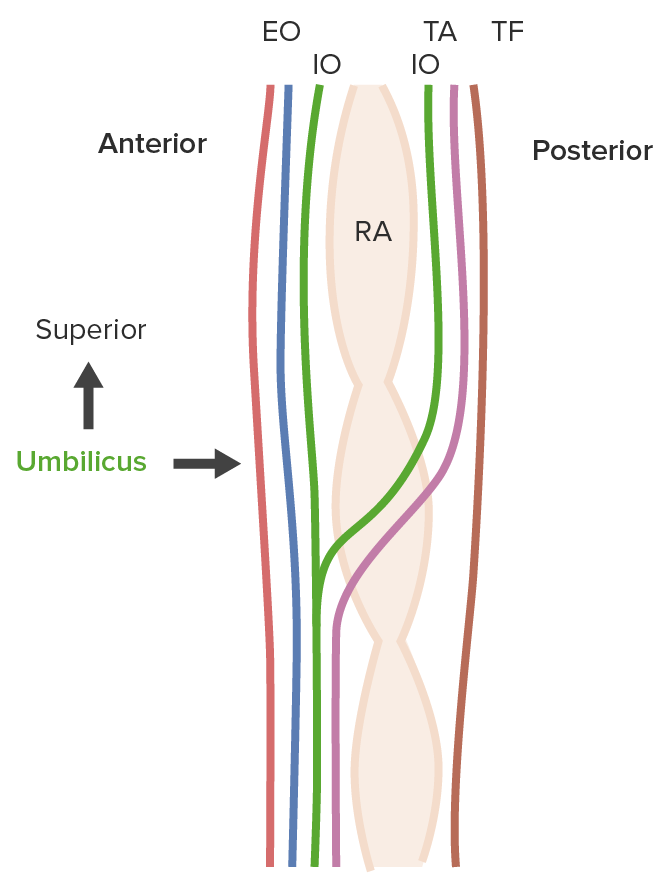
The outermost cutaneous layer is in orange. The aponeurosis of the exterior oblique (EO) is in blue, that of the internal oblique (IO) (anterior and posterior) is in green, that of the transverse abdominis (TA) is in purple, and that of the transversalis fascia (TF) is in black.
Note the change in the arrangement of the aponeurosis of the TA and the IO above and below the umbilicus. The posterior IO and TA aponeurosis move anterior to the rectus abdominis (RA) below the umbilicus while traveling posterior to the RA above the umbilicus. The point of transition is known as the arcuate line.
The inguinal canals are bilateral canals in the lower lateral anterior abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen that run obliquely and superolaterally to inferomedially. Each inguinal canal Inguinal canal The tunnel in the lower anterior abdominal wall through which the spermatic cord, in the male; round ligament, in the female; nerves; and vessels pass. Its internal end is at the deep inguinal ring and its external end is at the superficial inguinal ring. Inguinal Canal: Anatomy and Hernias has 4 walls and 2 openings (inguinal rings), 1 at each end.
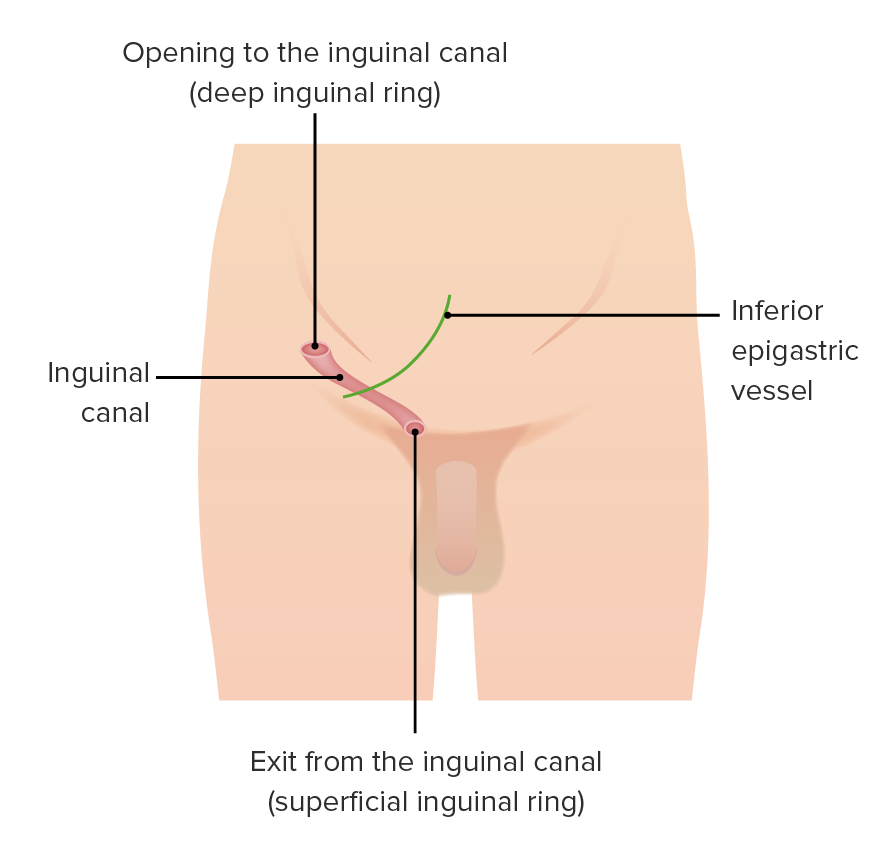
Schematic representation of the location of the inguinal canal in the anterior abdominal wall
Image by Lecturio.The arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology of the anterior abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen are divided into superficial and deep layers.
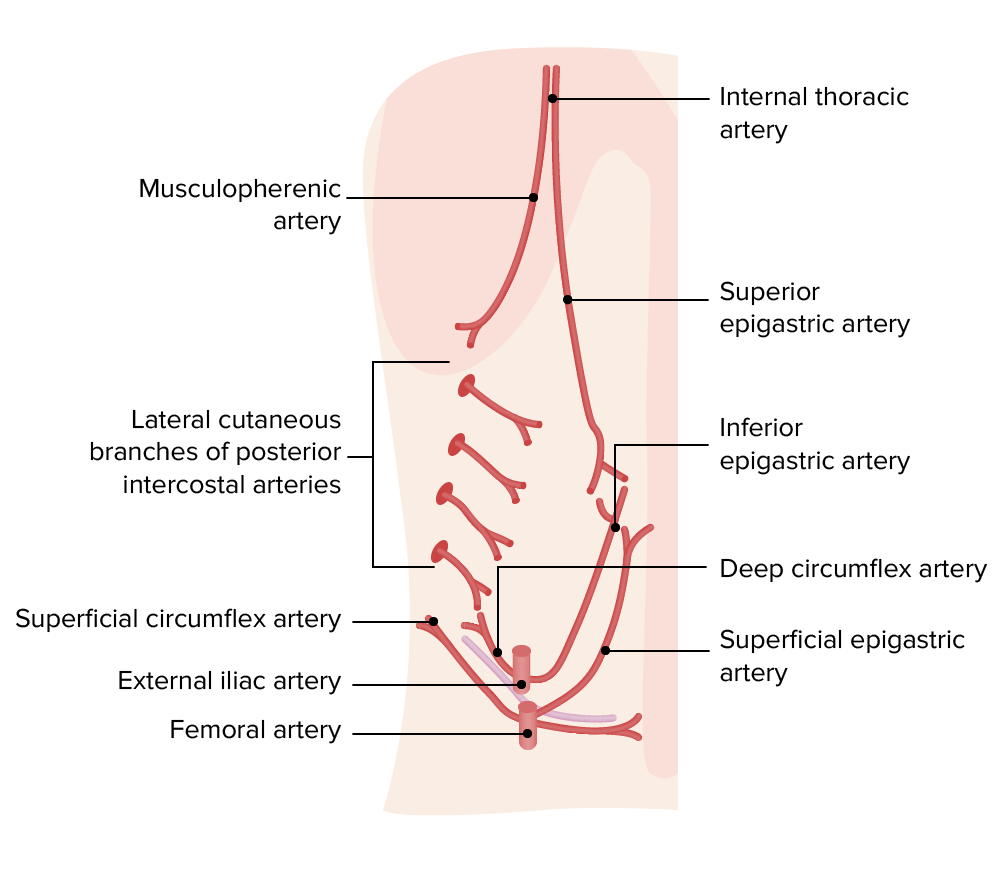
Arteries of the anterior and lateral abdominal wall
Image by Lecturio.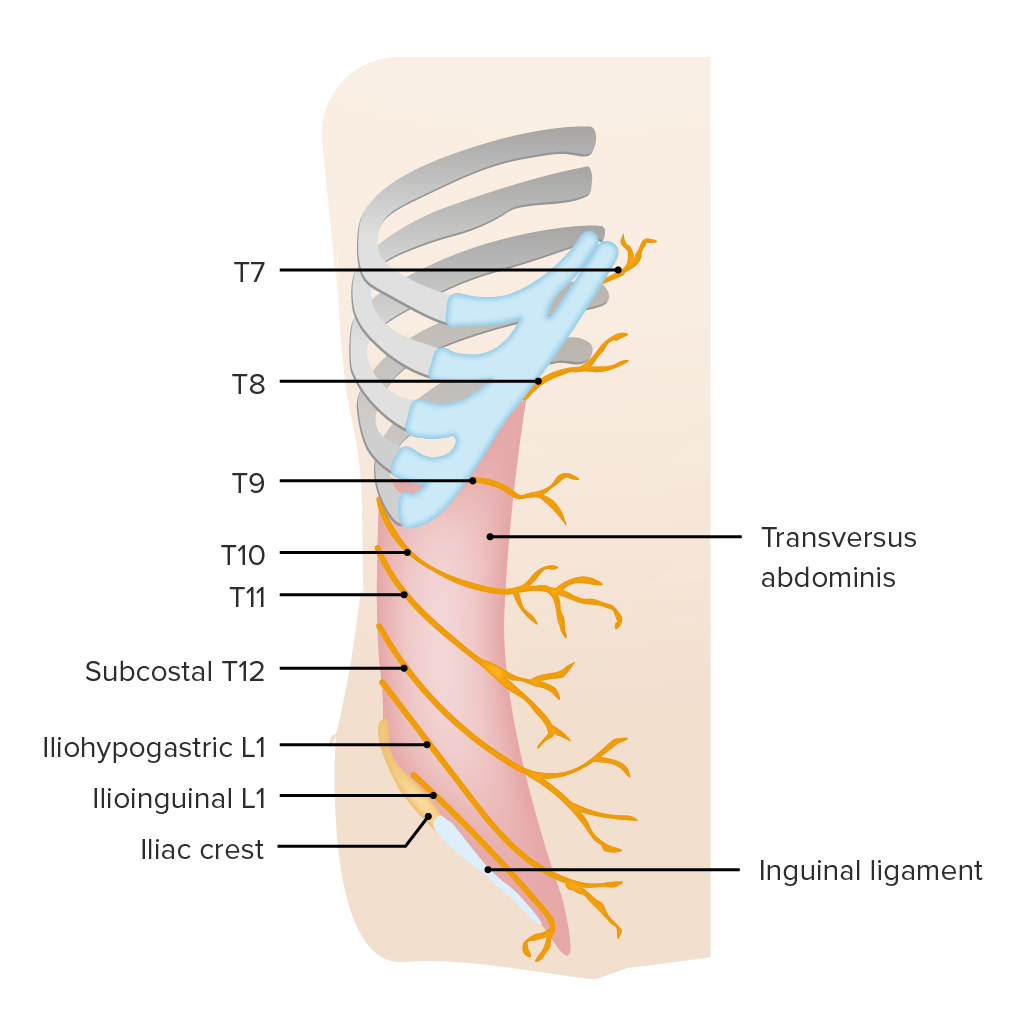
Innervation of the abdominal wall
Image by Lecturio.