An infection is the proliferation of microorganisms within tissues, body cavities, or spaces, which induces an immune response and overwhelms the body’s natural defenses. In surgical patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, these infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are frequently caused by the translocation of commensal organisms into deeper tissues, combined with the impairment of host defenses due to surgical injury or stress. Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease commonly identified in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship after surgery include surgical site infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, catheter-associated infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, and ventilator-associated infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Infection subtypes can be prevented, diagnosed, or treated using several strategies. The mainstays of treatment in surgical patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship involve local control of the infection as well as targeted antibiotic therapy.
Last updated: Apr 7, 2025
Surgical infection is a clinical disorder that manifests when the virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus of a microorganism introduced during surgical procedures overcome the innate and adaptive immune responses of the host.
Several factors make patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who have undergone surgery particularly susceptible to nosocomial infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease:
Presence of bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology may or may not be associated with clinically significant infection.
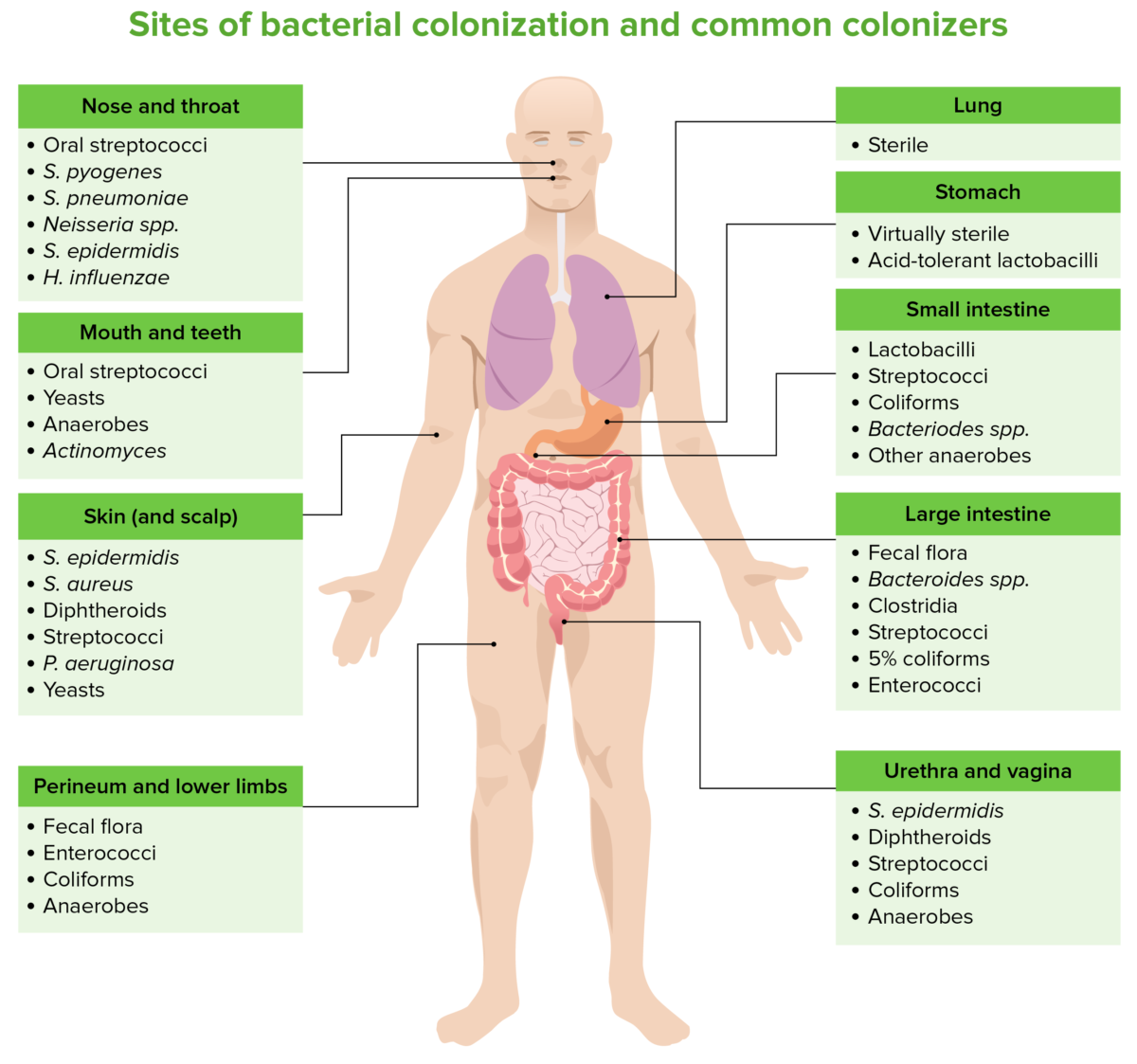
Sites of bacterial colonization and common colonizers
Image by Lecturio. License: CC BY-NC-SA 4.0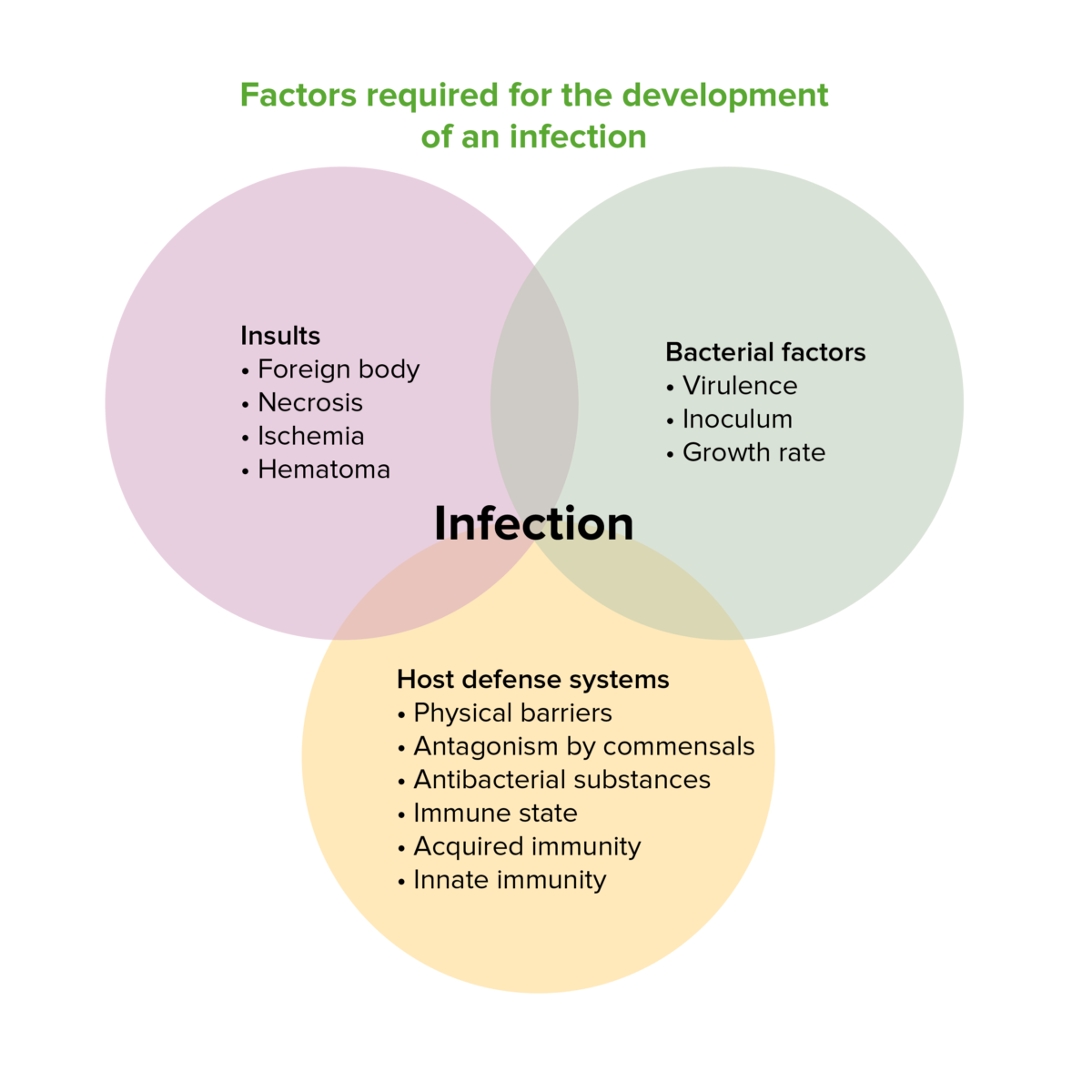
Factors required for the development of an infection
Image by Lecturio. License: CC BY-NC-SA 4.0Signs of systemic inflammation Systemic Inflammation Surgical Site Infections (SIRS):
Specific findings related to surgical infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease:
Signs of shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock:
Prevention of surgical infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease depends largely on sterile Sterile Basic Procedures technique, hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy hygiene, and the administration of prophylactic antibiotics.
A term used to describe steps taken by the surgical team before and during a surgical procedure to prevent the development of postoperative infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, which includes:
The management of surgical infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease is described using the term “source control,” which implies the combination of surgical management (if indicated) with the administration of antibiotics.
| Organism | 1st choice | Alternative |
|---|---|---|
| MSSA | Cefazolin Cefazolin A semisynthetic cephalosporin analog with broad-spectrum antibiotic action due to inhibition of bacterial cell wall synthesis. It attains high serum levels and is excreted quickly via the urine. Cephalosporins | Clarithromycin Clarithromycin A semisynthetic macrolide antibiotic derived from erythromycin that is active against a variety of microorganisms. It can inhibit protein synthesis in bacteria by reversibly binding to the 50s ribosomal subunits. This inhibits the translocation of aminoacyl transfer-RNA and prevents peptide chain elongation. Macrolides and Ketolides |
| MRSA MRSA A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins. Staphylococcus | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides |
|
| Coagulase-negative staphylococci Coagulase-negative staphylococci Staphylococcus | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides |
|
| Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus pneumoniae | Benzylpenicillin | Clarithromycin Clarithromycin A semisynthetic macrolide antibiotic derived from erythromycin that is active against a variety of microorganisms. It can inhibit protein synthesis in bacteria by reversibly binding to the 50s ribosomal subunits. This inhibits the translocation of aminoacyl transfer-RNA and prevents peptide chain elongation. Macrolides and Ketolides |
| S. pyogenes (group A β-hemolytic Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus) |
|
Clarithromycin Clarithromycin A semisynthetic macrolide antibiotic derived from erythromycin that is active against a variety of microorganisms. It can inhibit protein synthesis in bacteria by reversibly binding to the 50s ribosomal subunits. This inhibits the translocation of aminoacyl transfer-RNA and prevents peptide chain elongation. Macrolides and Ketolides |
| Enterococci | Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides |
| Bacteroides Bacteroides Bacteroides is a genus of opportunistic, anaerobic, gram-negative bacilli. Bacteroides fragilis is the most common species involved in human disease and is part of the normal flora of the large intestine. Bacteroides spp. | Metronidazole Metronidazole A nitroimidazole used to treat amebiasis; vaginitis; trichomonas infections; giardiasis; anaerobic bacteria; and treponemal infections. Pyogenic Liver Abscess |
|
| Escherichia coli Escherichia coli The gram-negative bacterium Escherichia coli is a key component of the human gut microbiota. Most strains of E. coli are avirulent, but occasionally they escape the GI tract, infecting the urinary tract and other sites. Less common strains of E. coli are able to cause disease within the GI tract, most commonly presenting as abdominal pain and diarrhea. Escherichia coli |
|
Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Haemophilus influenzae Haemophilus Influenzae A species of Haemophilus found on the mucous membranes of humans and a variety of animals. The species is further divided into biotypes I through viii. Haemophilus | Ceftriazone |
|
| Klebsiella Klebsiella Klebsiella are encapsulated gram-negative, lactose-fermenting bacilli. They form pink colonies on MacConkey agar due to lactose fermentation. The main virulence factor is a polysaccharide capsule. Klebsiella pneumoniae is the most important pathogenic species. Klebsiella spp. |
|
Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Proteus Proteus Proteus spp. are gram-negative, facultatively anaerobic bacilli. Different types of infection result from Proteus, but the urinary tract is the most common site. The majority of cases are caused by Proteus mirabilis (P. mirabilis). The bacteria are part of the normal intestinal flora and are also found in the environment. Proteus spp. |
|
Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Pseudomonas aeruginosa Pseudomonas aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas | Piperacillin-tazobactam Piperacillin-Tazobactam Multidrug-resistant Organisms and Nosocomial Infections | Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Clostridium spp. | Benzylpenicillin | Metronidazole Metronidazole A nitroimidazole used to treat amebiasis; vaginitis; trichomonas infections; giardiasis; anaerobic bacteria; and treponemal infections. Pyogenic Liver Abscess |
| C. difficile | Fidaxomicin |
|
Abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease:
Necrotizing fasciitis Necrotizing fasciitis Necrotizing fasciitis is a life-threatening infection that causes rapid destruction and necrosis of the fascia and subcutaneous tissues. Patients may present with significant pain out of proportion to the presenting symptoms and rapidly progressive erythema of the affected area. Necrotizing Fasciitis and diabetic foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease: