Multidrug-resistant organisms (MDROs) and nosocomial infections are a global health issue and a major cause of morbidity and mortality. MDROs are microorganisms, mainly bacteria, that are resistant/non-susceptible to ≥1 agent in ≥3 antimicrobial class categories. Included in this group are methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VREs), Gram-negative bacteria that produce extended spectrum beta-lactamases (ESBLs), difficult-to-treat/resistant Pseudomonas aeruginosa, and carbapenem-resistant Enterobacterales or CREs (e.g., Escherichia coli, Salmonella, and Klebsiella). Since antibiotic therapy for MDROs is limited, preventive measures such as antibiotic stewardship and infection control are recommended. Nosocomial infections, also called “healthcare-associated” or “hospital-acquired” infections (HAI), are infections transmitted in a hospital or healthcare facility, and which were absent at the time of admission. These include intravascular catheter-related infections, catheter-associated urinary tract infections (CAUTIs), hospital-acquired pneumonia (HAP), ventilator-associated pneumonia (VAP), Clostridioides difficile infections (CDIs), and surgical site infections. Risk factors for developing such infections include hospitalization, residence in a long-term healthcare facility, frequent use of antibiotics, and underlying comorbidities.
Last updated: Jul 10, 2023
Contents
Excluding nosocomial transmission of SARS-CoV-2 during the pandemic, non–bacterial HAIs HAIs Carbapenems and Aztreonam are less common than bacterial HAIs HAIs Carbapenems and Aztreonam.
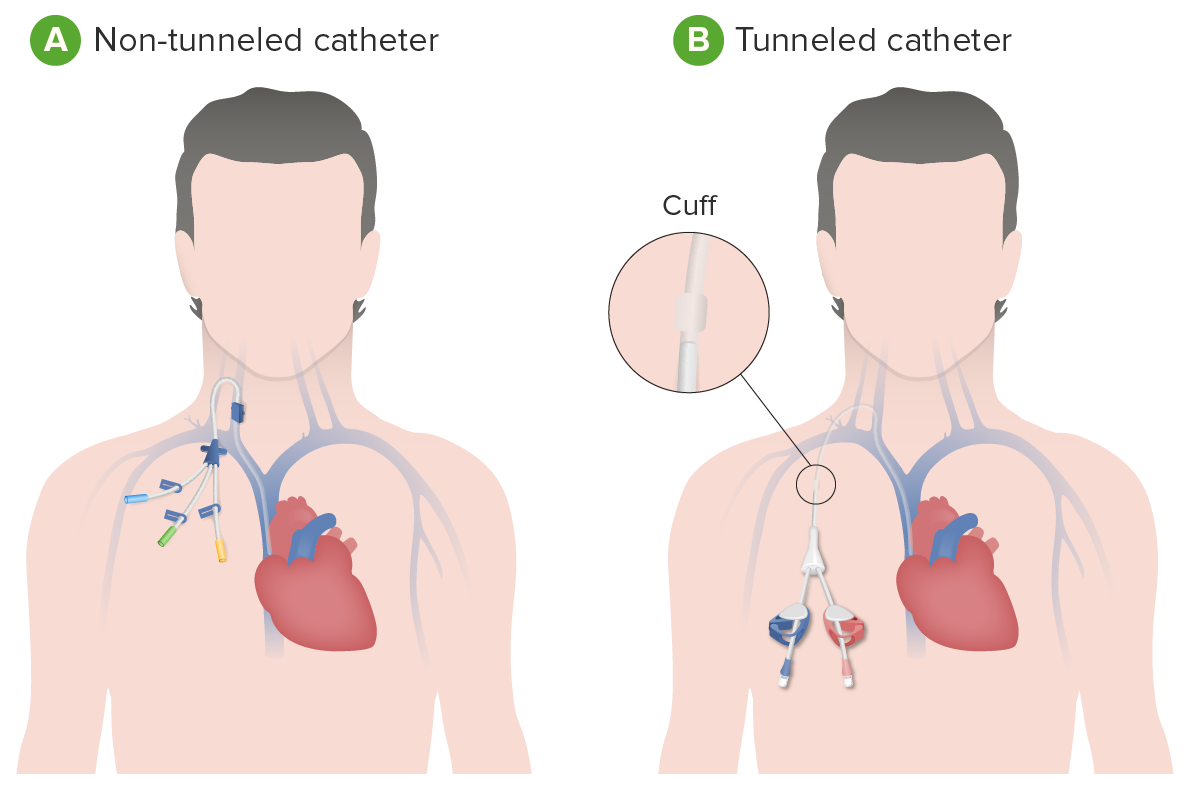
A central venous catheter (e.g., a dialysis catheter) is a potential source of infection:
A: Non-tunneled catheter (designed to be temporary and may be put into a large vein near the neck, chest, or groin)
B: Tunneled (placed underneath the skin) dialysis catheter (intended to be used for a longer duration of time)
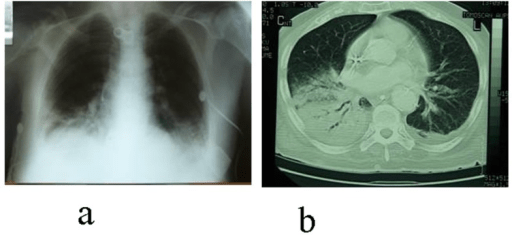
Ventilator-associated pneumonia:
a: Chest X-ray (CXR) showing pneumonia in the base of the right lung
b: CT scan of the chest reveals a developing lung abscess with pleuritis and apparent empyema in the area noted on the CXR
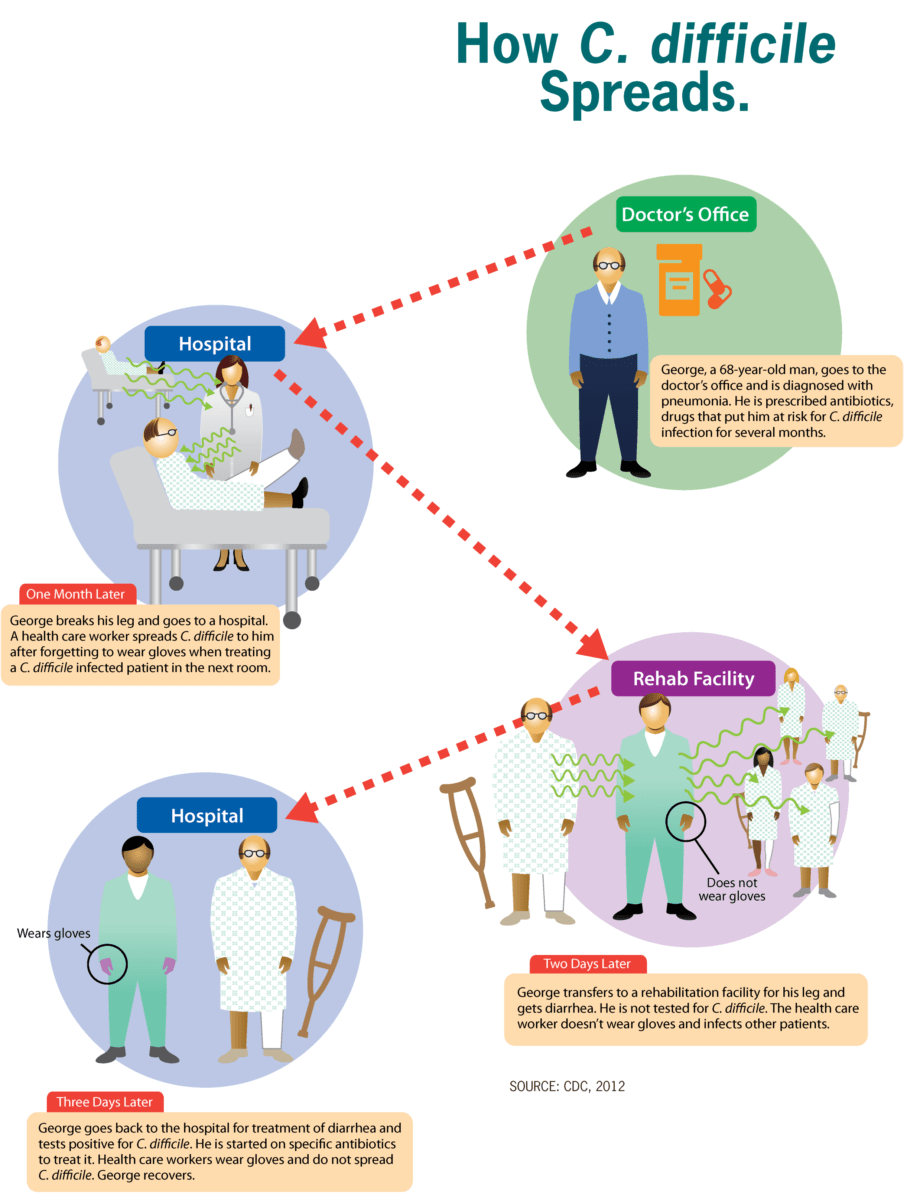
The image shows how Clostridioides difficile (C. difficile) spreads throughout the environment, favoring healthcare settings such as hospital and rehabilitation facilities
Image: “How C. difficile spreads” by CDC. License: Public Domain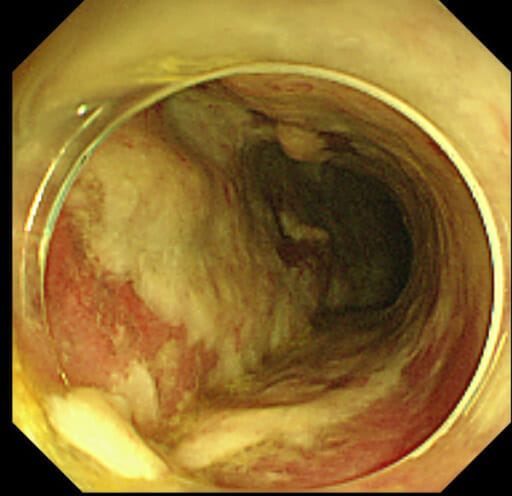
Pseudomembranous colitis due to C. difficile infection: colonoscopy demonstrating a colonic wall covered by thick pseudomembranes, which consist of irregular plaque-like patches of fibrinopurulent material and sloughed-off mucosal epithelium which overlie red, inflamed bowel mucosa.
Image: “Colonoscopy on the fifth postoperative day” by Department of Surgery, Jichi Medical University Saitama Medical Center. License: CC BY 2.0