Stevens-Johnson syndrome (SJS) is a cutaneous, immune-mediated hypersensitivity reaction that is commonly triggered by medications, including antiepileptics and antibiotics. The condition runs on a spectrum with toxic epidermal necrolysis (TEN) based on the amount of body surface area (BSA) involved. Stevens-Johnson syndrome is characterized by keratinocyte Keratinocyte Epidermal cells which synthesize keratin and undergo characteristic changes as they move upward from the basal layers of the epidermis to the cornified (horny) layer of the skin. Successive stages of differentiation of the keratinocytes forming the epidermal layers are basal cell, spinous or prickle cell, and the granular cell. Erythema Multiforme necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage and separation of the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions from the dermis Dermis A layer of vascularized connective tissue underneath the epidermis. The surface of the dermis contains innervated papillae. Embedded in or beneath the dermis are sweat glands; hair follicles; and sebaceous glands. Skin: Structure and Functions. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will present with a flu-like prodrome Prodrome Symptoms that appear 24–48 hours prior to migraine onset. Migraine Headache, followed by cutaneous bullae Bullae Erythema Multiforme and sloughing on the face, thorax, and mucous membranes. Stevens-Johnson syndrome is considered a medical emergency, and management is largely supportive. Withdrawal of the causative agent is required. Monitoring for, and treating, superinfection is essential due to the high risk of associated death in these patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.
Last updated: Jul 14, 2025
| Subtype | Involved BSA |
|---|---|
|
Stevens-Johnson syndrome |
<10% of BSA |
|
Overlapping SJS/TEN |
10%‒30% of BSA |
|
Toxic epidermal necrolysis |
>30% of BSA |
The following table lists the major common medications and infectious causes of SJS/TEN:
| Types | Examples | |
|---|---|---|
|
Medications |
Antiepileptics |
Lamotrigine Lamotrigine A phenyltriazine compound, sodium and calcium channel blocker that is used for the treatment of seizures and bipolar disorder. Second-Generation Anticonvulsant Drugs, phenobarbital Phenobarbital A barbituric acid derivative that acts as a nonselective central nervous system depressant. It potentiates gamma-aminobutyric acid action on gaba-a receptors, and modulates chloride currents through receptor channels. It also inhibits glutamate induced depolarizations. First-Generation Anticonvulsant Drugs, carbamazepine Carbamazepine A dibenzazepine that acts as a sodium channel blocker. It is used as an anticonvulsant for the treatment of grand mal and psychomotor or focal seizures. It may also be used in the management of bipolar disorder, and has analgesic properties. First-Generation Anticonvulsant Drugs, phenytoin Phenytoin An anticonvulsant that is used to treat a wide variety of seizures. The mechanism of therapeutic action is not clear, although several cellular actions have been described including effects on ion channels, active transport, and general membrane stabilization. Phenytoin has been proposed for several other therapeutic uses, but its use has been limited by its many adverse effects and interactions with other drugs. First-Generation Anticonvulsant Drugs |
|
Sulfa |
Cotrimoxazole, sulfasalazine Sulfasalazine A drug that is used in the management of inflammatory bowel diseases. Its activity is generally considered to lie in its metabolic breakdown product, 5-aminosalicylic acid released in the colon. Sulfonamides and Trimethoprim |
|
|
Other antibiotics |
Aminopenicillins Aminopenicillins Penicillins, fluoroquinolones Fluoroquinolones Fluoroquinolones are a group of broad-spectrum, bactericidal antibiotics inhibiting bacterial DNA replication. Fluoroquinolones cover gram-negative, anaerobic, and atypical organisms, as well as some gram-positive and multidrug-resistant (MDR) organisms. Fluoroquinolones, cephalosporins Cephalosporins Cephalosporins are a group of bactericidal beta-lactam antibiotics (similar to penicillins) that exert their effects by preventing bacteria from producing their cell walls, ultimately leading to cell death. Cephalosporins are categorized by generation and all drug names begin with “cef-” or “ceph-.” Cephalosporins |
|
|
Meloxicam Meloxicam A benzothiazine and thiazole derivative that acts as a nsaid and cyclooxygenase-2 (cox-2) inhibitor. It is used in the treatment of rheumatoid arthritis; osteoarthritis; and ankylosing spondylitis. Nonsteroidal Antiinflammatory Drugs (NSAIDs), piroxicam Piroxicam A cyclooxygenase inhibiting, non-steroidal anti-inflammatory agent (nsaid) that is well established in treating rheumatoid arthritis and osteoarthritis and used for musculoskeletal disorders, dysmenorrhea, and postoperative pain. Its long half-life enables it to be administered once daily. Nonsteroidal Antiinflammatory Drugs (NSAIDs) |
||
|
Antiretrovirals |
Nevirapine Nevirapine A potent, non-nucleoside reverse transcriptase inhibitor used in combination with nucleoside analogues for treatment of HIV infections and aids. Anti-HIV Drugs |
|
|
Miscellaneous |
Allopurinol Allopurinol A xanthine oxidase inhibitor that decreases uric acid production. It also acts as an antimetabolite on some simpler organisms. Gout Drugs, chlormezanone |
|
|
Infectious |
Viral |
Herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology, HIV HIV Anti-HIV Drugs, coxsackievirus Coxsackievirus Coxsackievirus is a member of a family of viruses called Picornaviridae and the genus Enterovirus. Coxsackieviruses are single-stranded, positive-sense RNA viruses, and are divided into coxsackie group A and B viruses. Both groups of viruses cause upper respiratory infections, rashes, aseptic meningitis, or encephalitis. Coxsackievirus, hepatitis, influenza Influenza Influenza viruses are members of the Orthomyxoviridae family and the causative organisms of influenza, a highly contagious febrile respiratory disease. There are 3 primary influenza viruses (A, B, and C) and various subtypes, which are classified based on their virulent surface antigens, hemagglutinin (HA) and neuraminidase (NA). Influenza typically presents with a fever, myalgia, headache, and symptoms of an upper respiratory infection. Influenza Viruses/Influenza, mumps Mumps Mumps is caused by a single-stranded, linear, negative-sense RNA virus of the family Paramyxoviridae. Mumps is typically a disease of childhood, which manifests initially with fever, muscle pain, headache, poor appetite, and a general feeling of malaise, and is classically followed by parotitis. Mumps Virus/Mumps, Epstein-Barr virus Epstein-Barr Virus Epstein-Barr virus (EBV) is a linear, double-stranded DNA virus belonging to the Herpesviridae family. This highly prevalent virus is mostly transmitted through contact with oropharyngeal secretions from an infected individual. The virus can infect epithelial cells and B lymphocytes, where it can undergo lytic replication or latency. Epstein-Barr Virus, enteroviruses |
|
Bacterial |
Group A beta-hemolytic streptococci, brucellosis Brucellosis Brucellosis (also known as undulant fever, Mediterranean fever, or Malta fever) is a zoonotic infection that spreads predominantly through ingestion of unpasteurized dairy products or direct contact with infected animal products. Clinical manifestations include fever, arthralgias, malaise, lymphadenopathy, and hepatosplenomegaly. Brucella/Brucellosis, mycobacteria Mycobacteria Mycobacterium is a genus of the family Mycobacteriaceae in the phylum Actinobacteria. Mycobacteria comprise more than 150 species of facultative intracellular bacilli that are mostly obligate aerobes. Mycobacteria are responsible for multiple human infections including serious diseases, such as tuberculosis (M. tuberculosis), leprosy (M. leprae), and M. avium complex infections. Mycobacterium, Mycoplasma pneumoniae Mycoplasma pneumoniae Short filamentous organism of the genus mycoplasma, which binds firmly to the cells of the respiratory epithelium. It is one of the etiologic agents of non-viral primary atypical pneumonia in man. Mycoplasma, rickettsia Rickettsia Rickettsiae are a diverse collection of obligate intracellular, gram-negative bacteria that have a tropism for vascular endothelial cells. The vectors for transmission vary by species but include ticks, fleas, mites, and lice. Rickettsia, tularemia | |
The exact mechanism is unknown, but there are several theories:
This impaired skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions integrity can lead to:
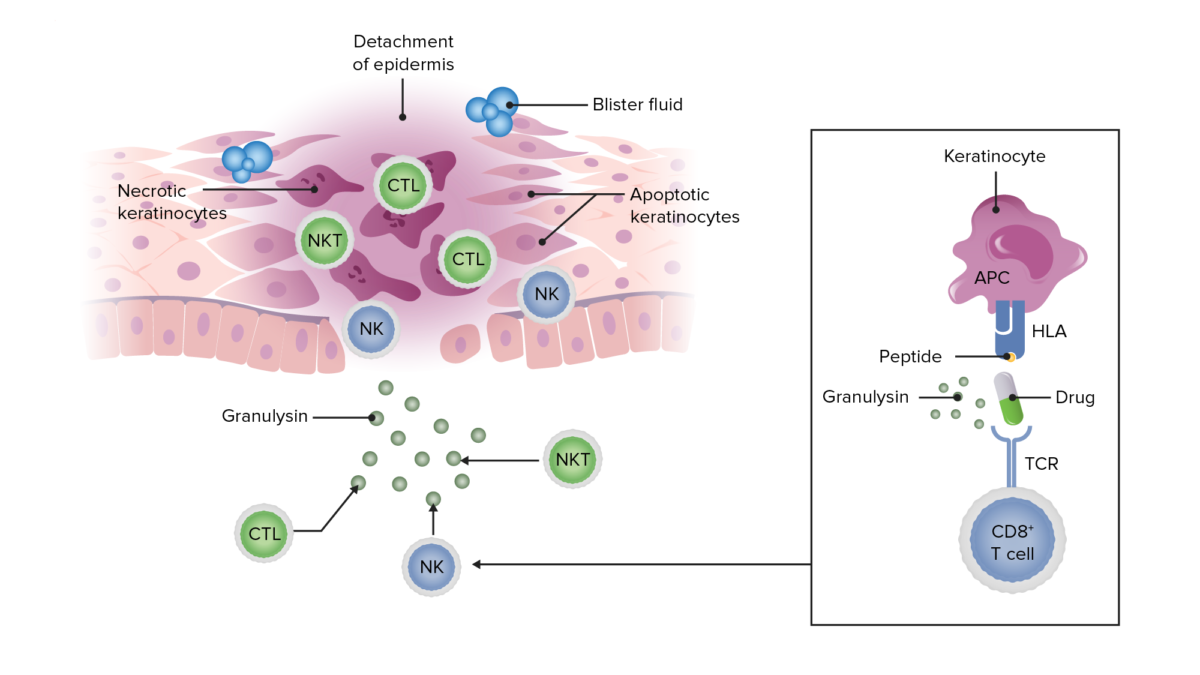
Schematic showing how a peptide antigen (in this case, from a drug) presented on keratinocytes can lead to a cytotoxic inflammatory response resulting in granulysin release, keratinocyte apoptosis and necrosis, detachment of the epidermis, and blister formation in SJS and TEN.
Image by Lecturio.Prodrome Prodrome Symptoms that appear 24–48 hours prior to migraine onset. Migraine Headache:
Acute phase Acute phase Short Bowel Syndrome:

Oral lesions from SJS seen in a patient on an antiretroviral medication (nevirapine).
Image: “Oral lesions associated with nevirapine-related Stevens Johnson syndrome: A report of four cases.” by lasundaram S, Ranganathan K, Umadevi K, Gunaseelan R, Kumaraswamy N, Solomon S, Devaleenol B, Ambrose P – Journal of oral and maxillofacial pathology : JOMFP (2011). License: CC BY 2.0
Characteristic lesions of SJS/TEN in a patient with accompanying erythema and sloughing.
Image: “Oral lesions associated with nevirapine-related Stevens Johnson syndrome: A report of four cases” by Balasundaram S, Ranganathan K, Umadevi K, Gunaseelan R, Kumaraswamy N, Solomon S, Devaleenol B, Ambrose P – Journal of oral and maxillofacial pathology : JOMFP (2011) . License: CC BY 2.0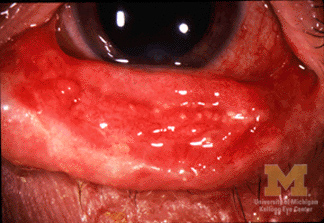
Keratoconjunctivitis in a patient with SJS/TEN.
Image: “Conjunctivitis in SJS” by Jonathan Trobe, M.D., University of Michigan Kellogg Eye Center. License: CC BY 3.0
Demonstration of Nikolsky’s sign by causing skin sloughing with the application of pressure.
Image: “Curcumin in stevens-johnsons syndrome: culprit or bystander?” by Irani C, Haddad F, Maalouly G, Nemnoum R. License: CC BY 2.0
Drug-induced toxic epidermal necrolysis with peeled skin over the back and buttocks.
Image: “Drug induced toxic epidermal necrolysis: two case reports” by Qadir SN, Raza N, Qadir F. License: CC BY 3.0
Photograph of a patient with widespread denudation of the epidermis in sheets, consistent with toxic epidermal necrolysis.
Image: “Review of Toxic Epidermal Necrolysis” by International Journal of Molecular Sciences. License: CC BY 4.0The diagnosis is clinical, based on history and physical exam findings.
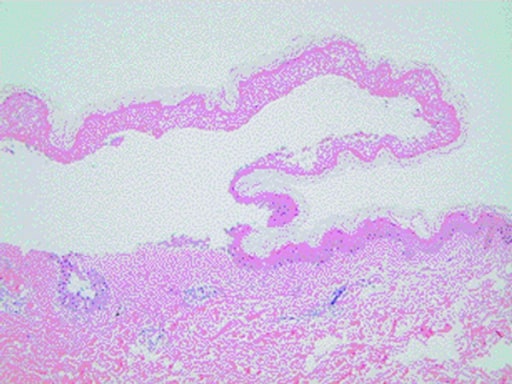
Histopathology of a skin biopsy taken from a patient with SJS/TEN showing characteristic epidermal detachment and lymphocyte infiltration in the dermis
Image: “Curcumin in stevens-johnsons syndrome: culprit or bystander?” by Irani C, Haddad F, Maalouly G, Nemnoum R. License: CC BY 2.0| Prognostic factors | Score |
|---|---|
|
Age ≥ 40 years |
1 |
|
Malignancy Malignancy Hemothorax present |
1 |
|
Body surface area detached ≥ 10% |
1 |
|
Tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children ≥ 120/min |
1 |
|
Serum urea Urea A compound formed in the liver from ammonia produced by the deamination of amino acids. It is the principal end product of protein catabolism and constitutes about one half of the total urinary solids. Urea Cycle > 10 mmol/L |
1 |
|
Serum glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance > 14 mmol/L |
1 |
|
Serum bicarbonate Bicarbonate Inorganic salts that contain the -HCO3 radical. They are an important factor in determining the ph of the blood and the concentration of bicarbonate ions is regulated by the kidney. Levels in the blood are an index of the alkali reserve or buffering capacity. Electrolytes < 20 mmol/L |
1 |
The SCORTEN score is used to help determine the severity, prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas, and appropriate setting for management in SJS/TEN patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.