Invasive mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing (IMV) is an advanced airway Airway ABCDE Assessment modality used for individuals with immediate or impending respiratory failure Respiratory failure Respiratory failure is a syndrome that develops when the respiratory system is unable to maintain oxygenation and/or ventilation. Respiratory failure may be acute or chronic and is classified as hypoxemic, hypercapnic, or a combination of the two. Respiratory Failure and/or in preparation for surgery. The IMV technique involves positive pressure ventilation Positive pressure ventilation Application of positive pressure to the inspiratory phase when the patient has an artificial airway in place and is connected to a ventilator. Flail Chest delivered to the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy through an endotracheal tube via a ventilator. The ventilator can be set to specific modes that determine how the machine assists with breathing. The modes are tailored to the individual's needs. The mode refers to the characteristics of mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing and mainly includes trigger (how inspiration Inspiration Ventilation: Mechanics of Breathing begins), cycle (how inspiration Inspiration Ventilation: Mechanics of Breathing ends), and limit (when inspiration Inspiration Ventilation: Mechanics of Breathing should be aborted). The most commonly used mode is assist-control ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing, which is usually followed by pressure-support ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing for weaning. Careful consideration should be exercised while planning extubation, as IMV is associated with complications.
Last updated: May 17, 2024
Invasive mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing (IMV) is a form of advanced airway Airway ABCDE Assessment management used to deliver oxygen and/or to regulate ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing at the level of the trachea Trachea The trachea is a tubular structure that forms part of the lower respiratory tract. The trachea is continuous superiorly with the larynx and inferiorly becomes the bronchial tree within the lungs. The trachea consists of a support frame of semicircular, or C-shaped, rings made out of hyaline cartilage and reinforced by collagenous connective tissue. Trachea: Anatomy through 3 main routes:
There are several modes of IMV that are managed jointly based on:
Invasive mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing is not a benign Benign Fibroadenoma intervention:
Ventilator mode is described based on 3 characteristics, namely, trigger, cycle, and limit:
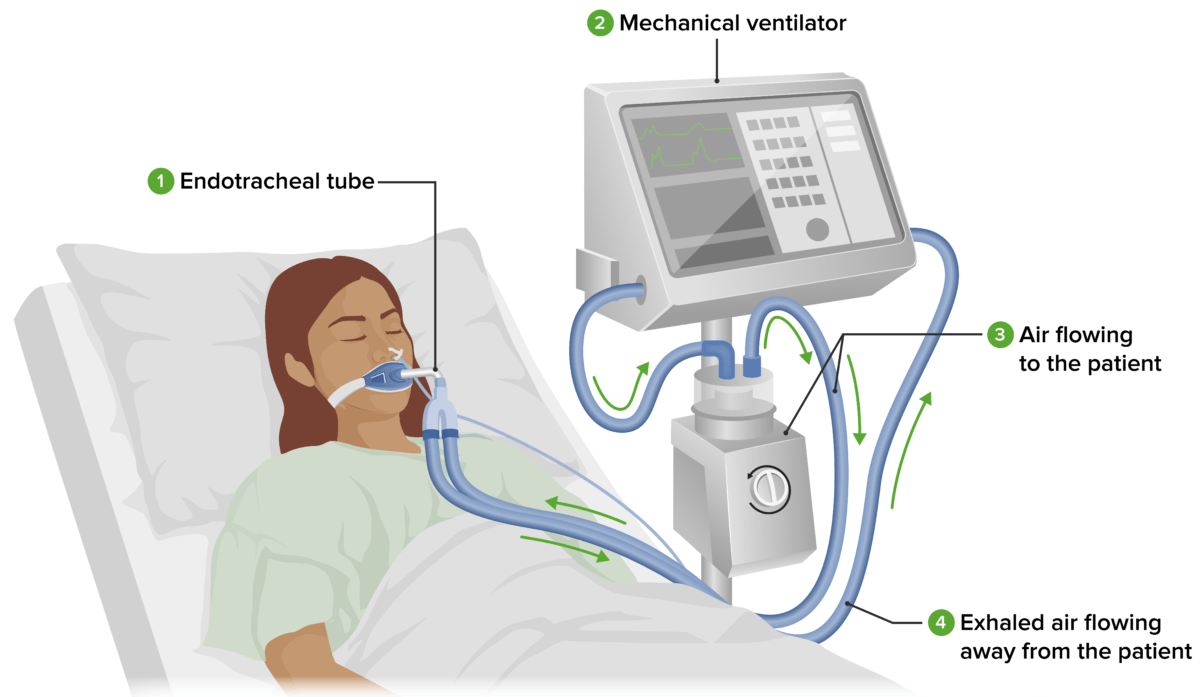
Standard ventilator setup:
An endotracheal tube (or tracheostomy) (1) placed in the individual’s trachea is attached to the tubing of the mechanical ventilator (2). The mechanical ventilator delivers oxygenated air through tubes into the individual’s respiratory tract. Air flowing to the individual (3) passes through a humidifier, where it is warmed and moistened. Exhaled air flowing away from the individual (4) is returned to the ventilator. The nurse periodically checks the individual and ventilator.
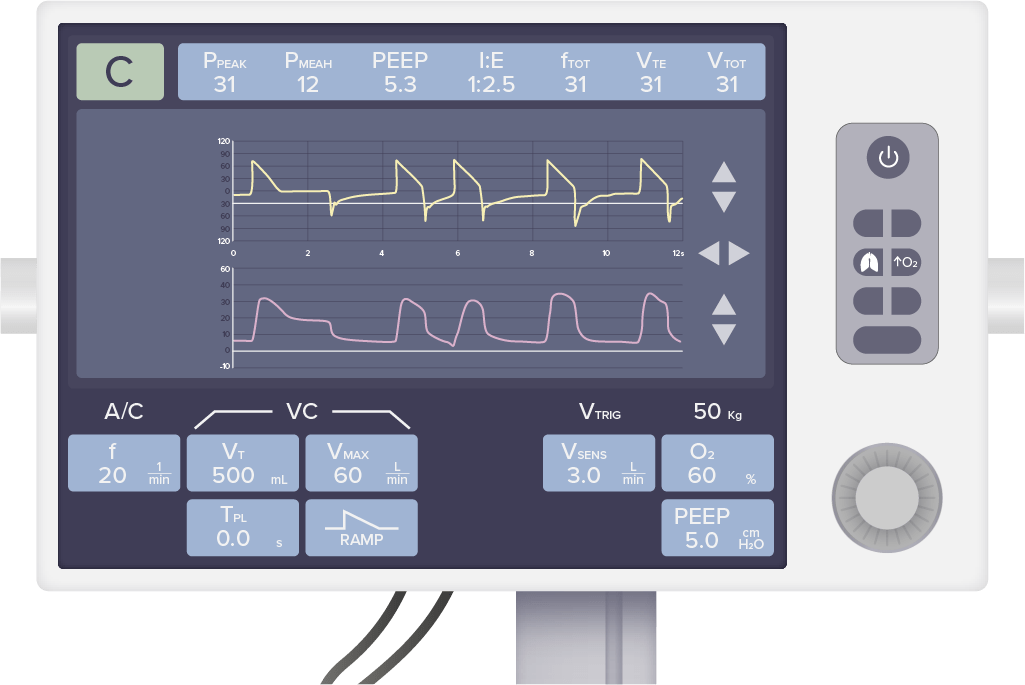
Standard ventilator user interface:
The top row of values displays respiratory parameters generated by the individual. The bottom row of values displays ventilator settings that can be manipulated by the operator depending on the clinical scenario and the needs of the individual.
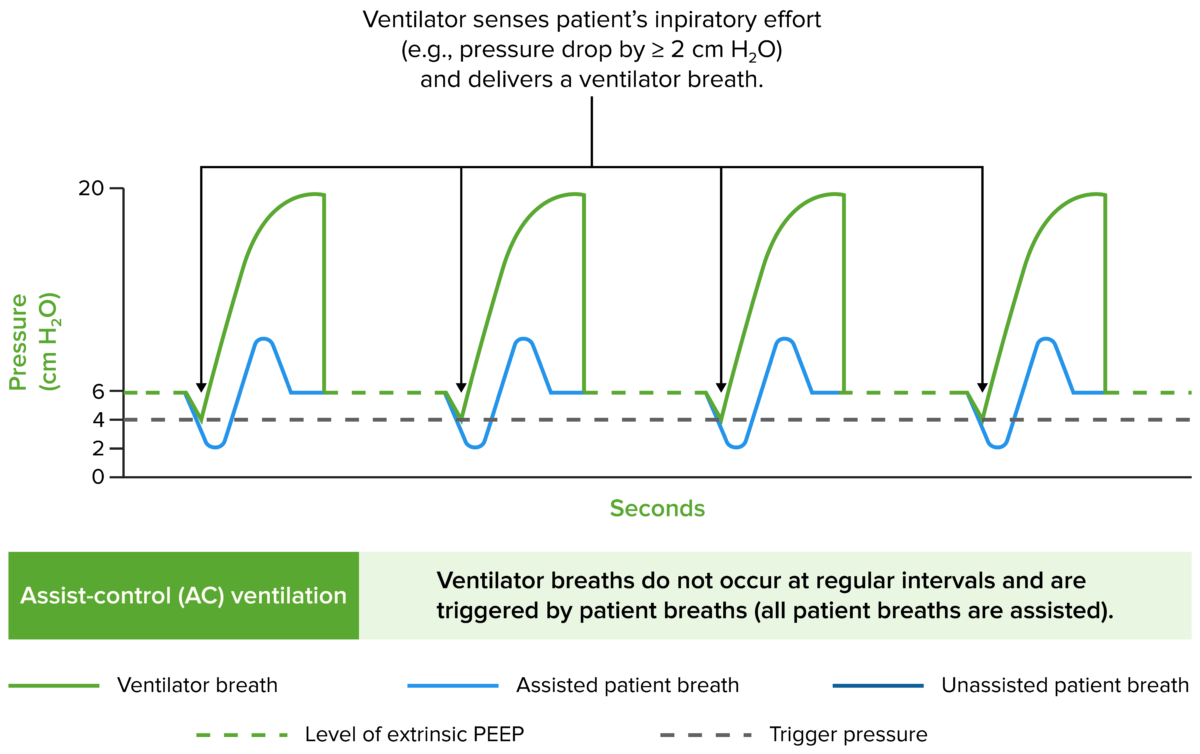
Airway pressure tracings in the main modes of ventilation
Image by Lecturio.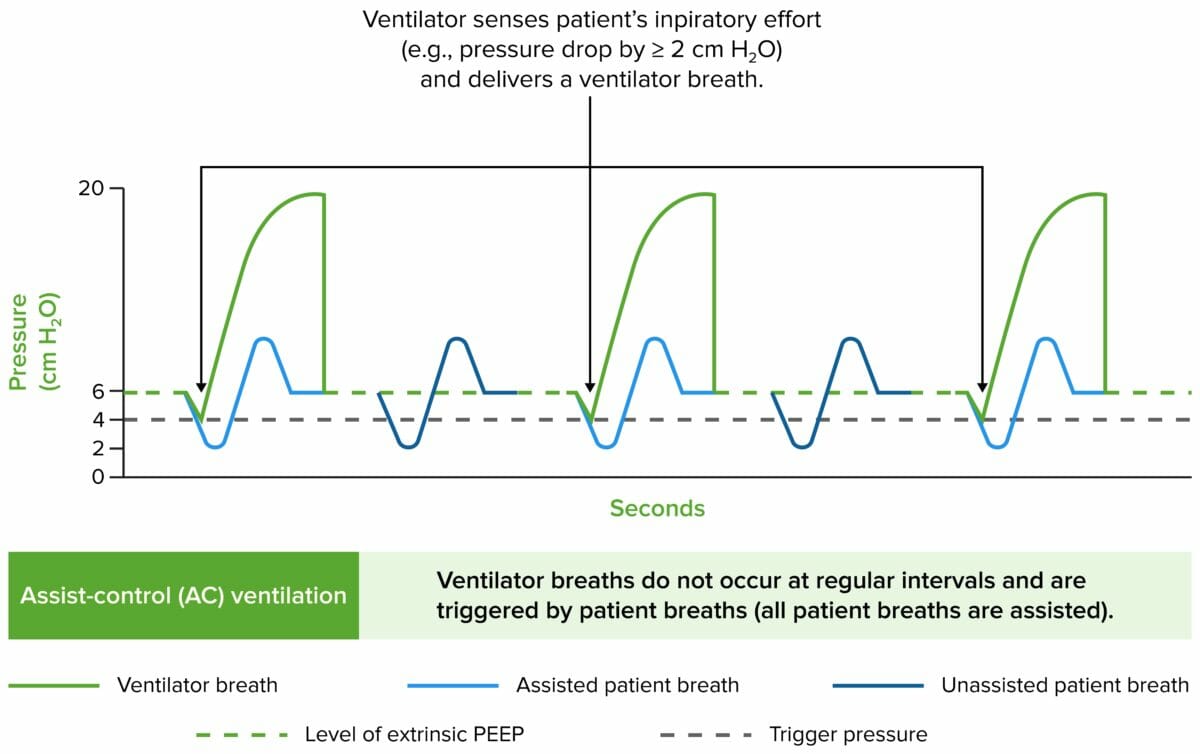
Airway pressure tracings in the main modes of ventilation
Image by Lecturio.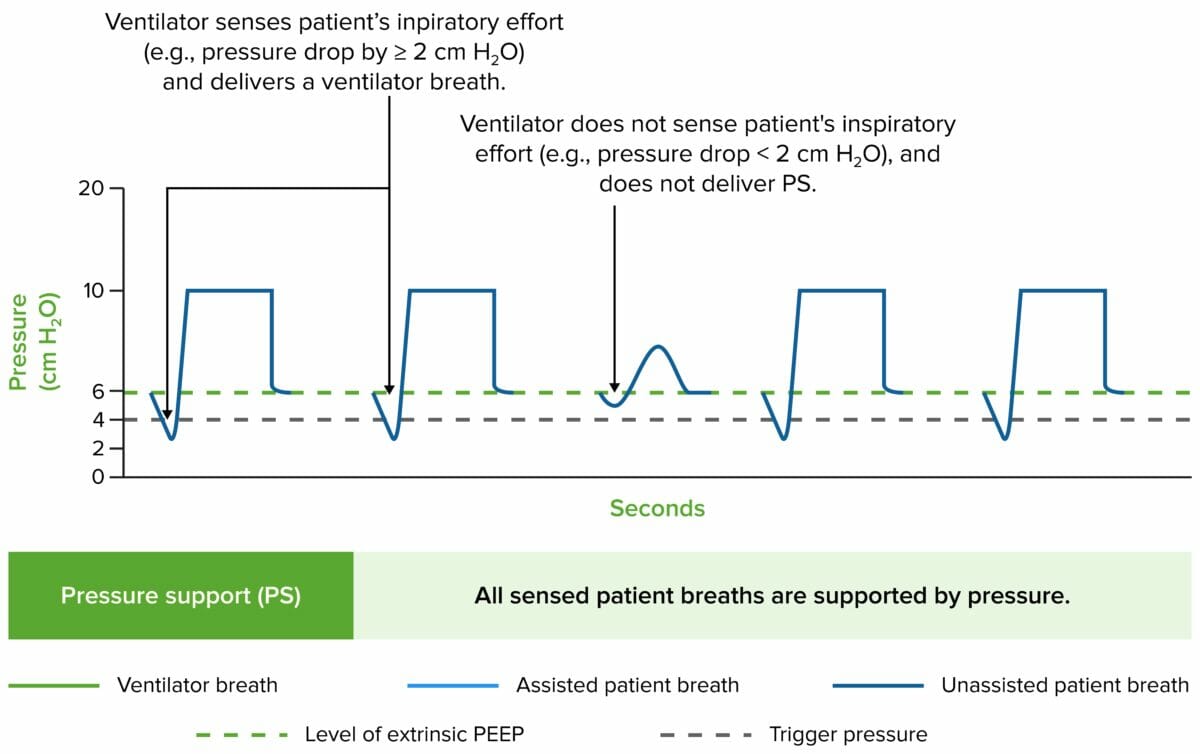
Airway pressure tracings in the main modes of ventilation
Image by Lecturio.Commonly used to prevent ventilator-associated complications.
An SBT consists of minimal ventilator settings that can be used to predict the chances of successful extubation.
When extubating, consider trialing higher levels of supplemental O₂:
Mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing is a medical intervention used to support a patient’s natural breathing when they are unable to do so adequately on their own, using a ventilator device.
The medical abbreviation CPAP CPAP A technique of respiratory therapy, in either spontaneously breathing or mechanically ventilated patients, in which airway pressure is maintained above atmospheric pressure throughout the respiratory cycle by pressurization of the ventilatory circuit. Noninvasive Ventilation stands for continuous positive airway Airway ABCDE Assessment pressure. In CPAP CPAP A technique of respiratory therapy, in either spontaneously breathing or mechanically ventilated patients, in which airway pressure is maintained above atmospheric pressure throughout the respiratory cycle by pressurization of the ventilatory circuit. Noninvasive Ventilation mode, a ventilator delivers a continuous and constant pressure of air (or oxygen-enriched air) to the patient’s airway Airway ABCDE Assessment. This pressure prevents the airway Airway ABCDE Assessment from collapsing during exhalation and promotes better oxygen exchange in the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy. CPAP CPAP A technique of respiratory therapy, in either spontaneously breathing or mechanically ventilated patients, in which airway pressure is maintained above atmospheric pressure throughout the respiratory cycle by pressurization of the ventilatory circuit. Noninvasive Ventilation is commonly used in non-invasive ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing to support patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with conditions like obstructive sleep apnea Sleep apnea Repeated cessation of breathing for > 10 seconds during sleep and results in sleep interruption, fatigue, and daytime sleepiness. Obstructive Sleep Apnea.
ACVC stands for assist-control volume control ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing. In AC/VC mode, the ventilator assists the patient’s breathing by delivering a preset volume of air with each breath, ensuring a consistent tidal volume Tidal volume The volume of air inspired or expired during each normal, quiet respiratory cycle. Common abbreviations are tv or V with subscript t. Ventilation: Mechanics of Breathing. If the patient initiates a breath, the ventilator will assist by delivering the set tidal volume Tidal volume The volume of air inspired or expired during each normal, quiet respiratory cycle. Common abbreviations are tv or V with subscript t. Ventilation: Mechanics of Breathing. If the patient does not initiate a breath within a certain time frame, the ventilator will deliver breaths at a preset rate to maintain ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing. AC/VC is commonly used in the intensive care unit ( ICU ICU Hospital units providing continuous surveillance and care to acutely ill patients. West Nile Virus) for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with various respiratory conditions.
PS/ CPAP CPAP A technique of respiratory therapy, in either spontaneously breathing or mechanically ventilated patients, in which airway pressure is maintained above atmospheric pressure throughout the respiratory cycle by pressurization of the ventilatory circuit. Noninvasive Ventilation refers to pressure support/continuous positive airway Airway ABCDE Assessment pressure. It is a combined mode of ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing that provides both CPAP CPAP A technique of respiratory therapy, in either spontaneously breathing or mechanically ventilated patients, in which airway pressure is maintained above atmospheric pressure throughout the respiratory cycle by pressurization of the ventilatory circuit. Noninvasive Ventilation and pressure support. CPAP CPAP A technique of respiratory therapy, in either spontaneously breathing or mechanically ventilated patients, in which airway pressure is maintained above atmospheric pressure throughout the respiratory cycle by pressurization of the ventilatory circuit. Noninvasive Ventilation maintains a continuous positive airway Airway ABCDE Assessment pressure to keep the airways open, while pressure support is an additional level of pressure delivered during inspiration Inspiration Ventilation: Mechanics of Breathing to assist the patient’s effort to breathe. PS/ CPAP CPAP A technique of respiratory therapy, in either spontaneously breathing or mechanically ventilated patients, in which airway pressure is maintained above atmospheric pressure throughout the respiratory cycle by pressurization of the ventilatory circuit. Noninvasive Ventilation is often used when a patient needs both maintenance of airway Airway ABCDE Assessment patency and pressure support to assist with respiratory effort, such as in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with neuromuscular diseases or during weaning from mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing.
VCV stands for volume-controlled ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing. In VCV (also known as AC/VC) mode, the ventilator controls and delivers a fixed volume of gas, and the patient’s respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination and effort determine the frequency and timing of breaths. This mode is particularly useful for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with specific tidal volume Tidal volume The volume of air inspired or expired during each normal, quiet respiratory cycle. Common abbreviations are tv or V with subscript t. Ventilation: Mechanics of Breathing requirements, such as those with acute respiratory distress syndrome Acute Respiratory Distress Syndrome Acute respiratory distress syndrome is characterized by the sudden onset of hypoxemia and bilateral pulmonary edema without cardiac failure. Sepsis is the most common cause of ARDS. The underlying mechanism and histologic correlate is diffuse alveolar damage (DAD). Acute Respiratory Distress Syndrome (ARDS) (ARDS) or patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship undergoing surgery. VCV allows precise control over the delivered tidal volume Tidal volume The volume of air inspired or expired during each normal, quiet respiratory cycle. Common abbreviations are tv or V with subscript t. Ventilation: Mechanics of Breathing, helping to maintain consistent ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing.