Obstructive sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep apnea (OSA) is a disorder characterized by recurrent obstruction of the upper airway Airway ABCDE Assessment during sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep, causing hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage and fragmented sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep. Obstructive sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep apnea is due to a partial or complete collapse of the upper airway Airway ABCDE Assessment and is associated with snoring, restlessness, sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep interruption, and daytime somnolence. The diagnosis relies on medical history, and polysomnography Polysomnography Simultaneous and continuous monitoring of several parameters during sleep to study normal and abnormal sleep. The study includes monitoring of brain waves, to assess sleep stages, and other physiological variables such as breathing, eye movements, and blood oxygen levels which exhibit a disrupted pattern with sleep disturbances. Physiology of Sleep can confirm the diagnosis. Management includes lifestyle changes, methods of positive airway Airway ABCDE Assessment pressure, and surgical intervention.
Last updated: May 17, 2024
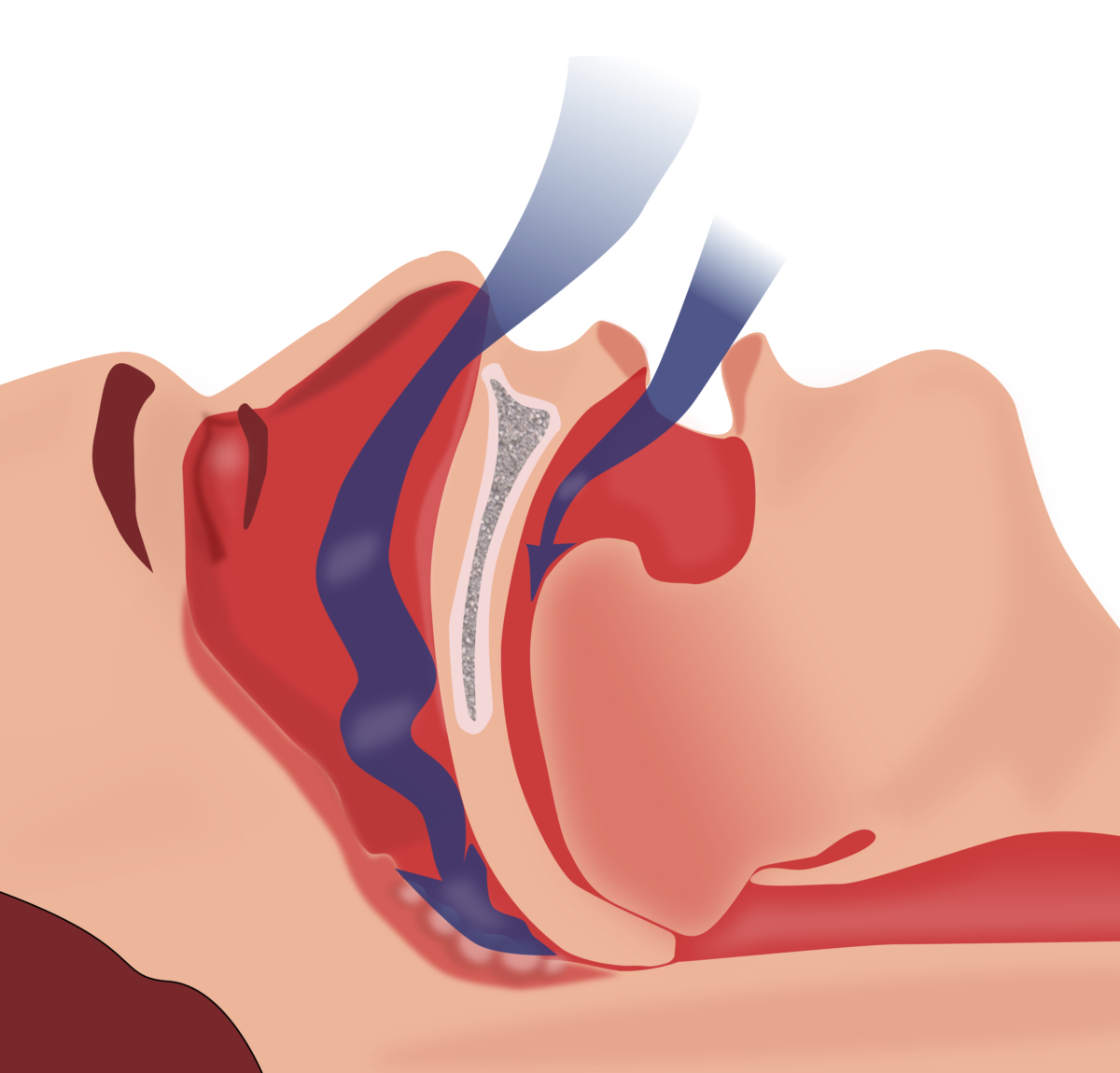
Illustration of the obstruction of ventilation. Note how the collapse of the pharyngeal muscles and backward placement of the tongue prevent the passage of air.
Image: “Illustration of obstruction of ventilation” by Habib M’henni. License: Public Domain, edited by Lecturio.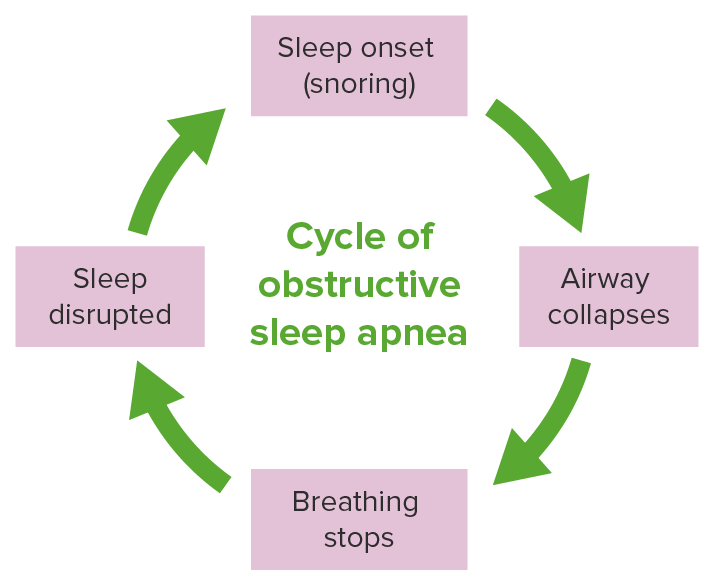
The pathological cycle of obstructive sleep apnea
Image by Lecturio.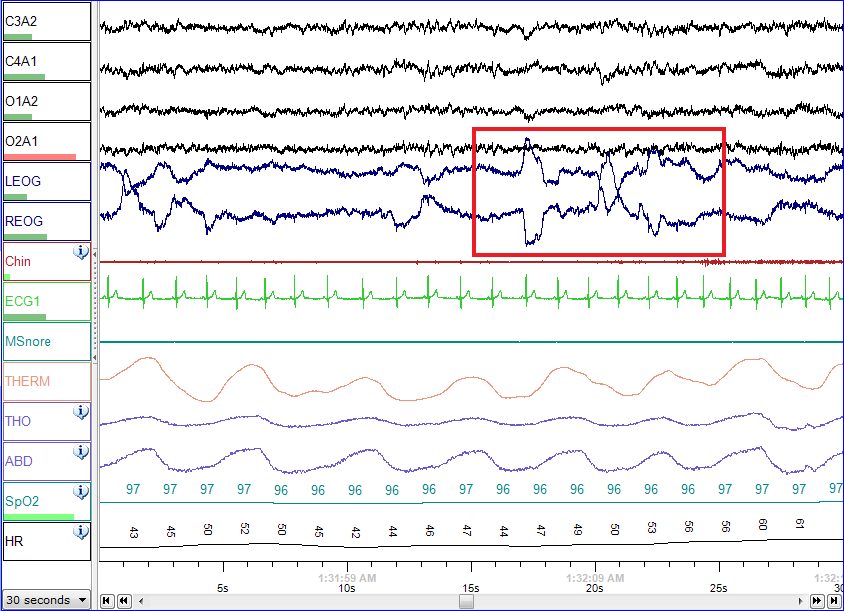
Normal polysomnographic record of REM sleep. Eye movements are highlighted by the red rectangle.
Image: “Screenshot of a PSG of a person in REM sleep” by NascarEd. License: CC BY-SA 3.0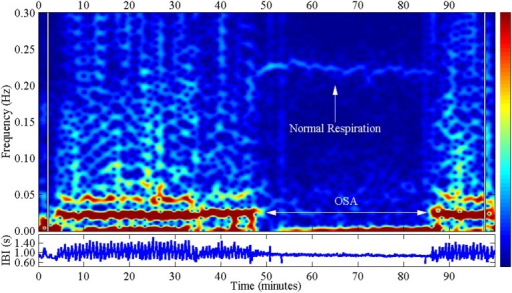
Spectral analysis of the cyclical variation in heart rate with obstructive sleep apnea from a polysomnography. Notice the difference between normal respiration and OSA.
Image: “Spectral analysis of the cyclical variation in heart rate with obstructive sleep apnea” by U.S. National Library of Medicine. License: CC BY 4.0Improving modifiable risk factors:
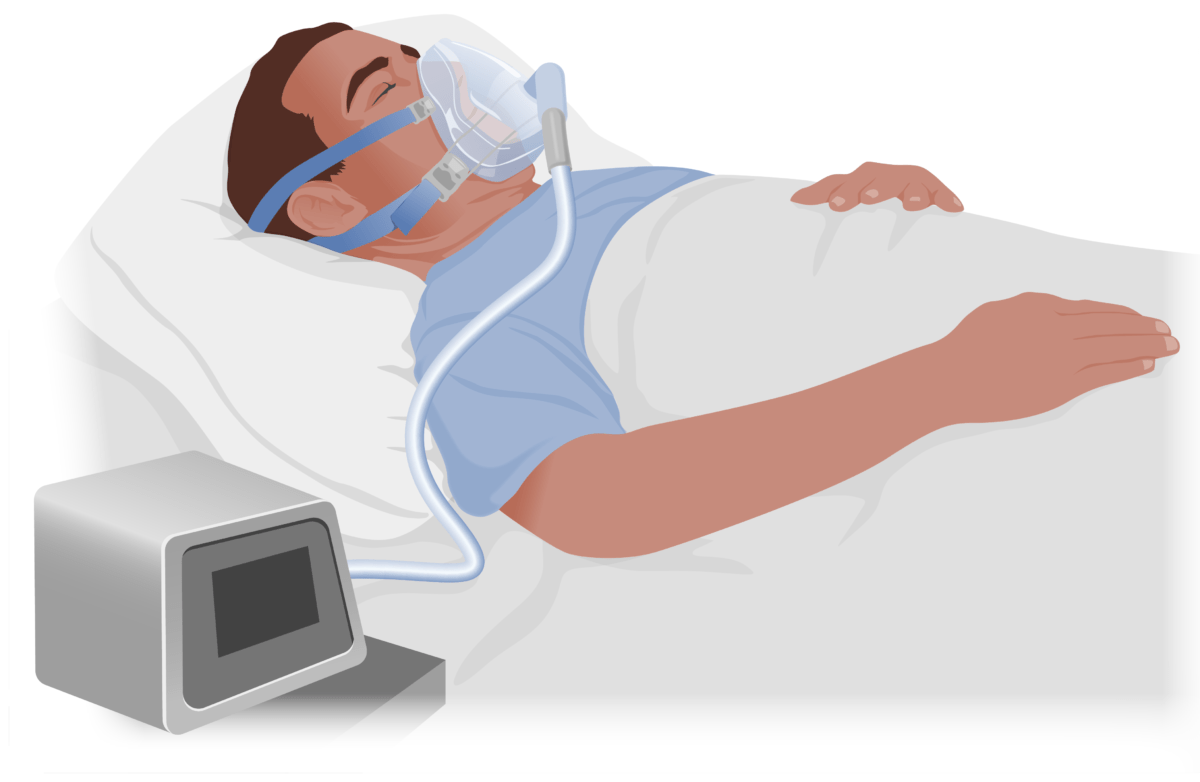
A continuous positive airway machine worn by a sleeping patient with obstructive sleep apnea. Notice how this would cause a low adherence rate due to the bulkiness of the mask and noise of the machine.
Image by Lecturio.Possible complications of obstructive sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep apnea: