Total anomalous pulmonary venous return (TAPVR) is a cyanotic congenital heart defect wherein the pulmonary veins Pulmonary veins The veins that return the oxygenated blood from the lungs to the left atrium of the heart. Lungs: Anatomy drain into anatomical sites other than the left atrium. The most common sub-type is the supra cardiac form, where the drainage is into the superior vena cava Superior vena cava The venous trunk which returns blood from the head, neck, upper extremities and chest. Mediastinum and Great Vessels: Anatomy. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are usually cyanotic from birth and present with respiratory and heart failure right after birth. On examination there is a fixed, wide split-second heart sound, and a chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests might reveal the “snowman” sign. Diagnosis is confirmed by an echocardiogram Echocardiogram Transposition of the Great Arteries, which can be prenatal. All patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship require surgery for survival and medical management is used to bridge the gap to surgery.
Last updated: Mar 19, 2025
Total anomalous pulmonary venous return (TAPVR) is a cyanotic congenital heart defect that results in the drainage of the 4 pulmonary veins Pulmonary veins The veins that return the oxygenated blood from the lungs to the left atrium of the heart. Lungs: Anatomy into the systemic venous circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment, rather than into the left atrium, resulting in mixing of oxygenated and deoxygenated blood. An interatrial defect ( ASD ASD Autism spectrum disorder (ASD) is a neurodevelopmental disorder marked by poor social skills, restricted interests/social interactions, and repetitive/stereotyped behaviors. The condition is termed a “spectrum” because of the wide variability in the severity of symptoms exhibited. Autism Spectrum Disorder, PFO PFO A patent foramen ovale (PFO) is an abnormal communication between the atria that persists after birth. The condition results from incomplete closure of the foramen ovale. Small, isolated, and asymptomatic pfos are a common incidental finding on echocardiography and require no treatment. Patent Foramen Ovale, or PDA PDA The ductus arteriosus (DA) allows blood to bypass pulmonary circulation. After birth, the DA remains open for up to 72 hours and then constricts and involutes, becoming the ligamentum arteriosum. Failure of this process to occur results in patent ductus arteriosus (PDA), a condition that causes up to 10% of congenital heart defects. Patent Ductus Arteriosus (PDA)) must be present to allow mixed blood to shunt to the left side of the heart and the systemic arterial circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment.
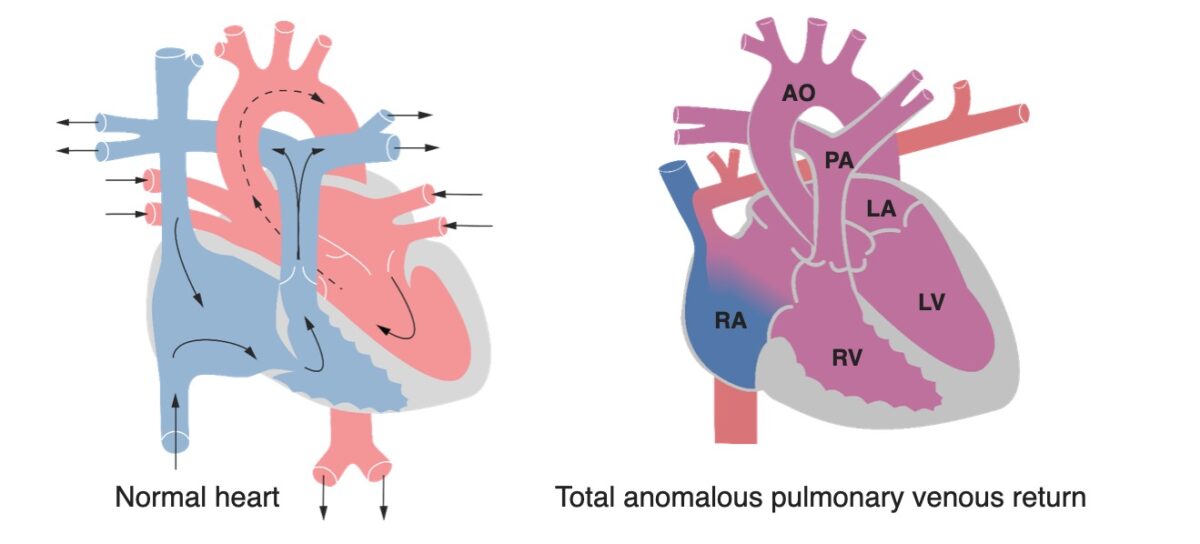
A heart with normal anatomy versus a heart with total anomalous pulmonary venous return:
The most common form of TAPVR features the 4 pulmonary veins draining into the superior vena cava (SVC) as shown here. Notice the increased size of the right ventricular wall, due to progressive ventricular overload.
This condition arises due to the failure of the left atrium to merge with the pulmonary venous plexus during fetal development.
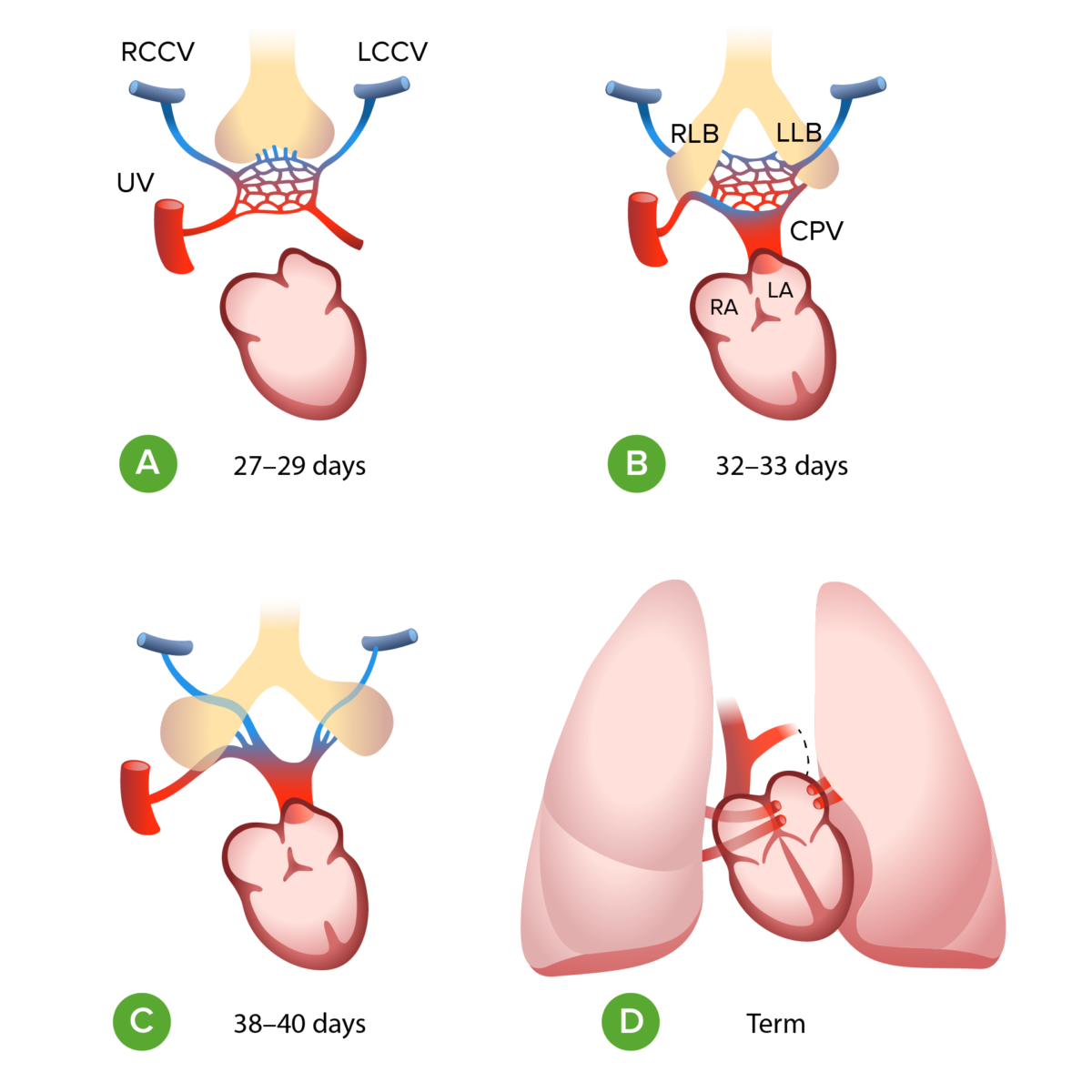
A: During the first month of gestation the left and right common cardinal vein (LCCV, RCCV) and the umbilical vein (UV) drain the splanchnic plexus (the primitive pulmonary vasculature) into the fetal heart.
B: At the end of the first month of gestation the embryonal left atrium (LA) gives rise to common pulmonary vein (CPV) which merges with the venous plexus
C: The connection to the LCCV, RCCV and UV disappear
D: CPV splits into 4 and is incorporated into the wall of the left atrium
RA: right atrium
LLB: left lung bud
RLB: right lung bud
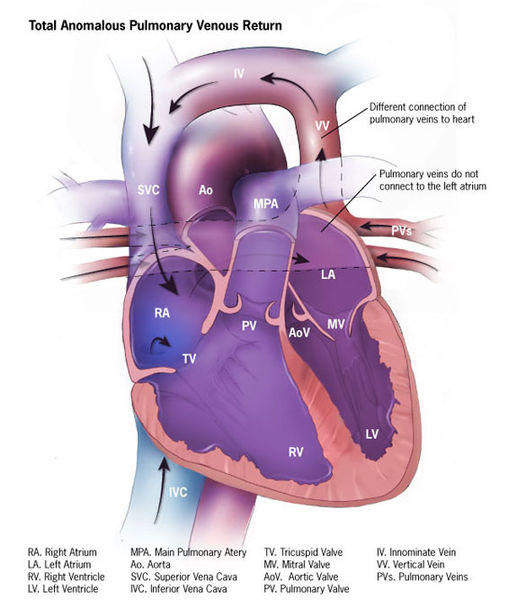
Blood mixing in total anomalous pulmonary venous return:
In TAPVR, oxygenated blood from the lungs returns to the systemic venous circulation mixing with deoxygenated blood. This mixed blood then shunts to the left side of the heart through an atrial septum defect and flows to the rest of the body resulting in cyanosis.
The degree of obstruction of pulmonary veins Pulmonary veins The veins that return the oxygenated blood from the lungs to the left atrium of the heart. Lungs: Anatomy determines the age of presentation:
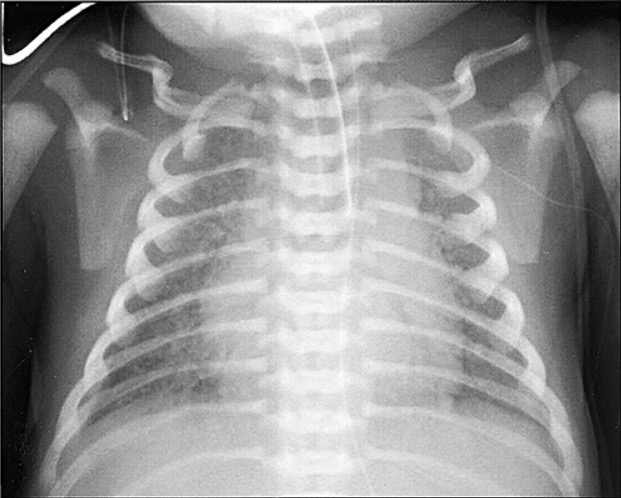
Total anomalous pulmonary vein drainage: marked pulmonary congestion and diffuse bilateral reticulogranular infiltrates
Image: “Total anomalous pulmonary vein drainage” by Departments of Pathology and Cell Biology, School of Medicine, University of Occupational and Environmental Health, Fukuoka Shin Mizumaki Hospital, Kitakyushu, Japan. License: CC BY 2.5