Coarctation of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy is a narrowing of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy between the aortic arch Aortic arch Mediastinum and Great Vessels: Anatomy and the iliac bifurcation commonly around the point of insertion of the ductus arteriosus Ductus arteriosus A fetal blood vessel connecting the pulmonary artery with the descending aorta. Patent Ductus Arteriosus (PDA). Coarctation of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy is typically congenital and the clinical presentation depends on the age of the patient. Neonates present with heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) upon the closure of the ductus arteriosus Ductus arteriosus A fetal blood vessel connecting the pulmonary artery with the descending aorta. Patent Ductus Arteriosus (PDA), while children and adults present with hypoperfusion and/or hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension. Classic findings on physical exam include radio-/brachio-femoral delay and decreased blood pressure in the lower limbs. Diagnosis is confirmed by echocardiogram Echocardiogram Transposition of the Great Arteries. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship should be surgically managed as early as possible to avoid complications of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension. Close follow-up is required as the risk of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension and re-coarctation remain.
Last updated: Apr 26, 2025
Coarctation of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy is a narrowing of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy caused by the thickening of the medial layer at a localized point, most commonly near the insertion of the ductus arteriosus Ductus arteriosus A fetal blood vessel connecting the pulmonary artery with the descending aorta. Patent Ductus Arteriosus (PDA).
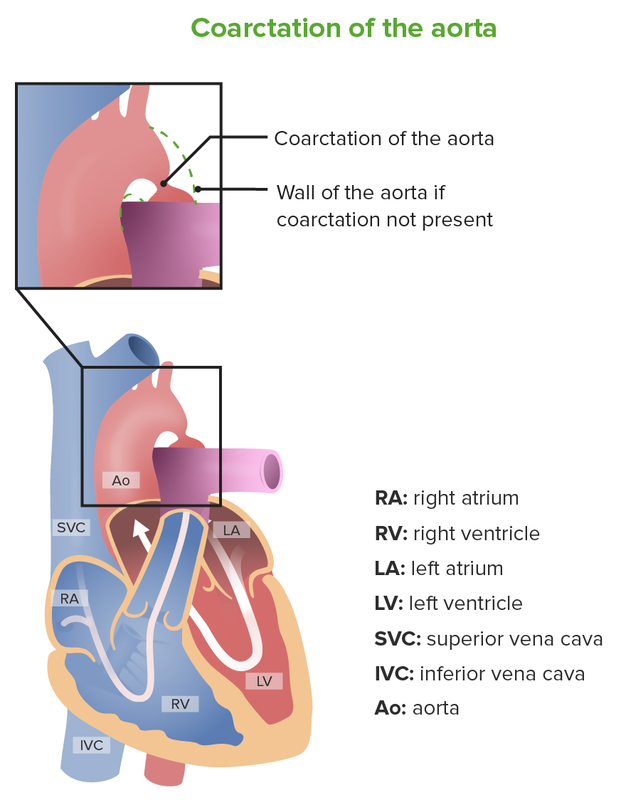
Schematic representation of coarctation of the aorta
Image by Lecturio.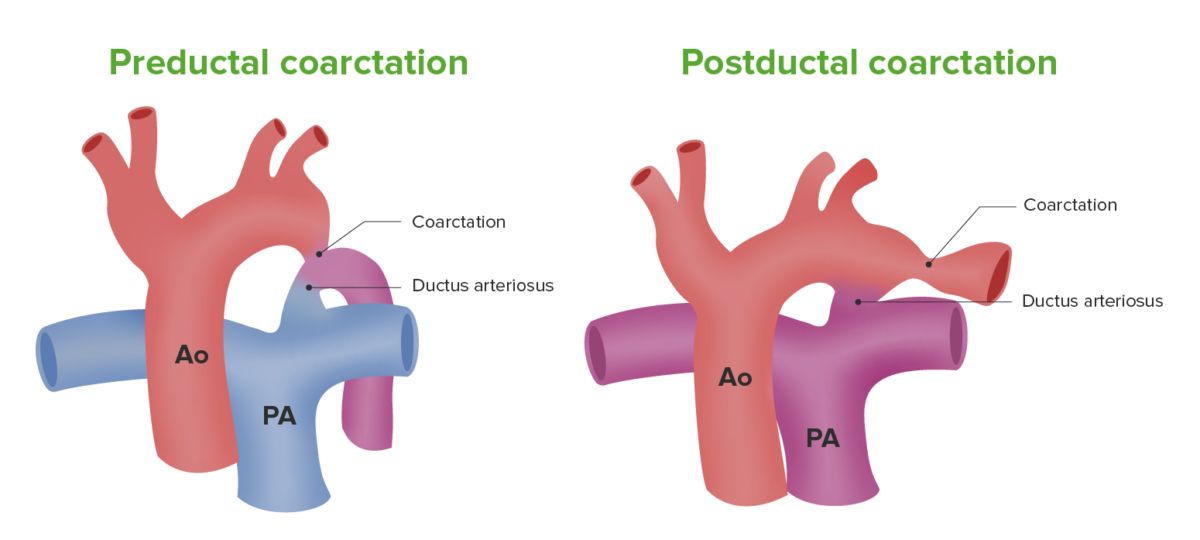
Types of coarctation of the aorta
Image by Lecturio.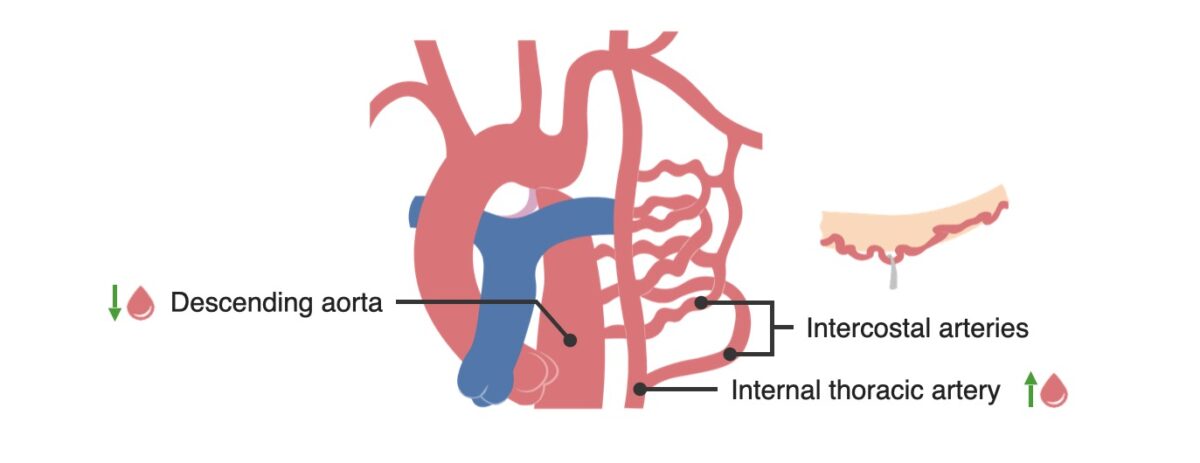
Collateral circulation composed of the inferior intercostal vessels develops to bypass the coarctation, which results in rib notching.
Image by Lecturio.Findings:
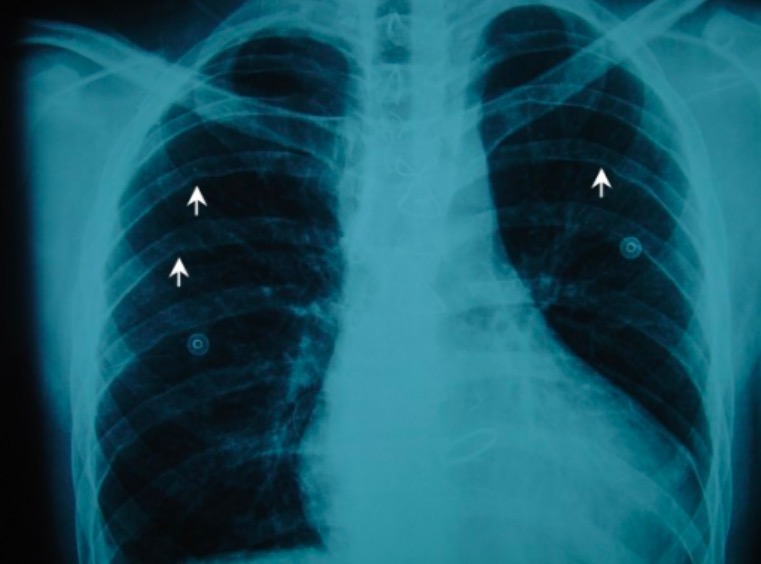
Chest X-ray shows rib notching on the undersurface of the posterior ribs (white arrows).
Image: “Chest X-ray” by Department of Cardiothoracic Surgery, School of Medicine, University of Patras, Patras, Greece. License: CC BY 2.0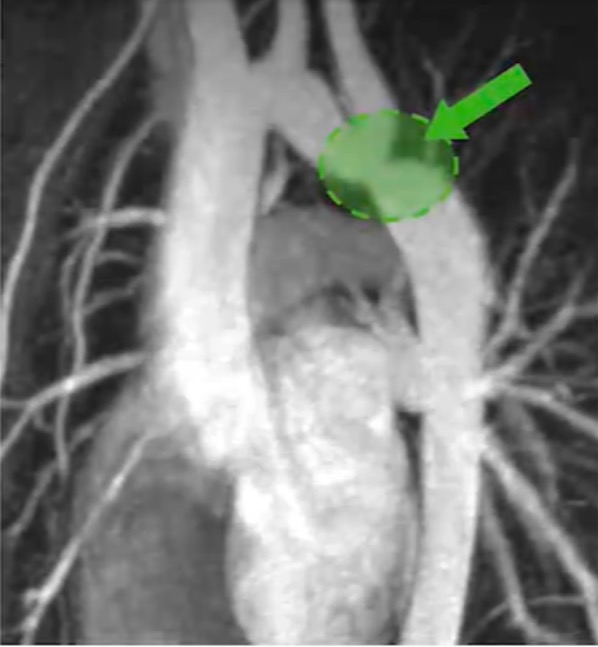
Computed tomography (CT) angiography showing coarctation of the aorta.
Image: “Magnetic resonance imaging” by Children’s Hospital Heart Center, Department of Pediatrics, University of Virginia, USA. License: CC BY 2.5, edited by Lecturio.Neonates:
Children and adults:
A few long-term complications can develop postsurgical repair:
Postoperative follow-up: Annual consult and imaging, such as an echocardiogram Echocardiogram Transposition of the Great Arteries, is required to detect complications.
The differential diagnosis of coarctation of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy must be considered depending on the age group of the patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.
Since patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present in shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock, other causes such as septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock or hypovolemic shock Hypovolemic Shock Types of Shock must be ruled out.
If a young girl is diagnosed with coarctation, karyotyping Karyotyping Mapping of the karyotype of a cell. Chromosome Testing for Turner syndrome Turner syndrome Turner syndrome is a genetic condition affecting women, in which 1 X chromosome is partly or completely missing. The classic result is the karyotype 45,XO with a female phenotype. Turner syndrome is associated with decreased sex hormone levels and is the most common cause of primary amenorrhea. Turner Syndrome must be performed as it accounts for 15% of cases.
Turner syndrome Turner syndrome Turner syndrome is a genetic condition affecting women, in which 1 X chromosome is partly or completely missing. The classic result is the karyotype 45,XO with a female phenotype. Turner syndrome is associated with decreased sex hormone levels and is the most common cause of primary amenorrhea. Turner Syndrome: a genetic condition in which 1 X chromosome X chromosome The female sex chromosome, being the differential sex chromosome carried by half the male gametes and all female gametes in human and other male-heterogametic species. Basic Terms of Genetics is partly or completely missing, resulting in karyotype Karyotype The full set of chromosomes presented as a systematized array of metaphase chromosomes from a photomicrograph of a single cell nucleus arranged in pairs in descending order of size and according to the position of the centromere. Congenital Malformations of the Female Reproductive System 45,X0. Presentation includes primary amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System (characteristic of a woman with short stature), webbed neck Webbed neck Turner Syndrome, broad chest, and widely spaced nipples. Genetic testing Genetic Testing Detection of a mutation; genotype; karyotype; or specific alleles associated with genetic traits, heritable diseases, or predisposition to a disease, or that may lead to the disease in descendants. It includes prenatal genetic testing. Myotonic Dystrophies confirms the diagnosis, and treatment is based on hormone replacement.
A delay in pulse may also be seen in peripheral arterial disease and aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection.