Migraine headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess is a primary headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess disorder and is among the most prevalent disorders in the world. Migraine is characterized by episodic, moderate to severe headaches that may be associated with increased sensitivity to light and sound, as well as nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and/or vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia. A migraine attack might be preceded by a so-called aura—neurologic phenomena of visual, auditory, sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology, or motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement. There is a strong hereditary component in the etiology of migraines. Migraine headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess is a clinical diagnosis with several variants. Management strategies include abortive therapy such as NSAIDs NSAIDS Primary vs Secondary Headaches and triptans Triptans Triptans and ergot alkaloids are agents used mainly for the management of acute migraines. The therapeutic effect is induced by binding to serotonin receptors, which causes reduced vasoactive neuropeptide release, pain conduction, and intracranial vasoconstriction. Triptans and Ergot Alkaloids to manage acute episodes as well as preventive strategies to minimize morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and pain-related disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman's compensation benefits. ABCDE Assessment.
Last updated: Feb 9, 2024
Migraine headaches are primary headaches Primary headaches Conditions in which the primary symptom is headache and the headache cannot be attributed to any known causes. Primary vs Secondary Headaches commonly associated with nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, photophobia, phonophobia Phonophobia Specific Phobias, and exacerbated by physical activity.
Distinguishing features:
Migraine-related terminology:
Migraine headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess is classified among the primary headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess disorders as well as having subtypes of its own.
Primary headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess disorders:
Subtypes of migraine headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess:
Current consensus holds that a primary neuronal dysfunction is responsible for a sequence of intracranial and extracranial changes that trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation prodromic and postdromic symptoms, aura, and the headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess itself.
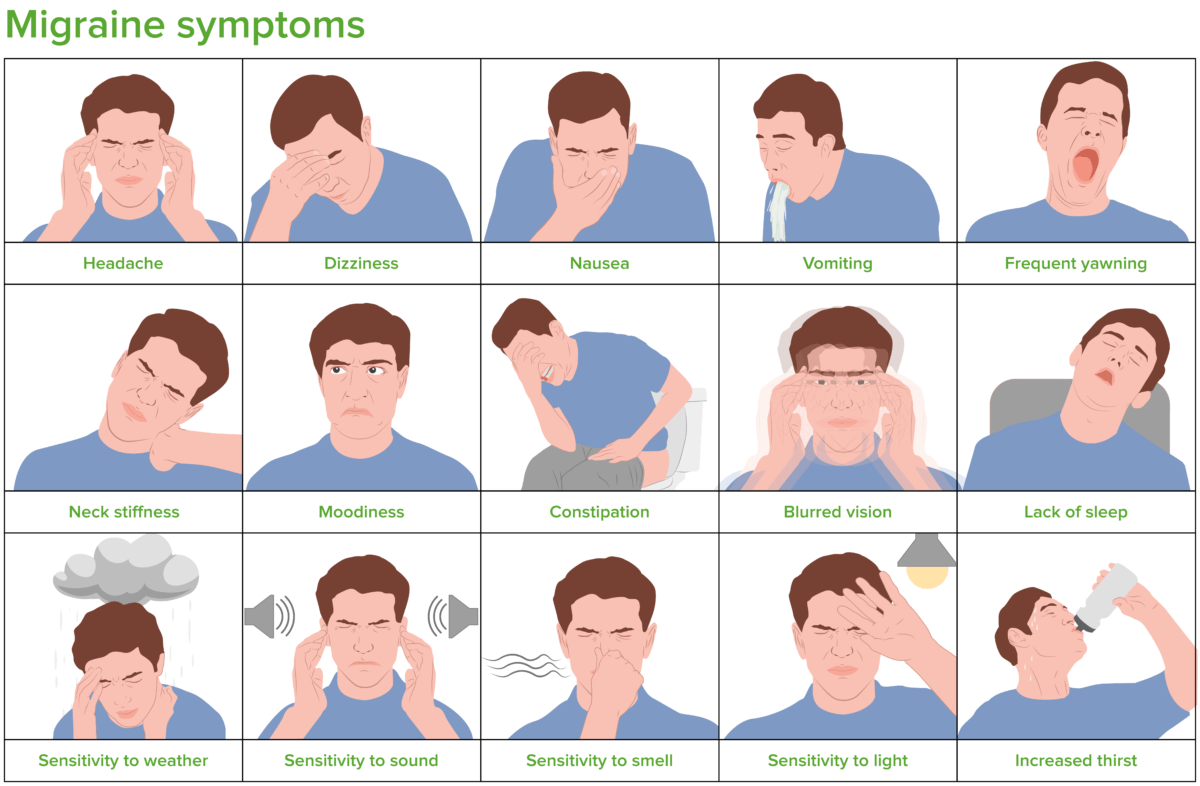
Illustration showing the clinical presentation of migraine
Image by Lecturio.Physical examination may be entirely normal unless the individual is currently experiencing an attack.
Aura symptoms:
During an attack:
General:
To diagnose migraine, there should have been ≥ 5 attacks meeting ≥ 2 of the following criteria:
Migraine with aura:
To diagnose migraine with aura, 3 of the 6 following features must be present:
Regardless of the abortive strategy used, allowing the migraine sufferer to lie down in a dark, quiet room is favorable.
Goals:
Indications:
Preventive treatment options: