Ménière disease is a condition characterized by episodes of vertigo Vertigo Vertigo is defined as the perceived sensation of rotational motion while remaining still. A very common complaint in primary care and the ER, vertigo is more frequently experienced by women and its prevalence increases with age. Vertigo is classified into peripheral or central based on its etiology. Vertigo, tinnitus Tinnitus A nonspecific symptom of hearing disorder characterized by the sensation of buzzing, ringing, clicking, pulsations, and other noises in the ear. Objective tinnitus refers to noises generated from within the ear or adjacent structures that can be heard by other individuals. The term subjective tinnitus is used when the sound is audible only to the affected individual. Tinnitus may occur as a manifestation of cochlear diseases; vestibulocochlear nerve diseases; intracranial hypertension; craniocerebral trauma; and other conditions. Cranial Nerve Palsies, and hearing loss Hearing loss Hearing loss, also known as hearing impairment, is any degree of impairment in the ability to apprehend sound as determined by audiometry to be below normal hearing thresholds. Clinical presentation may occur at birth or as a gradual loss of hearing with age, including a short-term or sudden loss at any point. Hearing Loss, likely caused by endolymphatic hydrops Hydrops Cholecystitis of the labyrinthine system in the inner ear Inner ear The essential part of the hearing organ consists of two labyrinthine compartments: the bony labyrinthine and the membranous labyrinth. Ear: Anatomy. Risk factors include a family history Family History Adult Health Maintenance of Ménière disease, preexisting autoimmune disorders, allergies Allergies A medical specialty concerned with the hypersensitivity of the individual to foreign substances and protection from the resultant infection or disorder. Selective IgA Deficiency, and trauma to the head or ear. The diagnosis is made clinically by audiometry, vestibular testing Vestibular Testing Vertigo, and, occasionally, imaging. Management consists of diet and lifestyle modification, vasodilators Vasodilators Drugs used to cause dilation of the blood vessels. Thromboangiitis Obliterans (Buerger Disease), diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication, antihistamines Antihistamines Antihistamines are drugs that target histamine receptors, particularly H1 and H2 receptors. H1 antagonists are competitive and reversible inhibitors of H1 receptors. First-generation antihistamines cross the blood-brain barrier and can cause sedation. Antihistamines, benzodiazepines Benzodiazepines Benzodiazepines work on the gamma-aminobutyric acid type A (GABAA) receptor to produce inhibitory effects on the CNS. Benzodiazepines do not mimic GABA, the main inhibitory neurotransmitter in humans, but instead potentiate GABA activity. Benzodiazepines, antiemetics Antiemetics Antiemetics are medications used to treat and/or prevent nausea and vomiting. These drugs act on different target receptors. The main classes include benzodiazepines, corticosteroids, atypical antipsychotics, cannabinoids, and antagonists of the following receptors: serotonin, dopamine, and muscarinic and neurokinin receptors. Antiemetics, glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids, surgical intervention, and/or hearing aids AIDS Chronic HIV infection and depletion of CD4 cells eventually results in acquired immunodeficiency syndrome (AIDS), which can be diagnosed by the presence of certain opportunistic diseases called AIDS-defining conditions. These conditions include a wide spectrum of bacterial, viral, fungal, and parasitic infections as well as several malignancies and generalized conditions. HIV Infection and AIDS.
Last updated: Jan 13, 2023
Ménière disease is a triad of episodic vertigo Vertigo Vertigo is defined as the perceived sensation of rotational motion while remaining still. A very common complaint in primary care and the ER, vertigo is more frequently experienced by women and its prevalence increases with age. Vertigo is classified into peripheral or central based on its etiology. Vertigo, tinnitus Tinnitus A nonspecific symptom of hearing disorder characterized by the sensation of buzzing, ringing, clicking, pulsations, and other noises in the ear. Objective tinnitus refers to noises generated from within the ear or adjacent structures that can be heard by other individuals. The term subjective tinnitus is used when the sound is audible only to the affected individual. Tinnitus may occur as a manifestation of cochlear diseases; vestibulocochlear nerve diseases; intracranial hypertension; craniocerebral trauma; and other conditions. Cranial Nerve Palsies, and hearing loss Hearing loss Hearing loss, also known as hearing impairment, is any degree of impairment in the ability to apprehend sound as determined by audiometry to be below normal hearing thresholds. Clinical presentation may occur at birth or as a gradual loss of hearing with age, including a short-term or sudden loss at any point. Hearing Loss likely caused by endolymphatic hydrops Hydrops Cholecystitis of the labyrinthine system of the inner ear Inner ear The essential part of the hearing organ consists of two labyrinthine compartments: the bony labyrinthine and the membranous labyrinth. Ear: Anatomy.
Ménière syndrome is Ménière disease occurring secondary to other inner ear Inner ear The essential part of the hearing organ consists of two labyrinthine compartments: the bony labyrinthine and the membranous labyrinth. Ear: Anatomy infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease.
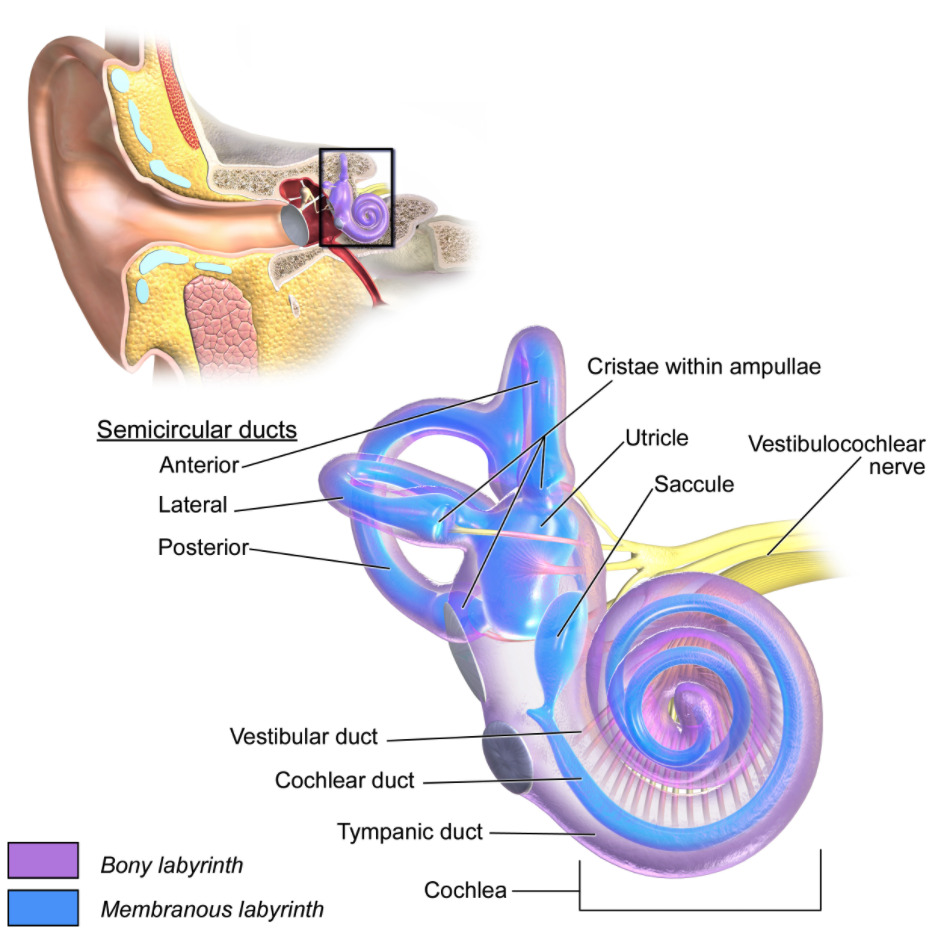
Anatomy of the inner ear
Image: “The internal ear” by BruceBlaus. License: CC BY 3.0Clinical diagnosis made by the presence of:
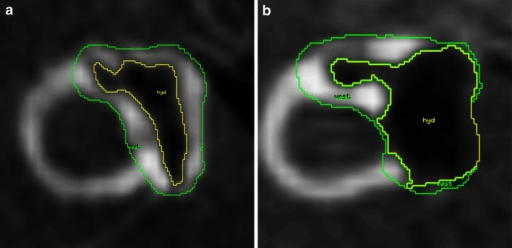
MRI of endolymphatic hydrops (EH) in patients with Ménière disease:
a: corresponding-to-mild EH
b: corresponding-to-significant EH
Treatment improves and relieves symptoms but does not correct the underlying pathophysiology.