Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Associated symptoms, including fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, weight loss Weight loss Decrease in existing body weight. Bariatric Surgery, and bloody stools are also important to elicit from the history. Most causes of acute diarrhea are infectious and do not require additional workup. Since diarrhea is usually a self-limited condition, management is generally supportive. However, chronic diarrhea can require laboratory studies, stool studies, imaging, or procedures to determine the cause. Management ultimately hinges on treating the underlying pathology, though symptomatic and empiric therapies may be utilized under the right circumstances.
Last updated: May 17, 2024
Diarrhea is the passage of ≥ 3 watery or loose stools in 24 hours.
Diarrhea can be classified by the duration of symptoms:
Additionally, diarrhea may be classified based on the underlying etiology and pathophysiology:
Inflammatory/invasive:
Noninflammatory/noninvasive:
Risk factors:
Secretory:
Osmotic:
Malabsorption Malabsorption General term for a group of malnutrition syndromes caused by failure of normal intestinal absorption of nutrients. Malabsorption and Maldigestion:
Inflammatory/exudative:
Altered motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility:
Inflammatory/invasive:
Noninflammatory/noninvasive:
Secretory:
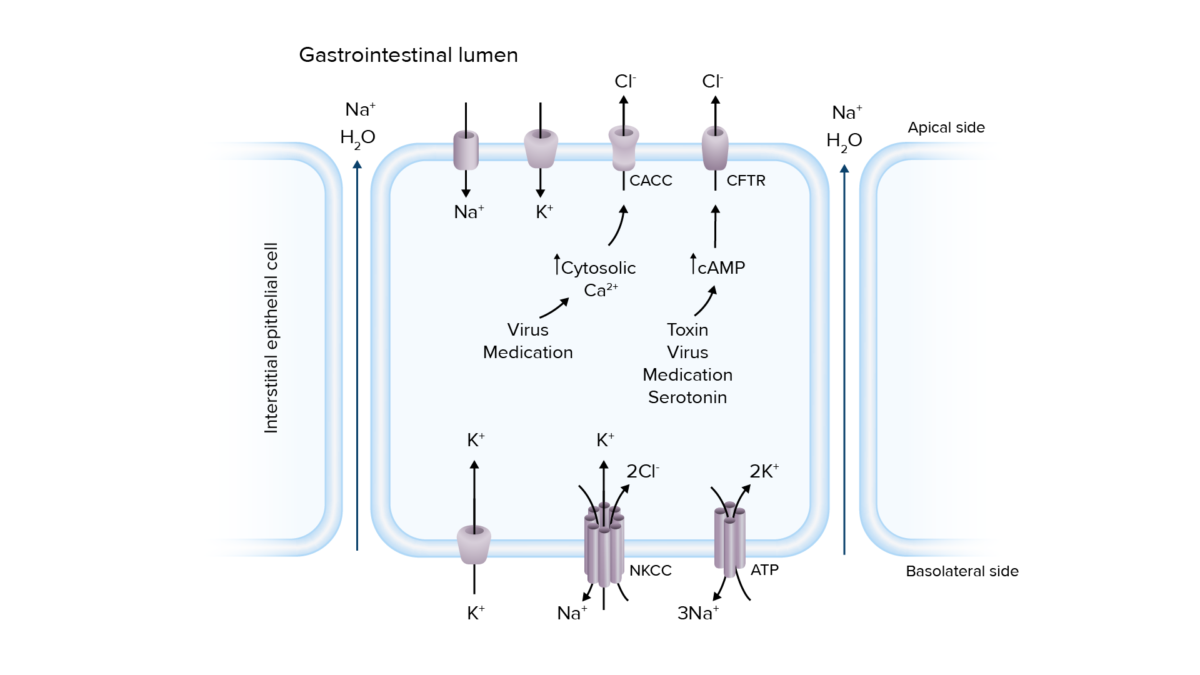
Pathogenesis of secretory diarrhea:
Overactivation of ion transport channels can lead to secretion of electrolytes and water into the intestinal lumen, resulting in diarrhea.
Ca2+: calcium
CaCC: calcium-activated chloride channels
cAMP: cyclic adenosine monophosphate
CFTR: cystic fibrosis transmembrane conductance regulator
Cl−: chloride
K+: potassium
Na+: sodium
NKCC: sodium–potassium chloride cotransporter
Osmotic:
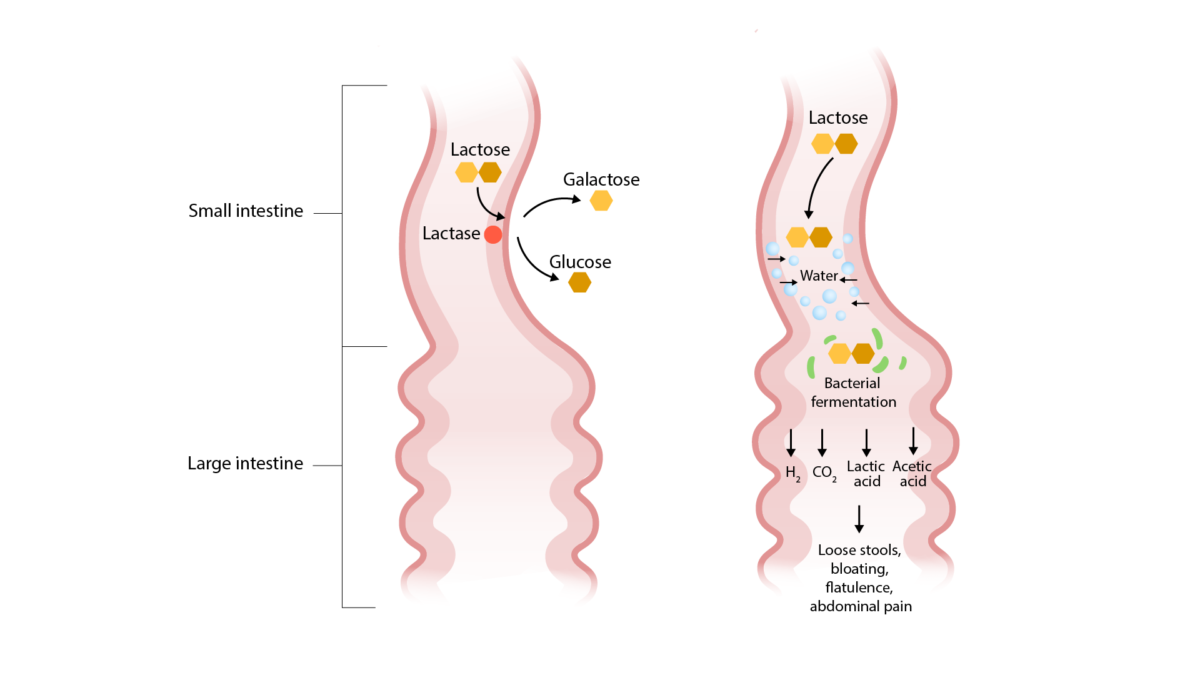
Pathogenesis of lactase deficiency (an etiology of osmotic diarrhea):
Lactose is not broken down and remains in the small intestinal lumen, drawing in water and causing osmotic diarrhea. Bacterial fermentation of lactose results in the symptoms of bloating, flatulence, and abdominal pain.
Malabsorption Malabsorption General term for a group of malnutrition syndromes caused by failure of normal intestinal absorption of nutrients. Malabsorption and Maldigestion:
Inflammatory/exudative:
Altered motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility: rapid intestinal passage → ↓ time for fluid absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption
The majority of cases are infectious in etiology.
Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will have self-limiting Self-Limiting Meningitis in Children symptoms and do not require testing.
Indications for stool studies:
Stool analysis:
Supporting laboratory evaluation:
The differential diagnosis of chronic diarrhea is lengthy, and the evaluation will be guided by clinical suspicion from the history and physical exam. Consultation with a gastroenterologist may be needed.
Laboratory studies:
Imaging and procedures:
Supportive care:
Antidiarrheal Antidiarrheal Antidiarrheal agents include several drug classes, including opioid agonists, somatostatin analogues, adsorbents, and bile acid sequestrants. These medications mainly work through antimotility and/or antisecretory effects. Antidiarrheal Drugs agents:
Antibiotic therapy:
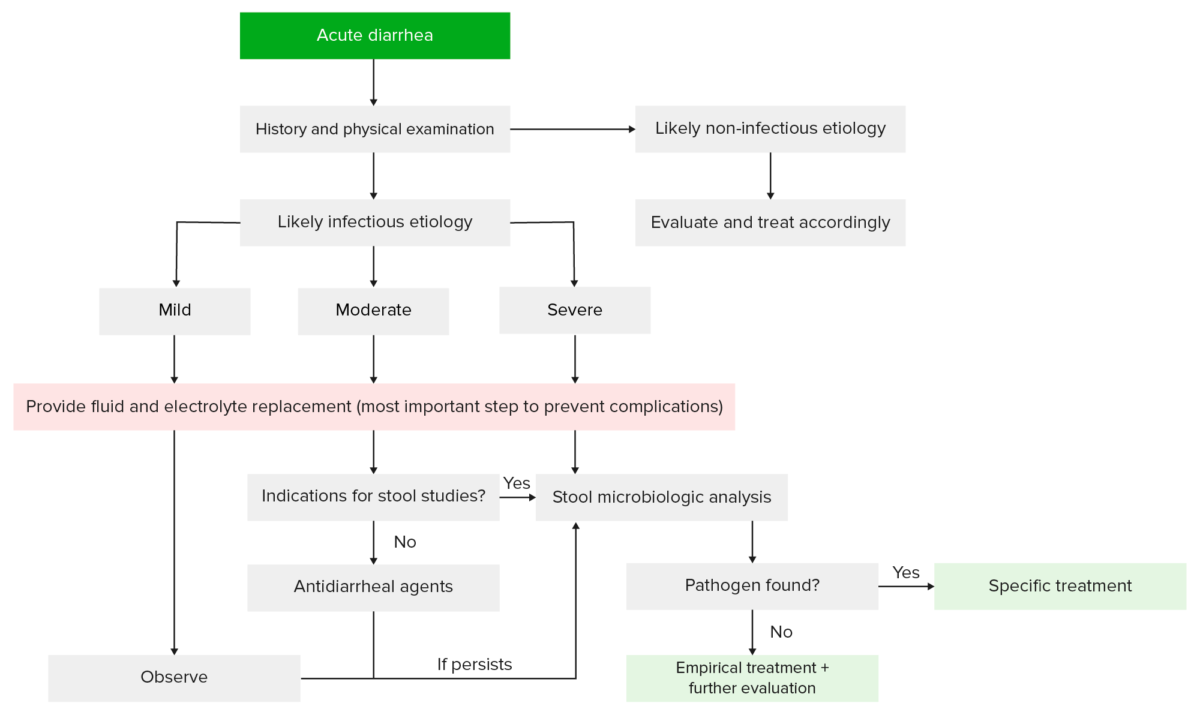
Evaluation and management of patients with acute diarrhea:
Based on the history and physical exam, a determination can be made about whether the diarrhea is related to an infectious or a noninfectious etiology (e.g., medications). Most patients will not require more than supportive care. However, those with indications for further workup may undergo laboratory and stool testing, which can help guide further therapy.
The treatment of chronic diarrhea hinges on diagnosing and treating the underlying etiology.
Symptomatic therapy:
Empiric therapy Empiric Therapy Meningitis in Children:

Melanosis coli, due to laxative abuse, as seen on colonoscopy
Image: “Black pigmentation of colonic mucosa” by University of Sidi Mohammed Ben Abdellah, Faculty of Medicine and Pharmacy, Department of gastroenterology C, Fez, Morocco. License: CC BY 2.0