A gastrinoma is a tumor Tumor Inflammation that secretes excessive levels of the hormone gastrin Gastrin A family of gastrointestinal peptide hormones that excite the secretion of gastric juice. They may also occur in the central nervous system where they are presumed to be neurotransmitters. Gastrointestinal Secretions and is responsible for Zollinger-Ellison syndrome Zollinger-ellison syndrome A syndrome that is characterized by the triad of severe peptic ulcer, hypersecretion of gastric acid, and gastrin-producing tumors of the pancreas or other tissue (gastrinoma). This syndrome may be sporadic or be associated with multiple endocrine neoplasia type 1. Esophagitis (ZES). Gastrinomas are frequently associated with multiple endocrine neoplasia Multiple endocrine neoplasia Multiple endocrine neoplasia syndromes are autosomal dominant inherited conditions characterized by 2 or more hormone-producing tumors involving the endocrine organs. There are different types of MEN, namely MEN1-4. Multiple Endocrine Neoplasia 1 (MEN 1) and can arise from the pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy, stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy, duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy, jejunum Jejunum The middle portion of the small intestine, between duodenum and ileum. It represents about 2/5 of the remaining portion of the small intestine below duodenum. Small Intestine: Anatomy, and/or even from the lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 - 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy. Gastrinoma tumors are often malignant and frequently metastasize to the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 - 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy, and bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types. Zollinger-Ellison syndrome Zollinger-ellison syndrome A syndrome that is characterized by the triad of severe peptic ulcer, hypersecretion of gastric acid, and gastrin-producing tumors of the pancreas or other tissue (gastrinoma). This syndrome may be sporadic or be associated with multiple endocrine neoplasia type 1. Esophagitis (ZES) is characterized by high gastrin Gastrin A family of gastrointestinal peptide hormones that excite the secretion of gastric juice. They may also occur in the central nervous system where they are presumed to be neurotransmitters. Gastrointestinal Secretions levels, elevated gastric acid Gastric acid Hydrochloric acid present in gastric juice. Gastroesophageal Reflux Disease (GERD) production, peptic ulcers, gastroesophageal reflux, and diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea. Diagnosis is based on fasting serum gastrin Gastrin A family of gastrointestinal peptide hormones that excite the secretion of gastric juice. They may also occur in the central nervous system where they are presumed to be neurotransmitters. Gastrointestinal Secretions levels. Management consists of surgical resection of the gastrinoma and/or symptomatic management for unresectable disease.
Last updated: Feb 25, 2025
A gastrinoma is a neuroendocrine tumor Tumor Inflammation associated with Zollinger-Ellison syndrome Zollinger-ellison syndrome A syndrome that is characterized by the triad of severe peptic ulcer, hypersecretion of gastric acid, and gastrin-producing tumors of the pancreas or other tissue (gastrinoma). This syndrome may be sporadic or be associated with multiple endocrine neoplasia type 1. Esophagitis (ZES), which secretes large amounts of gastrin Gastrin A family of gastrointestinal peptide hormones that excite the secretion of gastric juice. They may also occur in the central nervous system where they are presumed to be neurotransmitters. Gastrointestinal Secretions and overstimulates gastric acid Gastric acid Hydrochloric acid present in gastric juice. Gastroesophageal Reflux Disease (GERD) production causing severe peptic ulcers.
Gastrinomas are neuroendocrine tumors arising in the digestive tract.
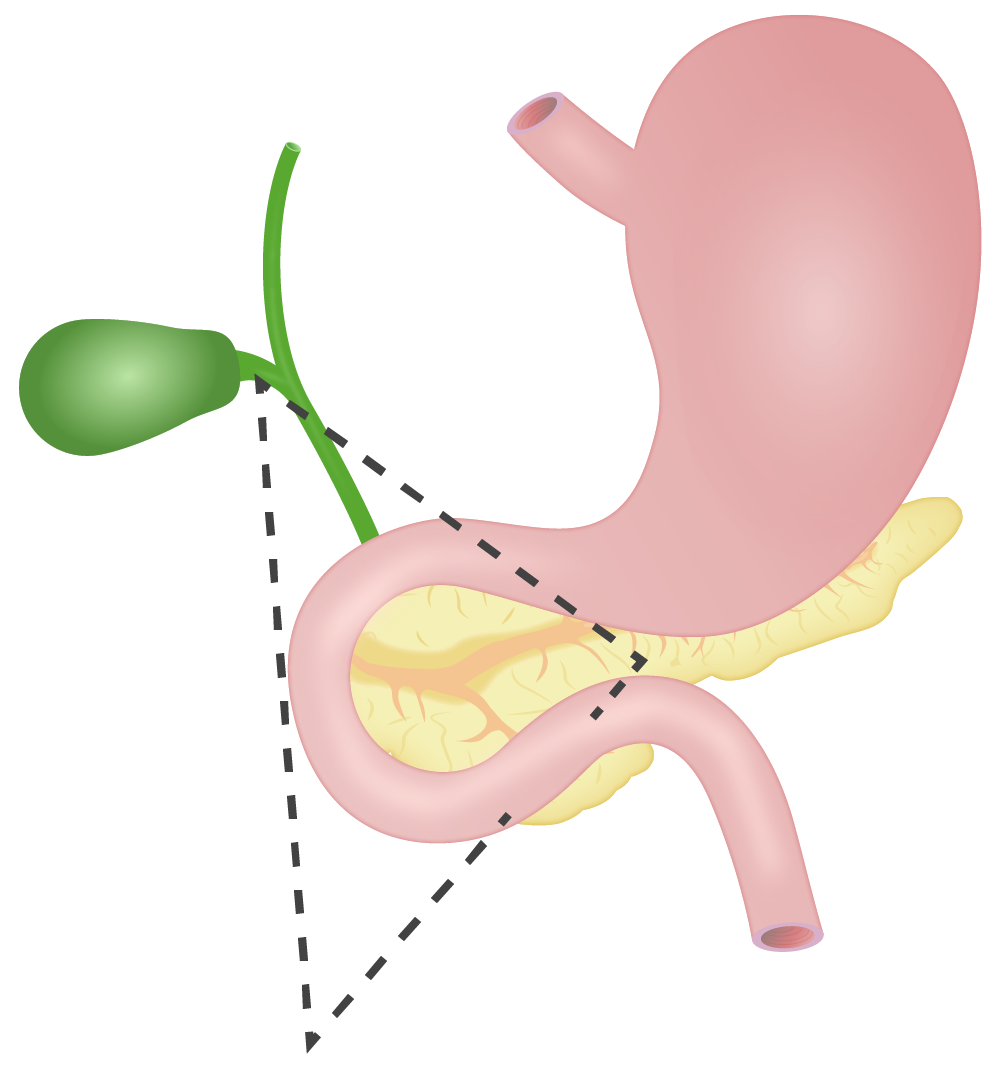
Passaro’s triangle:
Approximately 70%–90% of gastrinomas are found in the anatomical space known as “Passaro’s triangle”. The area is delineated by the junction of cystic and common bile ducts, the 2nd and 3rd portions of the duodenum, and the neck and body of the pancreas.
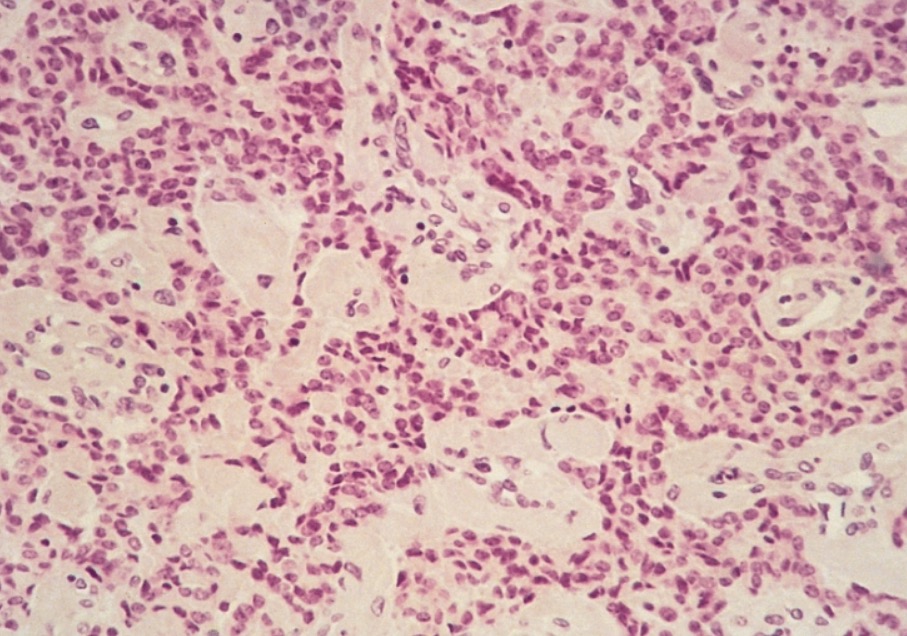
Pancreatic malignant gastrinoma showing a trabecular pattern
Image: “Gastrinoma” by The Armed Forces Institute of Pathology. License: Public DomainGastrinomas secrete excessive gastrin Gastrin A family of gastrointestinal peptide hormones that excite the secretion of gastric juice. They may also occur in the central nervous system where they are presumed to be neurotransmitters. Gastrointestinal Secretions:
Excessive gastric acid Gastric acid Hydrochloric acid present in gastric juice. Gastroesophageal Reflux Disease (GERD) results in:
If ZES is medically diagnosed, a gastrinoma must be identified.
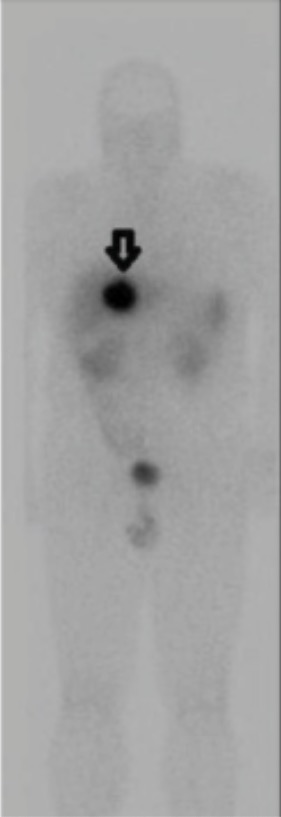
Somatostatin receptor scintigraphy (SRS) showing primary gastrinoma of the liver (arrow)
Image: “Anterior and posterior” by Division of General Surgery and Surgical Oncology, Department of Surgery and Oncology, University of Calgary, Calgary, Alberta T2N 2T9, Canada. License: CC BY 3.0, cropped by Lecturio.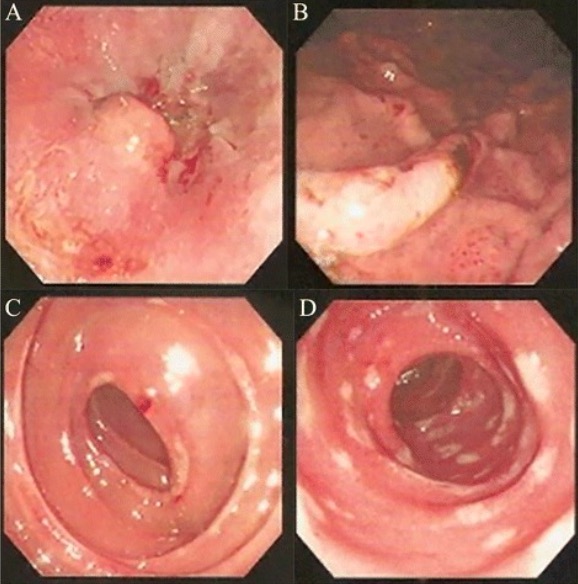
Endoscopic findings of ZES:
A: Reflux esophagitis
B: Gastric ulcers with hemorrhage
C: Duodenal erosions
D: Upper jejunal ulcers