Antidiarrheal agents include several drug classes, including opioid Opioid Compounds with activity like opiate alkaloids, acting at opioid receptors. Properties include induction of analgesia or narcosis. Constipation agonists, somatostatin Somatostatin A 14-amino acid peptide named for its ability to inhibit pituitary growth hormone release, also called somatotropin release-inhibiting factor. It is expressed in the central and peripheral nervous systems, the gut, and other organs. SRIF can also inhibit the release of thyroid-stimulating hormone; prolactin; insulin; and glucagon besides acting as a neurotransmitter and neuromodulator. In a number of species including humans, there is an additional form of somatostatin, srif-28 with a 14-amino acid extension at the n-terminal. Gastrointestinal Secretions analogues, adsorbents, and bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy acid sequestrants. These medications mainly work through antimotility and/or antisecretory effects. Somatostatin Somatostatin A 14-amino acid peptide named for its ability to inhibit pituitary growth hormone release, also called somatotropin release-inhibiting factor. It is expressed in the central and peripheral nervous systems, the gut, and other organs. SRIF can also inhibit the release of thyroid-stimulating hormone; prolactin; insulin; and glucagon besides acting as a neurotransmitter and neuromodulator. In a number of species including humans, there is an additional form of somatostatin, srif-28 with a 14-amino acid extension at the n-terminal. Gastrointestinal Secretions analogues are particularly helpful for secretory diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea due to endocrine hormone-producing malignancies, while bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy acid sequestrants can be used for conditions causing bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy acid malabsorption Malabsorption General term for a group of malnutrition syndromes caused by failure of normal intestinal absorption of nutrients. Malabsorption and Maldigestion diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea. Antidiarrheals can decrease the clearance of infectious pathogens and toxins and should be avoided in invasive infectious diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea.
Last updated: Dec 30, 2024
Diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea is the passage of ≥ 3 loose or liquid stools within 24 hours.
Classification:
General management:
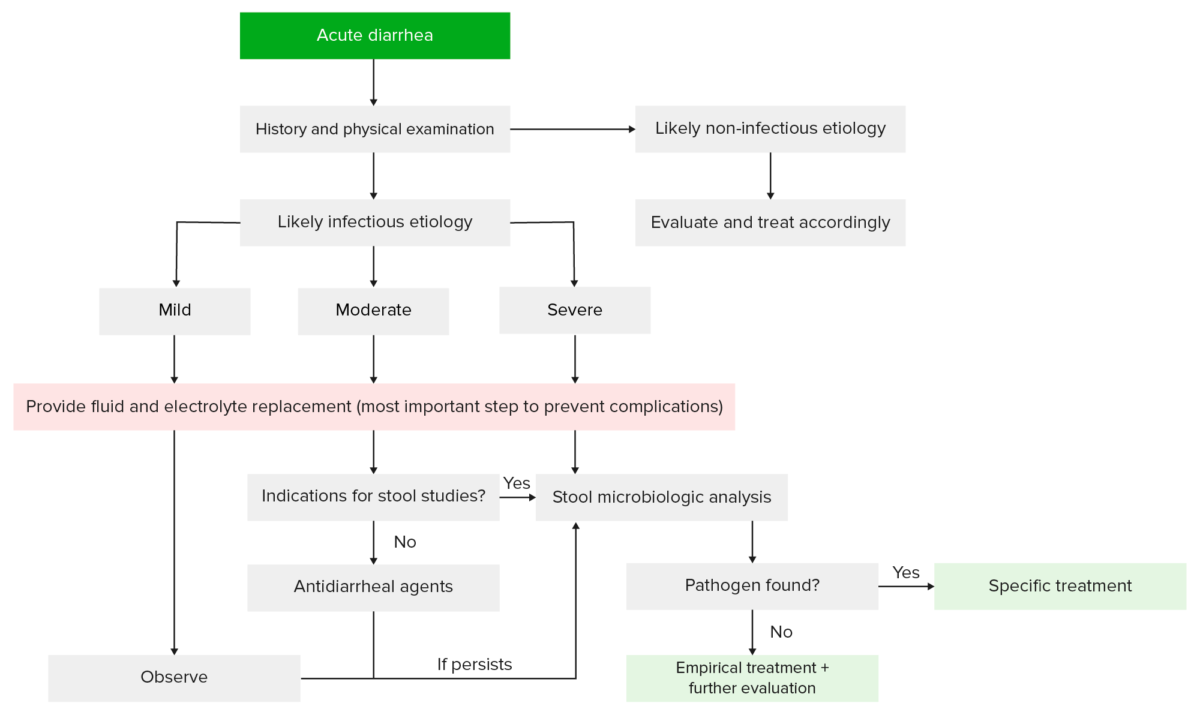
Evaluation and management of patients with acute diarrhea:
Based on the history and physical exam, a determination can be made about whether the diarrhea is related to an infectious or noninfectious etiology (e.g., medications). Most patients will not require more than supportive care. However, those with indications for further workup may undergo laboratory and stool testing, which can help guide further therapy.
These drug classes may improve symptoms of diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea via:
The opioid Opioid Compounds with activity like opiate alkaloids, acting at opioid receptors. Properties include induction of analgesia or narcosis. Constipation agonists utilized for their antidiarrheal activity are:
Loperamide:
Diphenoxylate:
These medications should be avoided in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with:
Bismuth subsalicylate should not be used for individuals with:
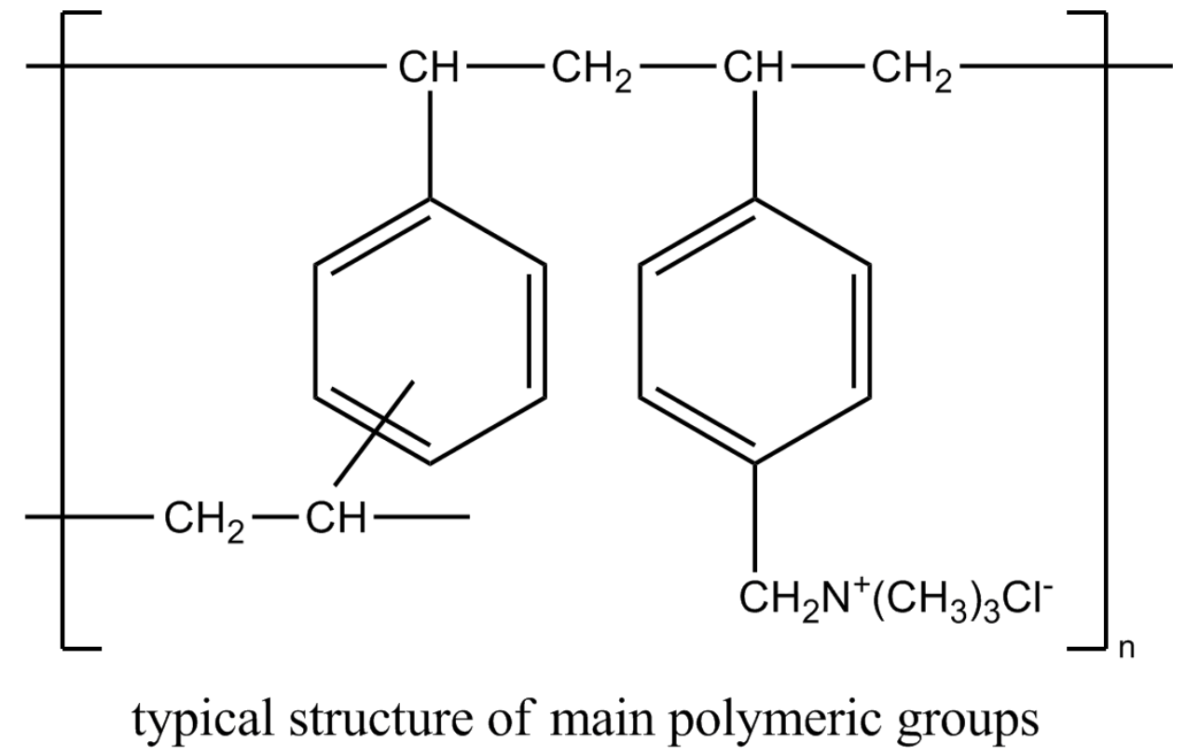
Chemical structure of cholestyramine
Image: “Cholestyramine” by Dahl J. License: CC0 1.0