Anal fistulas are abnormal communications between the anorectal lumen and another body structure, often to the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions. Anal fistulas often occur due to extension Extension Examination of the Upper Limbs of anal abscesses but are also associated with specific diseases such as Crohn's disease. Symptoms include pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways or irritation around the anus; abnormal discharge or purulent drainage; and swelling Swelling Inflammation, redness Redness Inflammation, or fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever if an abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease is present. Management is primarily surgical, with fistulotomy, but can include antibiotics if infection is present. Complications after surgery include recurrence and incontinence.
Last updated: May 6, 2025
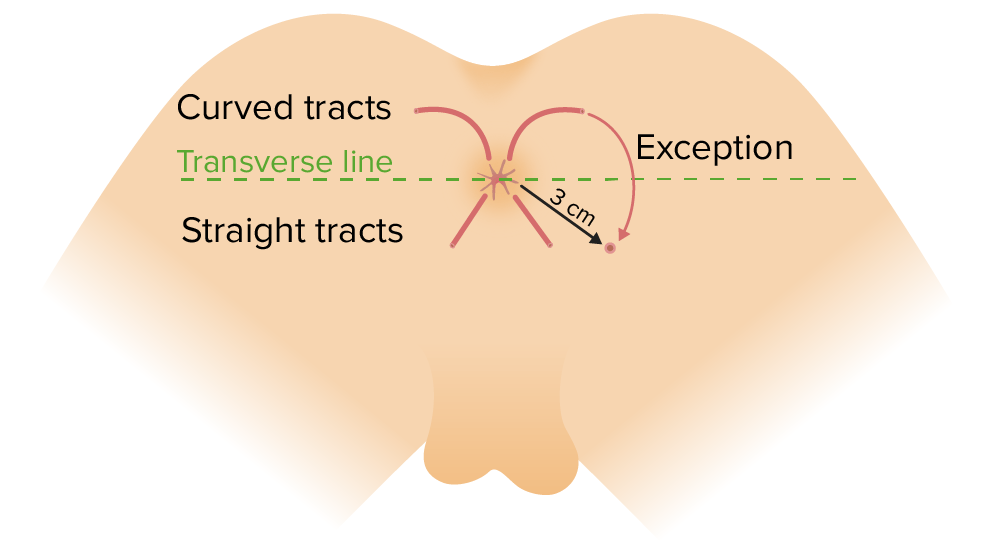
Goodsall rule:
Fistulas originating anterior to the transverse line through the anus will have a straight course and exit anteriorly (an exception to this rule includes anterior openings > 3 cm from the anal verge). Fistulas originating posterior to the transverse line will begin in the midline and have a curved tract.
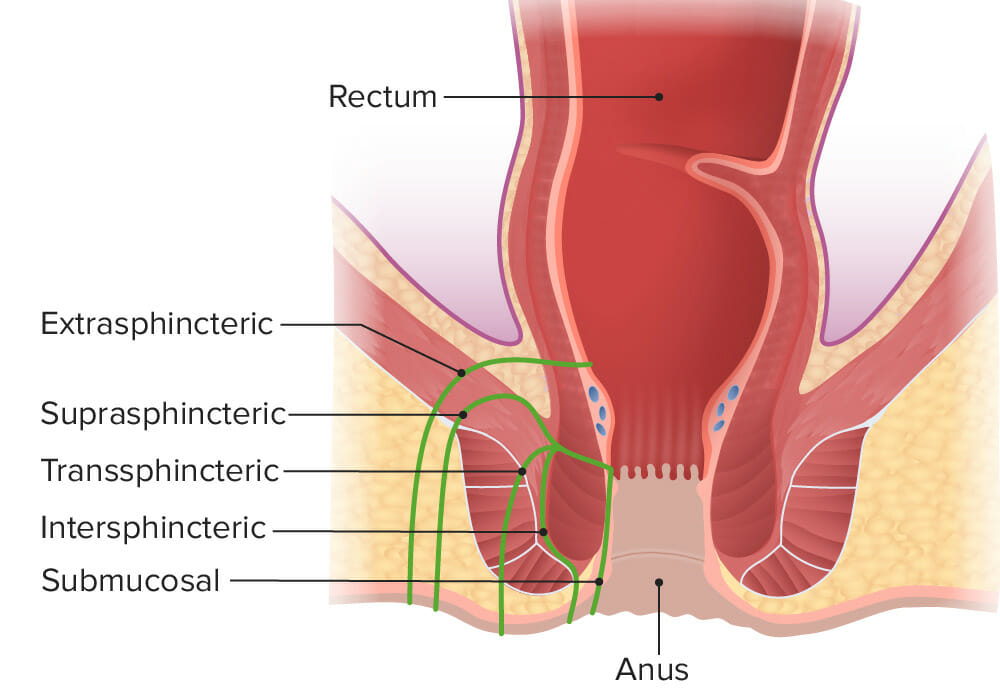
Types of fistula:
An intersphincteric (most common) fistula is located between the sphincters, which spares the external sphincter. A transsphincteric fistula goes through the internal and external sphincters, extending into the ischiorectal fossa. A suprasphincteric fistula penetrates the internal anal sphincter and tracks above the intersphincteric plane. An extrasphincteric fistula is high in the anal canal and tracks through the sphincter complex, going lateral to the sphincters before ending in the skin. A submucosal fistula does not penetrate any sphincter muscle.
Why fistulas stay open: “FRIENDS”
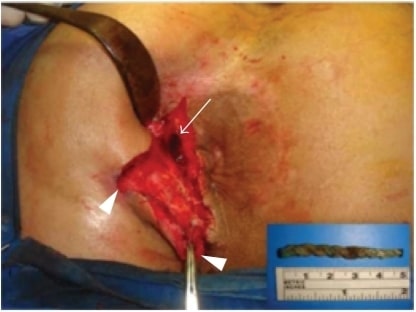
Intraoperative view of the external openings of the fistula-in-ano (arrow-heads) and the upper part of the tract, where the foreign material resided (arrow). The extracted nonabsorbable braided thread is shown in the inset figure.
Image: “Intraoperative view” by Department of General Surgery, Cerrahpasa Medical School, Istanbul University, Cerrahpasa, Fatih 34098, Istanbul, Turkey. License: CC BY 3.0