Bulimia nervosa is an eating disorder marked by recurrent episodes of binge eating Binge eating Binge eating is defined as consuming an amount of food in a specified amount of time (e.g., 1 hour) that greatly exceeds what most people would consume in that same amount of time. Binge Eating Disorder accompanied by inappropriate compensatory behaviors ( laxative Laxative Agents that produce a soft formed stool, and relax and loosen the bowels, typically used over a protracted period, to relieve constipation. Hypokalemia or diuretic use, self-induced vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, fasting, or excessive exercise) to counteract the effects of binge eating Binge eating Binge eating is defined as consuming an amount of food in a specified amount of time (e.g., 1 hour) that greatly exceeds what most people would consume in that same amount of time. Binge Eating Disorder and prevent weight gain. These episodes occur at least twice weekly for at least 3 months. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship have normal body weight (or are slightly overweight). Treatment consists of a combination of psychotherapy Psychotherapy Psychotherapy is interpersonal treatment based on the understanding of psychological principles and mechanisms of mental disease. The treatment approach is often individualized, depending on the psychiatric condition(s) or circumstance. Psychotherapy and pharmacotherapy.
Last updated: Mar 25, 2025
Bulimia nervosa is an eating disorder characterized by recurrent episodes of binge eating Binge eating Binge eating is defined as consuming an amount of food in a specified amount of time (e.g., 1 hour) that greatly exceeds what most people would consume in that same amount of time. Binge Eating Disorder (consuming a larger-than-appropriate amount of food in a set period of time) accompanied by inappropriate compensatory behavior Compensatory behavior Binge Eating Disorder (purging).
Specific exam findings can be suggestive of eating disorders:
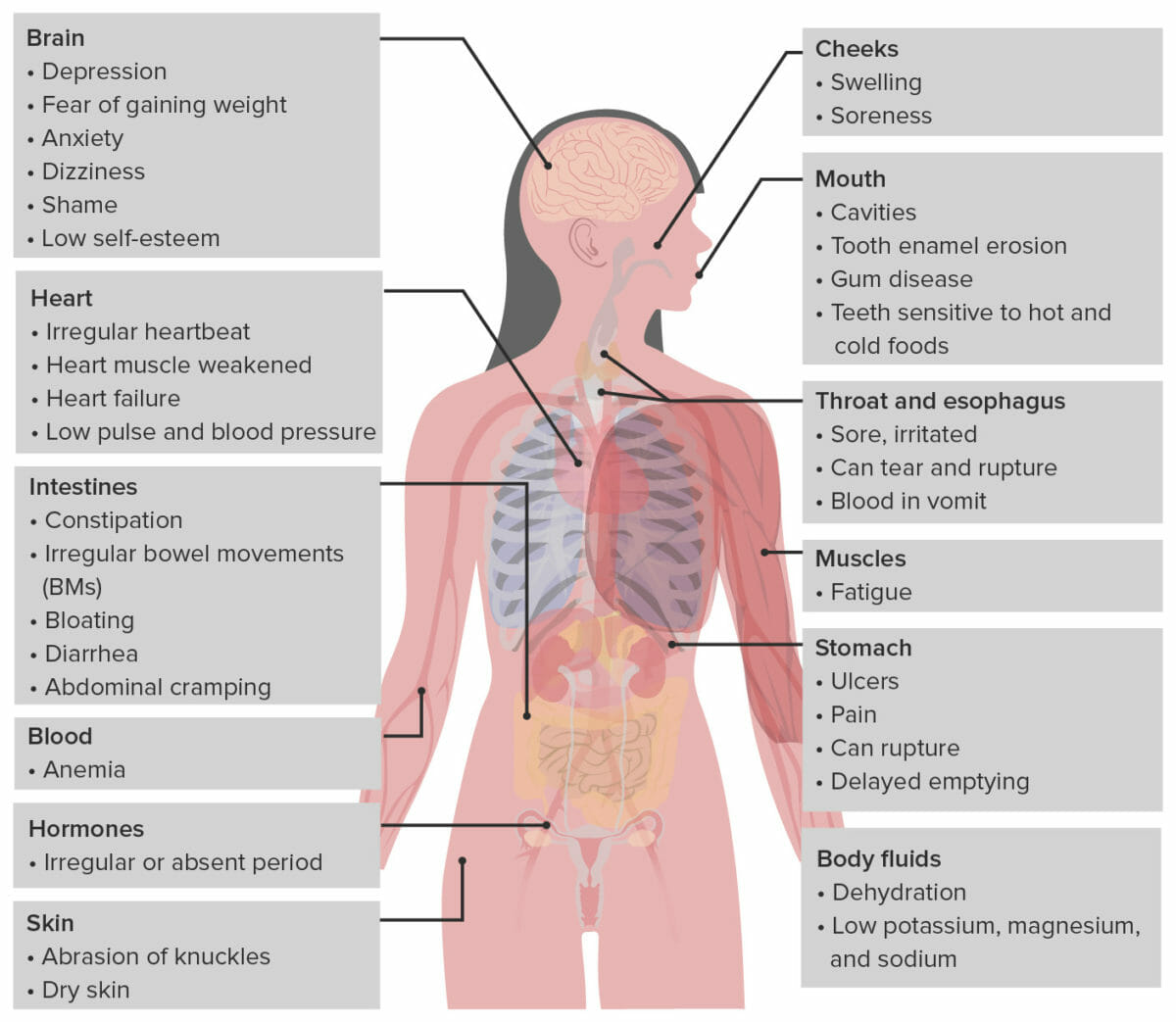
Illustration representing the effects of bulimia on different systems in the body
Image by Lecturio.Though not diagnostic, certain lab findings are suggestive of bulimia:
The 1st-line treatment is a combination of psychotherapy Psychotherapy Psychotherapy is interpersonal treatment based on the understanding of psychological principles and mechanisms of mental disease. The treatment approach is often individualized, depending on the psychiatric condition(s) or circumstance. Psychotherapy and pharmacotherapy.