Whipple's disease is a rare malabsorption syndrome with systemic manifestations (neurologic, cardiac, and musculoskeletal) caused by the bacterium Tropheryma whipplei. Patients often present with weight loss, diarrhea/steatorrhea, and arthralgias, as well as neurologic and cardiac manifestations. Whipple's disease is diagnosed with biopsy after the visualization of periodic acid–Schiff (PAS)-positive foamy macrophages in the involved tissues or with PCR for the bacterial DNA. It is managed with antibiotics, namely ceftriaxone or penicillin G and trimethoprim–sulfamethoxazole.
Last updated: May 7, 2025
Whipple’s disease is a malabsorption Malabsorption General term for a group of malnutrition syndromes caused by failure of normal intestinal absorption of nutrients. Malabsorption and Maldigestion syndrome with systemic manifestations that is caused by infection with Tropheryma whipplei.
Causative agent is T. whipplei:
Host immunodeficiency Immunodeficiency Chédiak-Higashi Syndrome has been implicated in symptomatic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease.

Endoscopic view of the jejunal mucosa in Whipple’s disease:
white lesions compatible with diffuse intestinal lymphangiectasia

T. whipplei–infected native mitral valve specimen:
transverse section of valve harboring voluminous bright yellow vegetations (arrowheads), up to 6 mm
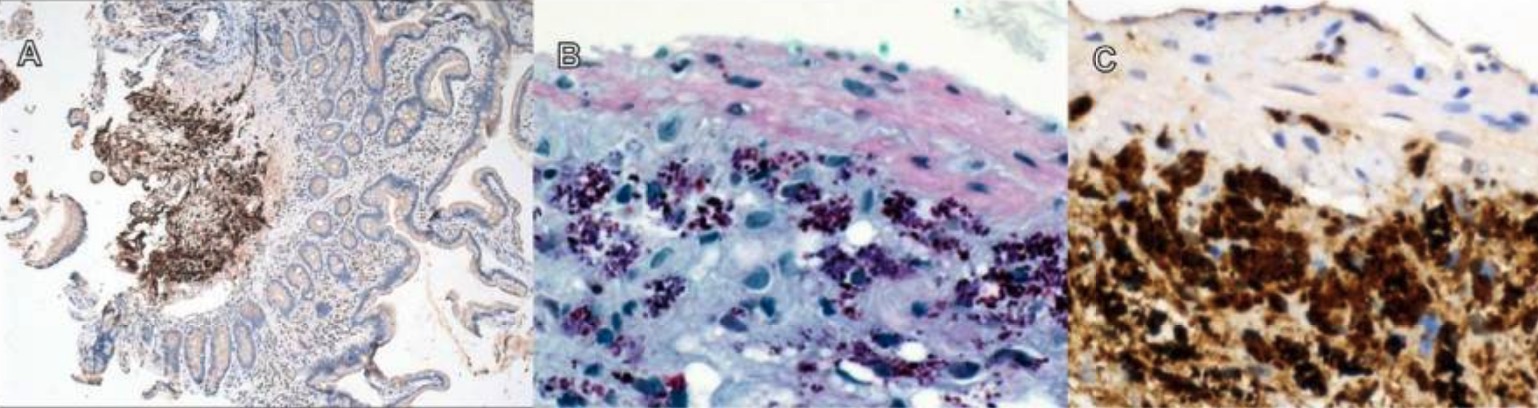
T. whipplei intestinal infection:
A: 40x magnification, T. whipplei immunostain visualized with hematoxylin
B: 400x magnification, PAS + macrophages
C: 400x magnification, dense submucosal aggregation of T. whipplei
The mainstay of treatment is antibiotics: