The human immunodeficiency Immunodeficiency Chédiak-Higashi Syndrome virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( HIV HIV Anti-HIV Drugs) is a species of Lentivirus, a genus of the family Retroviridae, which causes HIV HIV Anti-HIV Drugs infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease and acquired immunodeficiency Immunodeficiency Chédiak-Higashi Syndrome syndrome ( AIDS AIDS Chronic HIV infection and depletion of CD4 cells eventually results in acquired immunodeficiency syndrome (AIDS), which can be diagnosed by the presence of certain opportunistic diseases called AIDS-defining conditions. These conditions include a wide spectrum of bacterial, viral, fungal, and parasitic infections as well as several malignancies and generalized conditions. HIV Infection and AIDS). The virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology has high genetic variability and is divided into 2 major types, HIV HIV Anti-HIV Drugs type 1 Type 1 Spinal Muscular Atrophy ( HIV-1 HIV-1 The type species of lentivirus and the etiologic agent of aids. It is characterized by its cytopathic effect and affinity for the T4-lymphocyte. HIV Infection and AIDS) and HIV HIV Anti-HIV Drugs type 2 ( HIV-2 HIV-2 An HIV species related to HIV-1 but carrying different antigenic components and with differing nucleic acid composition. It shares serologic reactivity and sequence homology with the simian lentivirus simian immunodeficiency virus and infects only t4-lymphocytes expressing the CD4 phenotypic marker. HIV Infection and AIDS). The human immunodeficiency Immunodeficiency Chédiak-Higashi Syndrome virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology is a single-stranded, positive-sense, enveloped RNA RNA A polynucleotide consisting essentially of chains with a repeating backbone of phosphate and ribose units to which nitrogenous bases are attached. RNA is unique among biological macromolecules in that it can encode genetic information, serve as an abundant structural component of cells, and also possesses catalytic activity. RNA Types and Structure virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology, which targets and destroys WBCs, leading to frequent opportunistic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease and, eventually, death.
Last updated: Dec 29, 2023
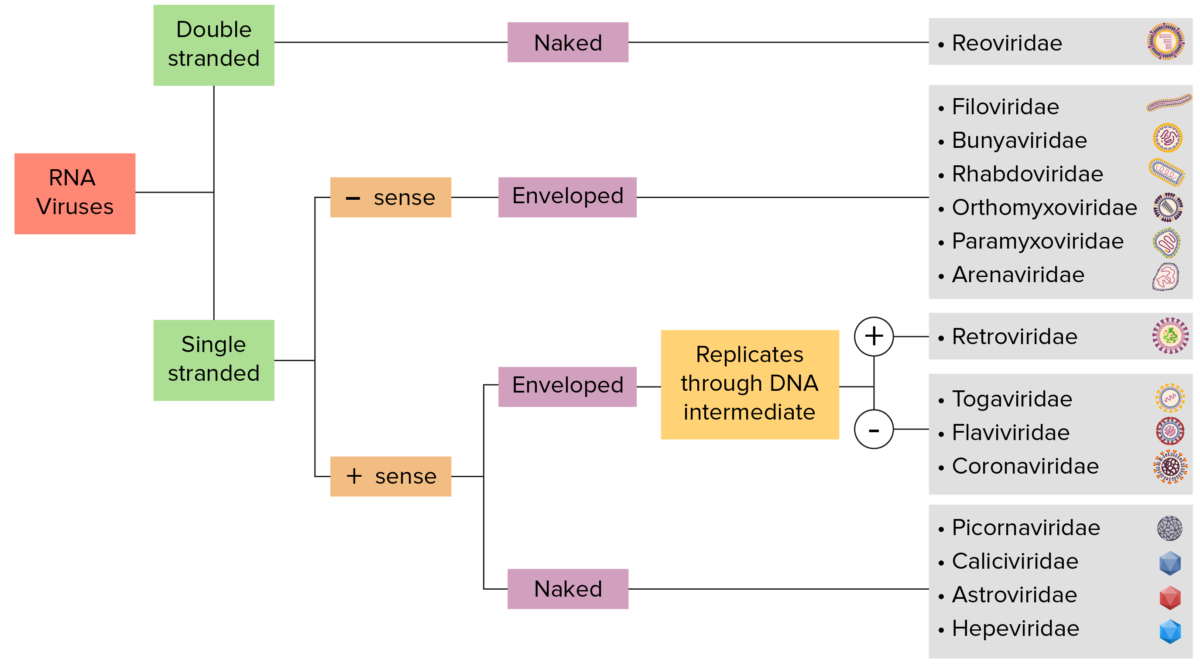
RNA virus identification:
Viruses can be classified in many ways. Most viruses, however, will have a genome formed by either DNA or RNA. RNA genome viruses can be further characterized by either a single- or double-stranded RNA. “Enveloped” viruses are covered by a thin coat of cell membrane (usually taken from the host cell). If the coat is absent, the viruses are called “naked” viruses. Viruses with single-stranded genomes are “positive-sense” viruses if the genome is directly employed as messenger RNA (mRNA), which is translated into proteins. “Negative-sense,” single-stranded viruses employ RNA dependent RNA polymerase, a viral enzyme, to transcribe their genome into messenger RNA.
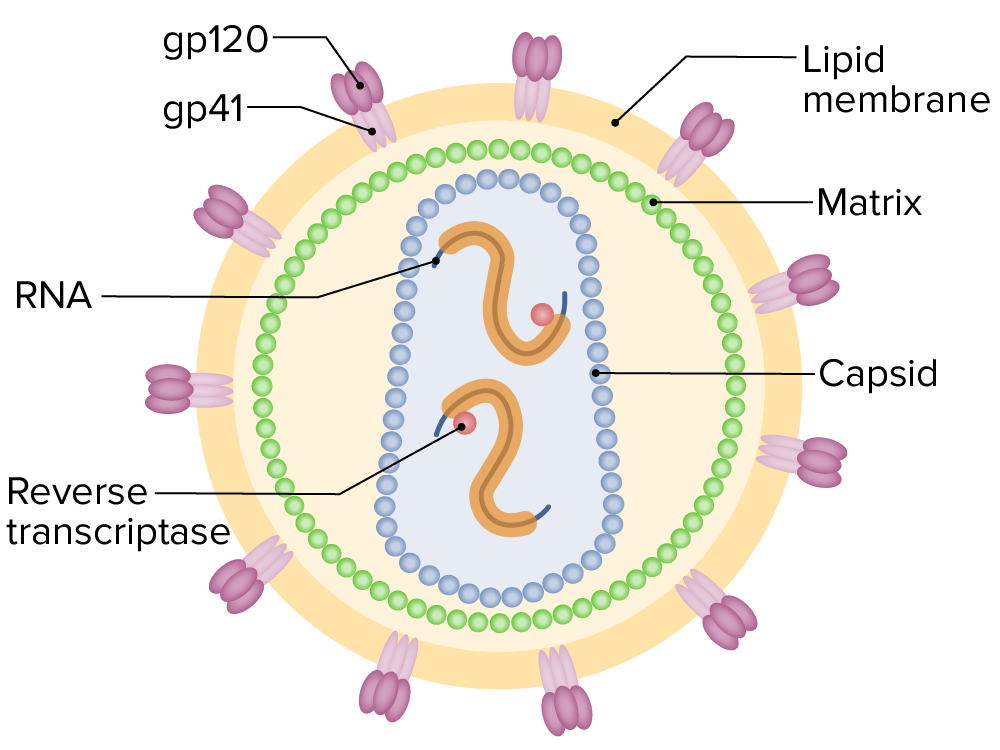
Diagram of the HIV type-1 virion featuring the genome structure, main enzymes, and glycoproteins (gp120 and gp41)
Image by Lecturio.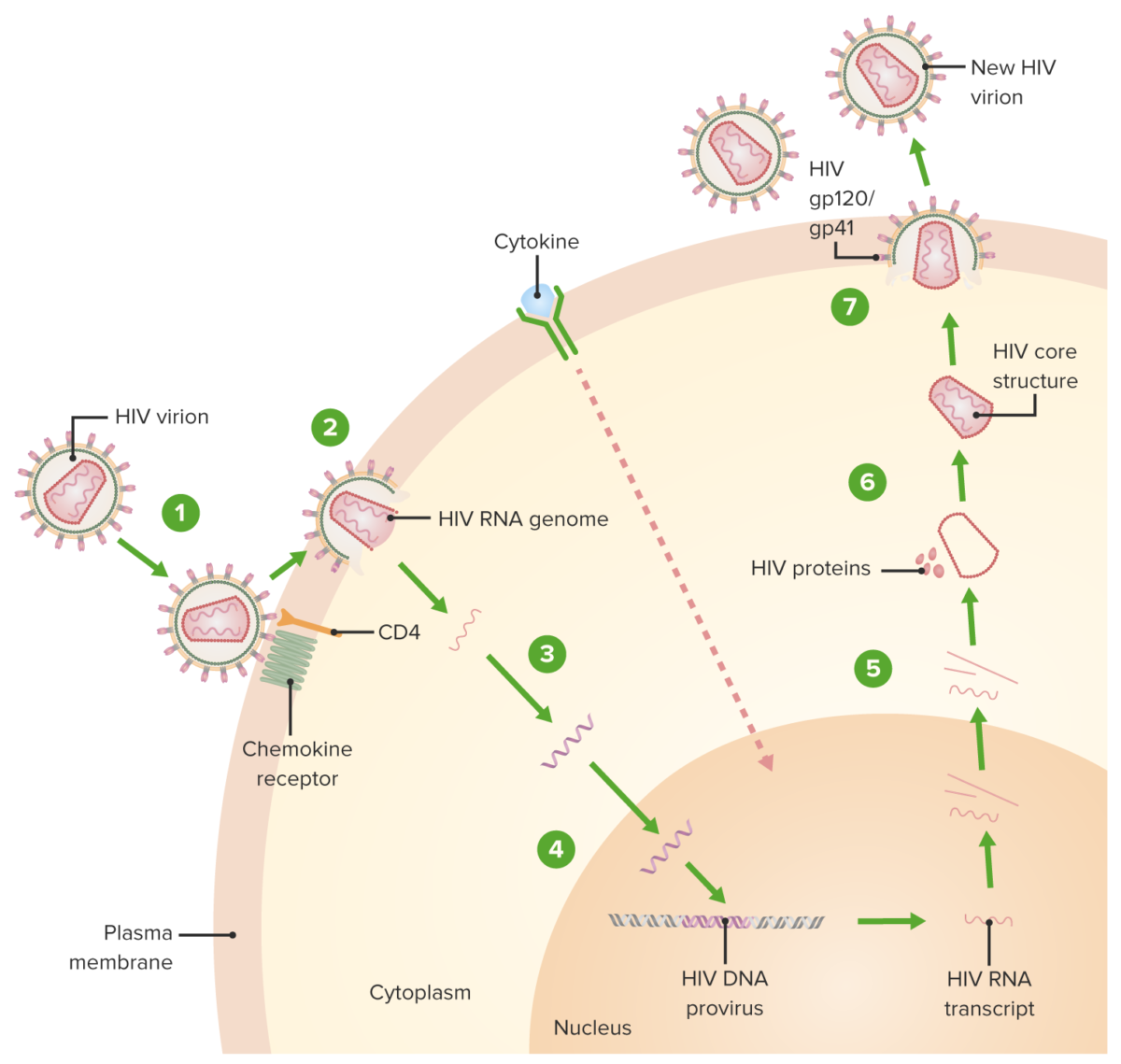
HIV replication cycle:
1. Virion binds the CD4 receptor and a chemokine receptor, followed by a conformational change that facilitates fusion of the virion and the host cell.
2. A capsid protein shell (surrounding the viral RNA and proteins) is uncoated as the virion traverses the cytoplasm.
3. Reverse transcriptase-mediated synthesis of proviral DNA occurs.
4. Viral DNA is transported across the nucleus and integrated into the host DNA, facilitated by integrase.
5. Viral DNA is transcribed, and multiple copies of new HIV RNA form and are transported to the cytoplasm. New HIV RNA becomes the genome of a new virus. Cytokine activation of the cell also occurs.
6. New viral RNA + proteins + enzymes move to the cell surface and form a noninfectious particle.
7. Particle (viral RNA + proteins) eventually buds out of the host cell with the immature HIV. Viral protein protease (enzyme) then cleaves newly synthesized polyproteins producing a mature HIV.
HIV particle released from an infected cell
Image: “HIV” by Bette Korber at Los Alamos National Laboratory. License: Public Domain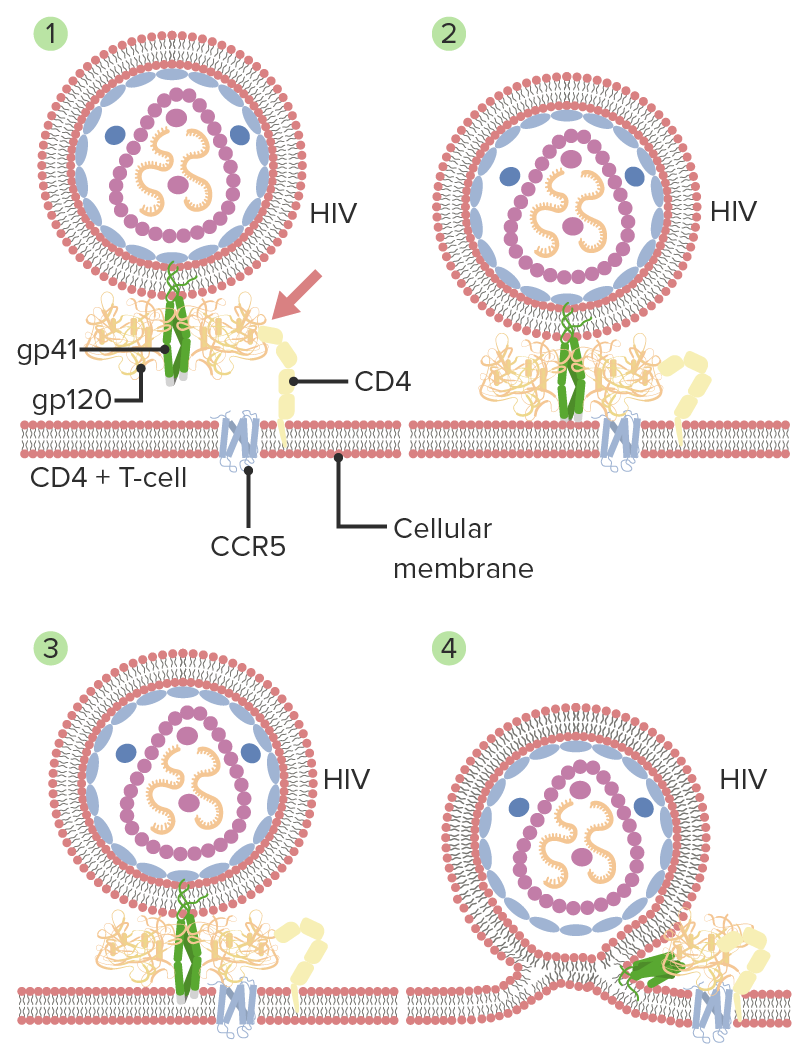
Mechanism of HIV entry and membrane fusion:
1. Initial interaction between gp120 and CD4
2. Conformational change in gp120 allows for secondary interaction with CCR5
3. Distal tips of gp41 are inserted into the cellular membrane.
4. gp41 undergoes significant conformational change. The process of folding in half and forming coiled coils pulls the viral and cellular membranes together, fusing them.