Human immunodeficiency Immunodeficiency Chédiak-Higashi Syndrome virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( HIV HIV Anti-HIV Drugs) infection is a sexually transmitted or blood-borne infection that destroys CD4 T cells CD4+ T cells A critical subpopulation of T-lymphocytes involved in the induction of most immunological functions. The HIV virus has selective tropism for the T4 cell which expresses the CD4 phenotypic marker, a receptor for HIV. In fact, the key element in the profound immunosuppression seen in HIV infection is the depletion of this subset of T-lymphocytes. T cells: Types and Functions. Chronic HIV HIV Anti-HIV Drugs infection and depletion of CD4 cells eventually results in acquired immunodeficiency Immunodeficiency Chédiak-Higashi Syndrome syndrome (AIDS), which can be diagnosed by the presence of certain opportunistic diseases called AIDS-defining conditions. These conditions include a wide spectrum of bacterial, viral, fungal, and parasitic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease as well as several malignancies and generalized conditions. These serious and life-threatening diseases are generally not seen in immunocompetent patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Treatment of HIV HIV Anti-HIV Drugs is very important in managing these diseases, and the incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency of AIDS-defining conditions has declined with the use of antiretroviral therapy Antiretroviral therapy Antiretroviral therapy (ART) targets the replication cycle of the human immunodeficiency virus (HIV) and is classified based on the viral enzyme or mechanism that is inhibited. The goal of therapy is to suppress viral replication to reach the outcome of undetected viral load. Anti-HIV Drugs.
Last updated: Jun 22, 2025
The tables below summarize the defining conditions of acquired immunodeficiency Immunodeficiency Chédiak-Higashi Syndrome syndrome (AIDS).
| AIDS-defining condition | CD4 count (cells/µL) | Clinical presentation | Management (in addition to HIV HIV Anti-HIV Drugs treatment) |
|---|---|---|---|
| Mycobacterium avium Mycobacterium avium A bacterium causing tuberculosis in domestic fowl and other birds. In pigs, it may cause localized and sometimes disseminated disease. The organism occurs occasionally in sheep and cattle. It should be distinguished from the m. avium complex, which infects primarily humans. Mycobacterium complex | < 50 |
|
Treatment: macrolide and ethambutol Ethambutol An antitubercular agent that inhibits the transfer of mycolic acids into the cell wall of the tubercle Bacillus. It may also inhibit the synthesis of spermidine in mycobacteria. The action is usually bactericidal, and the drug can penetrate human cell membranes to exert its lethal effect. Antimycobacterial Drugs |
| Mycobacterium tuberculosis Mycobacterium tuberculosis Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis complex bacteria. The bacteria usually attack the lungs but can also damage other parts of the body. Approximately 30% of people around the world are infected with this pathogen, with the majority harboring a latent infection. Tuberculosis spreads through the air when a person with active pulmonary infection coughs or sneezes. Tuberculosis | < 200 |
|
|
| Salmonella Salmonella Salmonellae are gram-negative bacilli of the family Enterobacteriaceae. Salmonellae are flagellated, non-lactose-fermenting, and hydrogen sulfide-producing microbes. Salmonella enterica, the most common disease-causing species in humans, is further classified based on serotype as typhoidal (S. typhi and paratyphi) and nontyphoidal (S. enteritidis and typhimurium). Salmonella septicemia | < 200 |
|
IV fluoroquinolones Fluoroquinolones Fluoroquinolones are a group of broad-spectrum, bactericidal antibiotics inhibiting bacterial DNA replication. Fluoroquinolones cover gram-negative, anaerobic, and atypical organisms, as well as some gram-positive and multidrug-resistant (MDR) organisms. Fluoroquinolones or 3rd-generation cephalosporins Cephalosporins Cephalosporins are a group of bactericidal beta-lactam antibiotics (similar to penicillins) that exert their effects by preventing bacteria from producing their cell walls, ultimately leading to cell death. Cephalosporins are categorized by generation and all drug names begin with “cef-” or “ceph-.” Cephalosporins |
| AIDS-defining condition | CD4 count (cells/µL) | Clinical presentation | Management (in addition to HIV HIV Anti-HIV Drugs treatment) |
|---|---|---|---|
| Cytomegalovirus Cytomegalovirus CMV is a ubiquitous double-stranded DNA virus belonging to the Herpesviridae family. CMV infections can be transmitted in bodily fluids, such as blood, saliva, urine, semen, and breast milk. The initial infection is usually asymptomatic in the immunocompetent host, or it can present with symptoms of mononucleosis. Cytomegalovirus (CMV) | < 50 |
|
Ganciclovir Ganciclovir An acyclovir analog that is a potent inhibitor of the herpesvirus family including cytomegalovirus. Ganciclovir is used to treat complications from aids-associated cytomegalovirus infections. Antivirals for Herpes Virus, valganciclovir, foscarnet Foscarnet An antiviral agent used in the treatment of cytomegalovirus retinitis. Foscarnet also shows activity against human herpesviruses and HIV. Antivirals for Herpes Virus, or cidofovir Cidofovir An acyclic nucleoside phosphonate that acts as a competitive inhibitor of viral DNA polymerases. It is used in the treatment of retinitis caused by cytomegalovirus infections and may also be useful for treating herpesvirus infections. Antivirals for Herpes Virus |
| Herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology | < 100 | Non-healing lesions, tracheitis, pneumonitis Pneumonitis Human Herpesvirus 6 and 7, esophagitis Esophagitis Esophagitis is the inflammation or irritation of the esophagus. The major types of esophagitis are medication-induced, infectious, eosinophilic, corrosive, and acid reflux. Patients typically present with odynophagia, dysphagia, and retrosternal chest pain. Esophagitis, keratitis Keratitis Inflammation of the cornea. Herpes Simplex Virus 1 and 2, meningoencephalitis Meningoencephalitis Encephalitis | Acyclovir Acyclovir A guanosine analog that acts as an antimetabolite. Viruses are especially susceptible. Used especially against herpes. Herpes Zoster (Shingles), valacyclovir Valacyclovir A prodrug of acyclovir that is used in the treatment of herpes zoster and herpes simplex virus infection of the skin and mucous membranes, including genital herpes. Herpes Zoster (Shingles), or famciclovir Famciclovir An aminopurine derivative and prodrug of penciclovir which is a competitive inhibitor of herpes simplex 2 DNA polymerase. It is used to treat herpes simplex virus infection. Antivirals for Herpes Virus |
| JC virus JC Virus JC virus (JCV) is a small, nonenveloped, single-stranded DNA virus belonging to the Polyomaviridae family, which are ubiquitous in the human population. While the primary infection is usually asymptomatic, the infection leads to lifelong latency in the kidneys and lymphoid organs. JC Virus and BK Virus (progressive multifocal Multifocal Retinoblastoma leukoencephalopathy) | < 200 | Focal-neurologic deficits, cognitive impairment | Supportive |
| AIDS-defining condition | CD4 count (cells/µL) | Clinical presentation | Management (in addition to HIV HIV Anti-HIV Drugs treatment) |
|---|---|---|---|
| Esophageal candidiasis Esophageal candidiasis Candida/Candidiasis | < 100 | Odynophagia Odynophagia Epiglottitis, oral thrush may be present | Fluconazole Fluconazole Triazole antifungal agent that is used to treat oropharyngeal candidiasis and cryptococcal meningitis in aids. Azoles |
| Pneumocystis jirovecii pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia | < 200 | Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, non-productive cough | Treatment and prophylaxis Prophylaxis Cephalosporins: TMP-SMX |
| Cryptococcal meningitis Cryptococcal meningitis Meningeal inflammation produced by cryptococcus neoformans, an encapsulated yeast that tends to infect individuals with acquired immunodeficiency syndrome and other immunocompromised states. The organism enters the body through the respiratory tract, but symptomatic infections are usually limited to the lungs and nervous system. The organism may also produce parenchymal brain lesions (torulomas). Clinically, the course is subacute and may feature headache; nausea; photophobia; focal neurologic deficits; seizures; cranial neuropathies; and hydrocephalus. Cryptococcus/Cryptococcosis | < 100 | Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, neck stiffness Neck Stiffness Meningitis, AMS AMS Neurologic syndrome with no physical findings occurring > 6 hours after ascent to altitudes > 2,500 m (rarely, 1,500 m) Altitude Sickness, neurologic deficits Neurologic Deficits High-Risk Headaches | Amphotericin B Amphotericin B Macrolide antifungal antibiotic produced by streptomyces nodosus obtained from soil of the orinoco river region of venezuela. Polyenes and flucytosine Flucytosine Flucytosine is a pyrimidine analog that disrupts fungal DNA and RNA synthesis. Flucytosine is always used in combination with other antifungal agents and is primarily used to treat cryptococcal meningitis. Flucytosine, Griseofulvin, and Terbinafine, followed by fluconazole Fluconazole Triazole antifungal agent that is used to treat oropharyngeal candidiasis and cryptococcal meningitis in aids. Azoles |
| CNS toxoplasmosis Toxoplasmosis Toxoplasmosis is an infectious disease caused by Toxoplasma gondii, an obligate intracellular protozoan parasite. Felines are the definitive host, but transmission to humans can occur through contact with cat feces or the consumption of contaminated foods. The clinical presentation and complications depend on the host’s immune status. Toxoplasma/Toxoplasmosis | < 100 | Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, AMS AMS Neurologic syndrome with no physical findings occurring > 6 hours after ascent to altitudes > 2,500 m (rarely, 1,500 m) Altitude Sickness, focal neurologic deficits Neurologic Deficits High-Risk Headaches, seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures |
|
| Coccidioidomycosis Coccidioidomycosis Coccidioidomycosis, commonly known as San Joaquin Valley fever, is a fungal disease caused by Coccidioides immitis or Coccidioides posadasii. When Coccidioides spores are inhaled, they transform into spherules that result in infection. Coccidioidomycosis is also a common cause of community-acquired pneumonia and can cause severe disease in the immunocompromised. Coccidioides/Coccidioidomycosis (disseminated, extrapulmonary) | < 250 | Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, night sweats Night sweats Tuberculosis, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, cough, lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy, weight loss Weight loss Decrease in existing body weight. Bariatric Surgery |
|
| Histoplasmosis Histoplasmosis Histoplasmosis is an infection caused by Histoplasma capsulatum, a dimorphic fungus. Transmission is through inhalation, and exposure to soils containing bird or bat droppings increases the risk of infection. Most infections are asymptomatic; however, immunocompromised individuals generally develop acute pulmonary infection, chronic infection, or even disseminated disease. Histoplasma/Histoplasmosis (disseminated, extrapulmonary) | < 150 | Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, night sweats Night sweats Tuberculosis, fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia, weight loss Weight loss Decrease in existing body weight. Bariatric Surgery, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, cough, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions | Amphotericin B Amphotericin B Macrolide antifungal antibiotic produced by streptomyces nodosus obtained from soil of the orinoco river region of venezuela. Polyenes or itraconazole Itraconazole A triazole antifungal agent that inhibits cytochrome p-450-dependent enzymes required for ergosterol synthesis. Azoles |
| Cryptosporidiosis | < 100 | Diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea, AIDS cholangiopathy | Nitazoxanide or paromomycin Paromomycin An aminoglycoside antibacterial and antiprotozoal agent produced by species of streptomyces. Amebicides |
| Cystoisosporiasis Cystoisosporiasis Cystoisospora is a genus within the Coccidia subclass of protozoans. They are single-celled, obligate intracellular parasites that cause intestinal infections in humans. Humans are the only host for these species, and they are both transmitted through the fecal-oral route. The symptoms of cystoisosporiasis are watery diarrhea, abdominal pain, and fever. Cystoisospora/Cystoisosporiasis and Cyclospora/Cyclosporiasis | < 50 | Watery, non-bloody diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea, anorexia Anorexia The lack or loss of appetite accompanied by an aversion to food and the inability to eat. It is the defining characteristic of the disorder anorexia nervosa. Anorexia Nervosa, abdominal pain Abdominal Pain Acute Abdomen, vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia | TMP-SMX |
| AIDS-defining condition | CD4 count (cells/μl) | Clinical presentation | Management (in addition to HIV HIV Anti-HIV Drugs treatment) |
|---|---|---|---|
| Lymphoma Lymphoma A general term for various neoplastic diseases of the lymphoid tissue. Imaging of the Mediastinum (Burkitt’s, DLBCL DLBCL Malignant lymphoma composed of large B lymphoid cells whose nuclear size can exceed normal macrophage nuclei, or more than twice the size of a normal lymphocyte. The pattern is predominantly diffuse. Most of these lymphomas represent the malignant counterpart of B-lymphocytes at midstage in the process of differentiation. Non-Hodgkin Lymphomas) | Burkitt’s: < 50; DLBCL DLBCL Malignant lymphoma composed of large B lymphoid cells whose nuclear size can exceed normal macrophage nuclei, or more than twice the size of a normal lymphocyte. The pattern is predominantly diffuse. Most of these lymphomas represent the malignant counterpart of B-lymphocytes at midstage in the process of differentiation. Non-Hodgkin Lymphomas: Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables | Constitutional symptoms Constitutional Symptoms Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis, extranodal mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast with rapid growth | Depends on the stage and includes chemotherapy Chemotherapy Osteosarcoma, immunotherapy, and radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy |
| CNS lymphoma Lymphoma A general term for various neoplastic diseases of the lymphoid tissue. Imaging of the Mediastinum | < 50 | Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, AMS AMS Neurologic syndrome with no physical findings occurring > 6 hours after ascent to altitudes > 2,500 m (rarely, 1,500 m) Altitude Sickness, focal neurological deficits Focal Neurological Deficits Brain Abscess, seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures, constitutional symptoms Constitutional Symptoms Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis | Chemotherapy Chemotherapy Osteosarcoma |
| Invasive cervical carcinoma | Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables | Watery, bloody vaginal discharge, pelvic pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways |
|
| Kaposi’s sarcoma | < 500 | Malignant vascular lesions of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, mucosa, GI, and respiratory tract |
|
| AIDS-defining condition | CD4 count (cells/μl) | Clinical presentation | Management (in addition to HIV HIV Anti-HIV Drugs treatment) |
|---|---|---|---|
| Wasting syndrome | Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables | Weight loss Weight loss Decrease in existing body weight. Bariatric Surgery of ≥ 10%, fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea | Nutritional care, treatment of secondary infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease |
| HIV-associated dementia Dementia Major neurocognitive disorders (NCD), also known as dementia, are a group of diseases characterized by decline in a person’s memory and executive function. These disorders are progressive and persistent diseases that are the leading cause of disability among elderly people worldwide. Major Neurocognitive Disorders | < 200 | Cognitive dysfunction, behavioral and mood changes, motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology symptoms | Optimize antiretroviral treatment. |
| HIV HIV Anti-HIV Drugs + | ≤ 200 | CD4 ≤ 200 is defined as AIDS per CDC | ART |

A patient with wasting syndrome due to AIDS
Image: “HIV Wasting Syndrome” by Department of Medicine, Ahmadu Bello University Teaching Hospital (ABUTH), Zaria, Nigeria. License: CC BY 3.0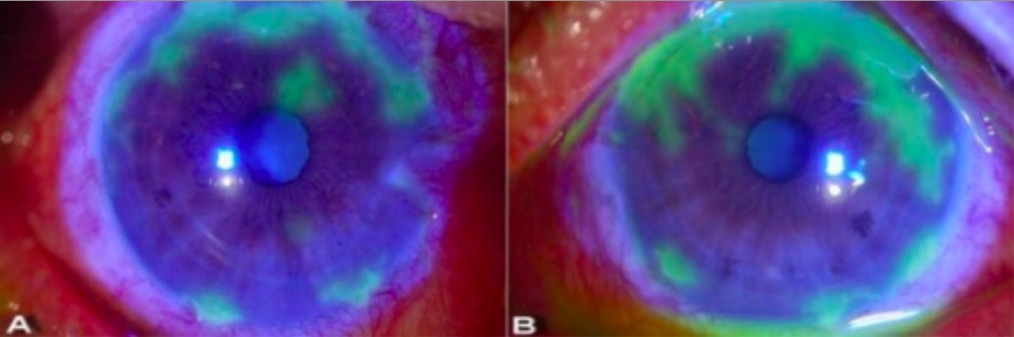
Slit lamp examination showing dendritic lesions in herpetic keratitis:
Seen here as
irregular geographic patterns of ulceration highlighted in green after the application of
yellow-orange fluorescein dye. The dye is taken up by damaged cornea (where the
surface has been disrupted) so the area appears green under cobalt blue light.
CMV retinitis CMV retinitis Infection of the retina by cytomegalovirus characterized by retinal necrosis, hemorrhage, vessel sheathing, and retinal edema. Cytomegalovirus retinitis is a major opportunistic infection in AIDS patients and can cause blindness. Retinal Detachment:
Toxoplasma Toxoplasma Toxoplasmosis is an infectious disease caused by Toxoplasma gondii, an obligate intracellular protozoan parasite. Felines are the definitive host, but transmission to humans can occur through contact with cat feces or the consumption of contaminated foods. The clinical presentation and complications depend on the host’s immune status. Toxoplasma/Toxoplasmosis chorioretinitis Chorioretinitis Chorioretinitis is the inflammation of the posterior segment of the eye, including the choroid and the retina. The condition is usually caused by infections, the most common of which is toxoplasmosis. Some of these infections can affect the fetus in utero and present as congenital abnormalities. Chorioretinitis:
Varicella zoster retinitis:
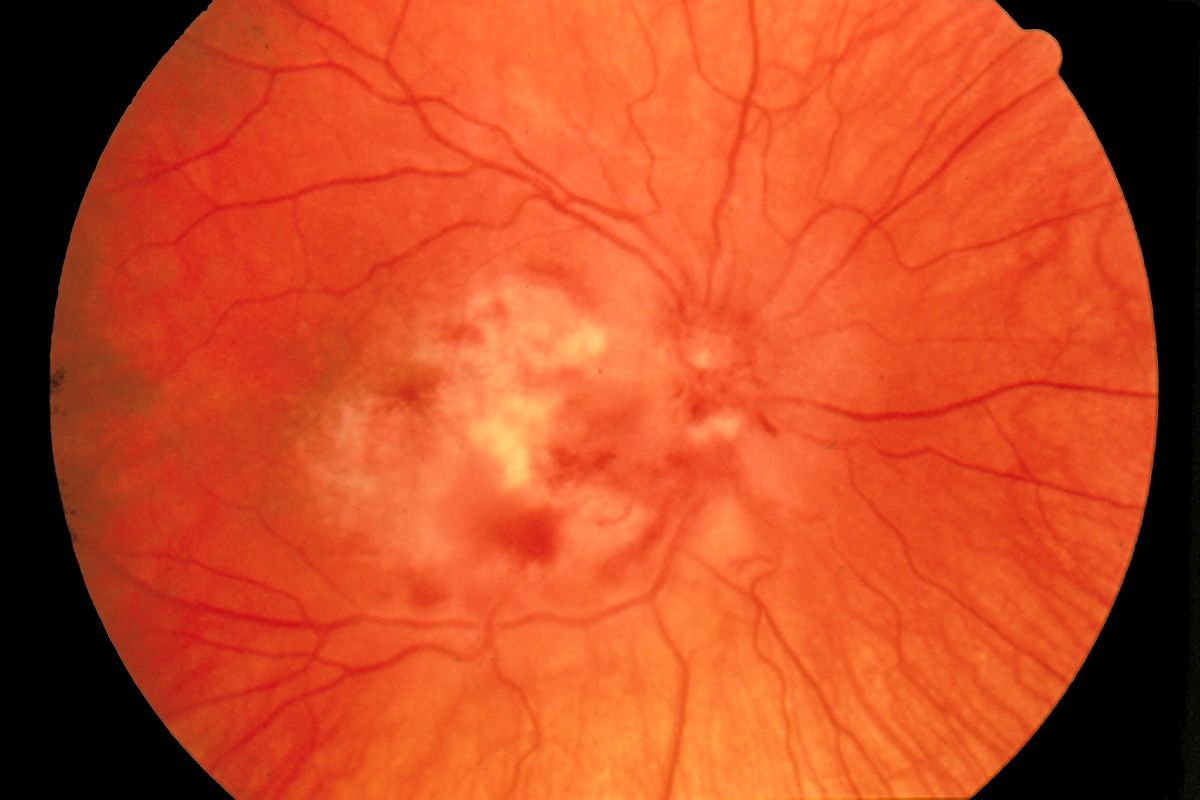
Fundoscopy of CMV retinitis
Image: “Fundus photograph-CMV retinitis” by National Eye Institute. License: Public Domain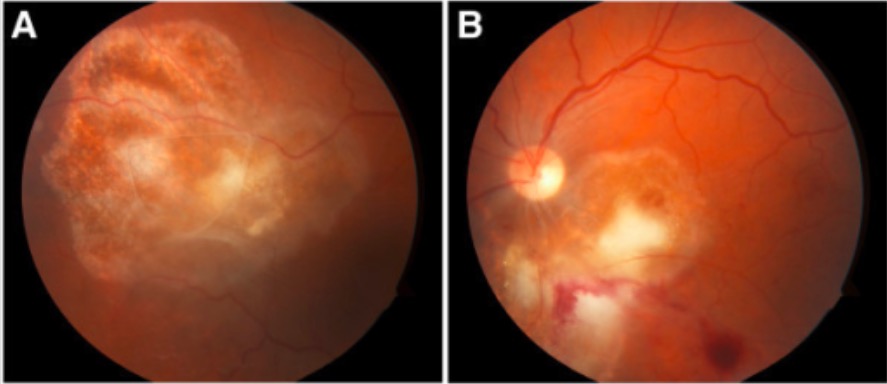
Fundoscopy of toxoplasma chorioretinitis
Note the yellow-white cotton lesions in both the right eye (A) and left eye (B).
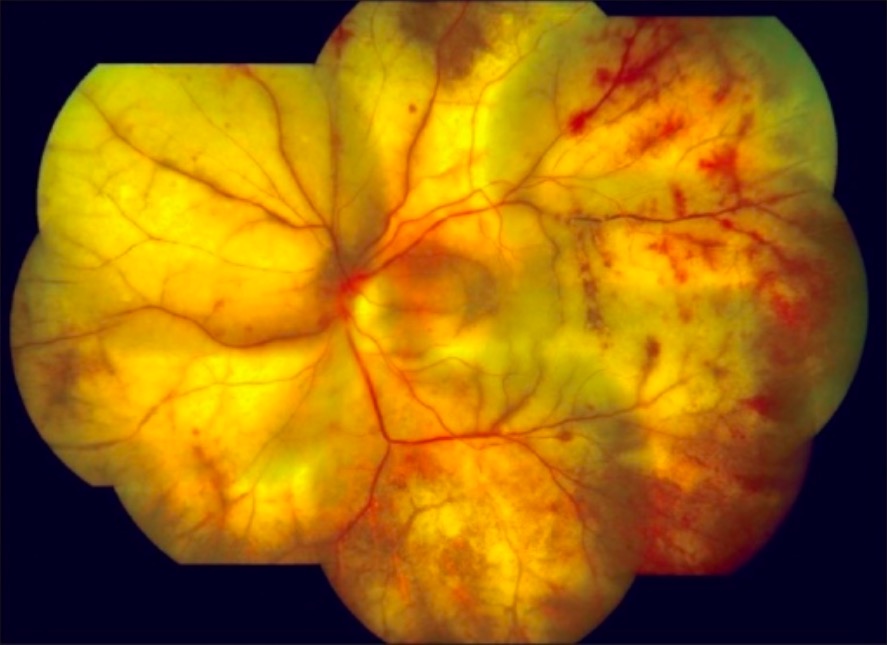
Fundoscopy of progressive retinal outer necrosis, a rare disease caused by varicella zoster
Image: “Cracked mud appearance” by Medical Research Foundation, Chennai, India. License: CC BY 2.0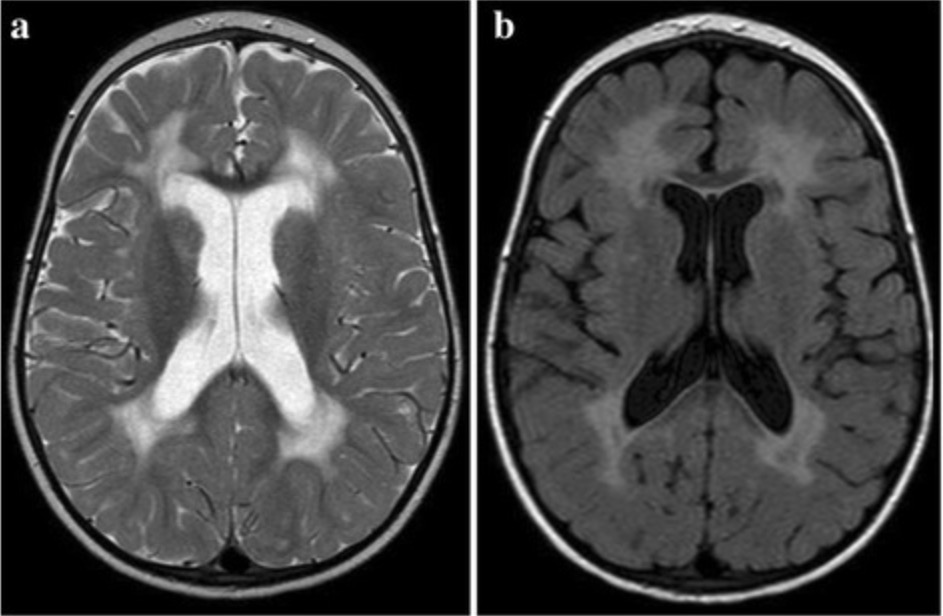
Magnetic resonance imaging in a patient with HIV-associated dementia
Axial T2 (a) and FLAIR (fluid-attenuated inversion recovery) (b) images showing bilateral symmetrical hyperintensity in the periventricular white matter
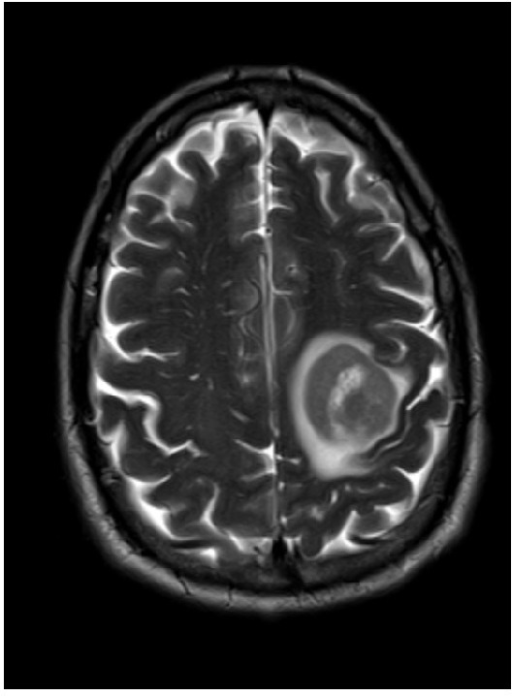
Toxoplasmosis and AIDS
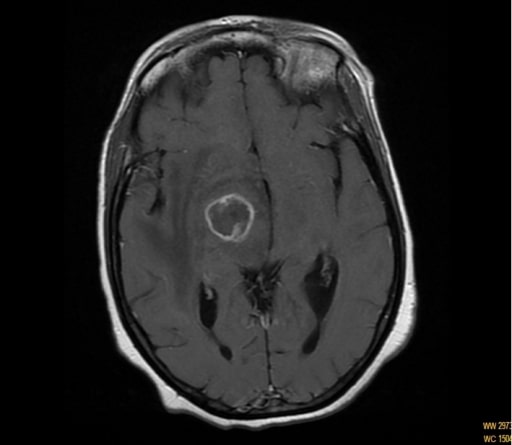
MRI showing ring enhancing of the capsule-thalamic lesion in a patient with hemichorea-hemiballismus
Magnetic resonance imaging of a patient with primary CNS lymphoma
Image shows a single ring-enhancing mass in the left hemisphere.
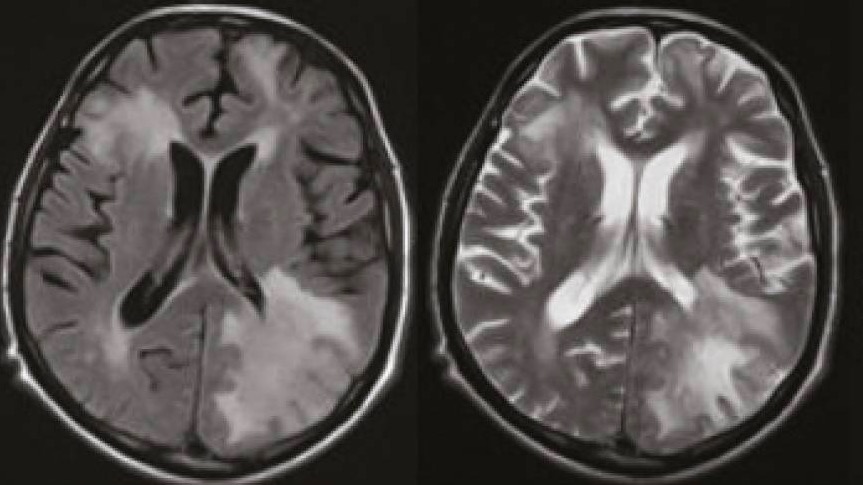
Magnetic reonance imaging in a patient with PML
Axial FLAIR (left) and axial T2-weighted images (right) show extensive diffuse lesions in the subcortical and periventricular white matter.
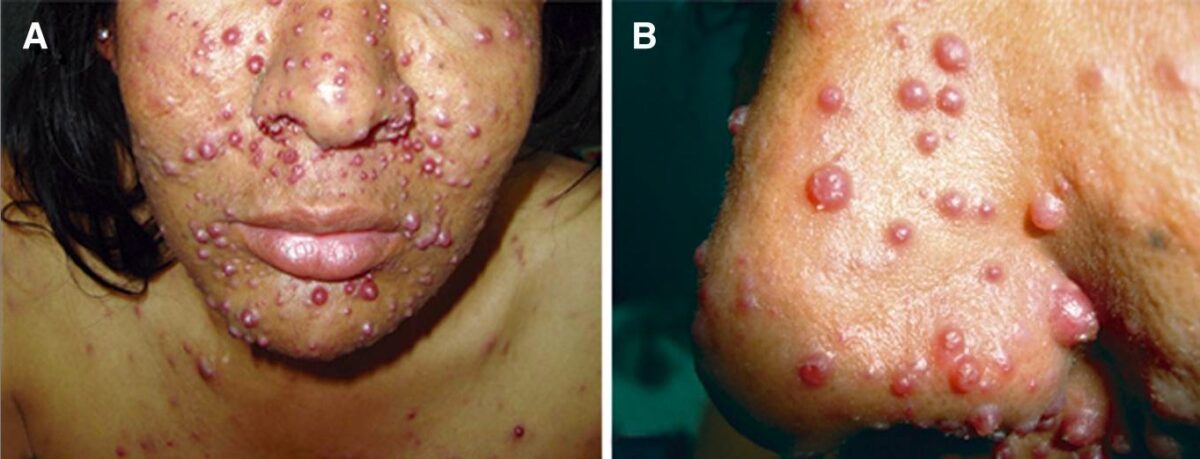
Nodular lesions due to bacillary angiomatosis in a patient with AIDS
Image: “Bacillary angiomatosis” by Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Lima, Peru. License: CC BY 4.0, edited by Lecturio.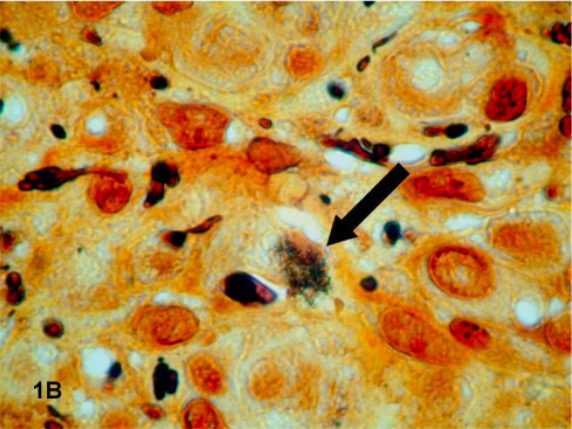
Histopathology specimen from a patient with bacillary angiomatosis
A dark-staining cluster of B. quintana (indicated by an arrow) is revealed with Warthin-Starry staining of a tissue specimen.

Cutaneous lesions on the nose of a patient with Kaposi’s sarcoma
Image: “Kaposi’s sarcoma” by M. Sand et al. License: CC BY 2.0
Cutaneous lesions of Kaposi’s sarcoma
Image: “Kaposi’s sarcoma” by OpenStax College. License: CC BY 3.0
Kaposi’s sarcoma presenting as violaceous papules in an HIV-positive patient’s mouth
Image: “Intraoral Kaposi’s sarcoma” by National Cancer Institute. License: Public DomainBiopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma confirms the diagnosis.
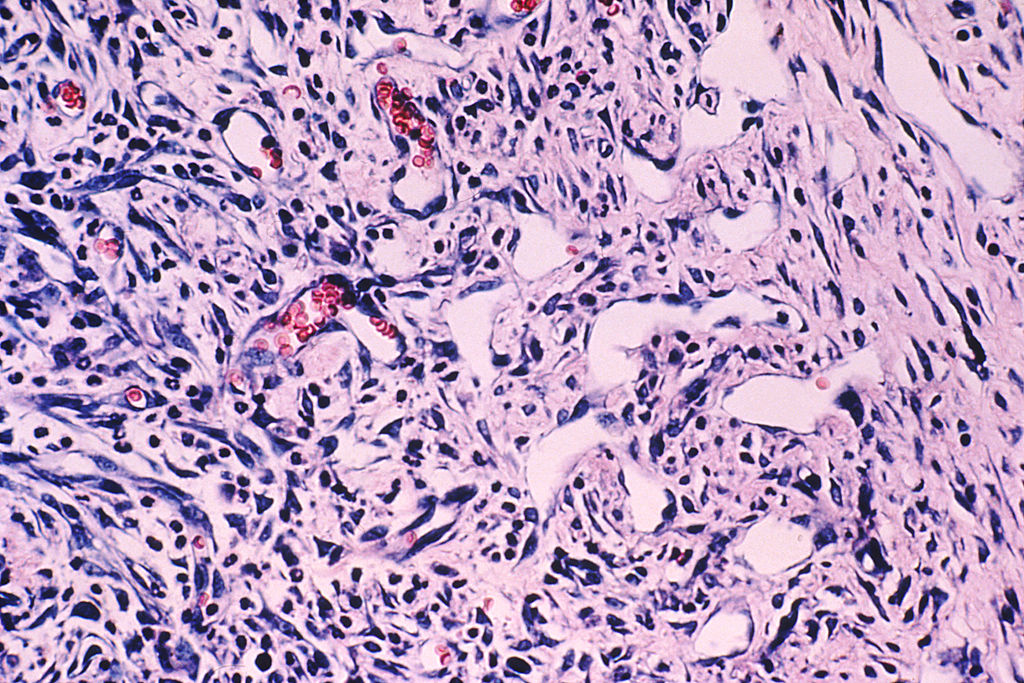
Histologic findings of angiogenesis in Kaposi’s sarcoma
Biopsy showing new blood vessel formation (appear as open spaces) where there are dividing epithelial cells and some red blood cells
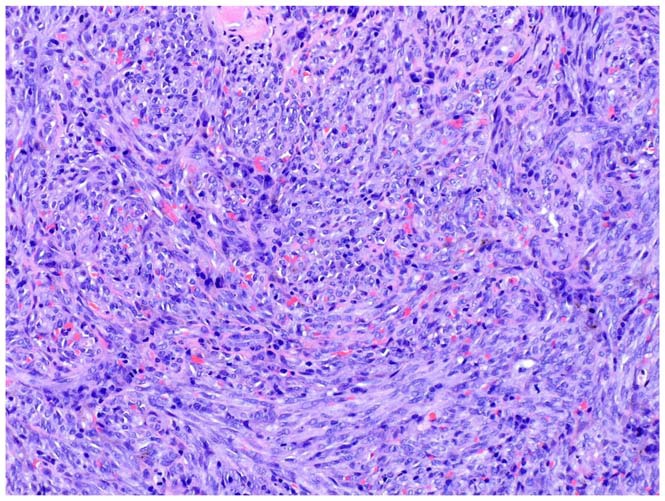
Biopsy image of Kaposi’s sarcoma
Spindle cells are seen, and red blood cells are visualized within poorly defined slit-like vascular spaces.