Uveitis is the inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the uvea Uvea The pigmented vascular coat of the eyeball, consisting of the choroid; ciliary body; and iris, which are continuous with each other. Eye: Anatomy, the pigmented middle layer of the eye, which comprises the iris, ciliary body Ciliary body A ring of tissue extending from the scleral spur to the ora serrata of the retina. It consists of the uveal portion and the epithelial portion. The ciliary muscle is in the uveal portion and the ciliary processes are in the epithelial portion. Eye: Anatomy, and choroid Choroid The thin, highly vascular membrane covering most of the posterior of the eye between the retina and sclera. Eye: Anatomy. The condition is categorized based on the site of disease; anterior uveitis is the most common. Uveitis can be caused by an infection or systemic disease, but in some cases the cause is idiopathic Idiopathic Dermatomyositis. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with blurred vision Blurred Vision Retinal Detachment, eye redness Redness Inflammation, and pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways (frequently in anterior uveitis) or reduced vision Vision Ophthalmic Exam and floaters Floaters Chorioretinitis (in intermediate and posterior uveitis). Diagnosis is by dilated funduscopy and slit-lamp examination Slit-Lamp Examination Blepharitis. Treatment for anterior uveitis is topical steroids Steroids A group of polycyclic compounds closely related biochemically to terpenes. They include cholesterol, numerous hormones, precursors of certain vitamins, bile acids, alcohols (sterols), and certain natural drugs and poisons. Steroids have a common nucleus, a fused, reduced 17-carbon atom ring system, cyclopentanoperhydrophenanthrene. Most steroids also have two methyl groups and an aliphatic side-chain attached to the nucleus. Benign Liver Tumors, while uveitis in deeper locations requires an injection. Uveitis from infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease and systemic disorders requires etiology-directed therapy.
Last updated: May 17, 2024
Uveitis is an inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the uvea Uvea The pigmented vascular coat of the eyeball, consisting of the choroid; ciliary body; and iris, which are continuous with each other. Eye: Anatomy, the middle layer of the eye, which comprises the iris, ciliary body Ciliary body A ring of tissue extending from the scleral spur to the ora serrata of the retina. It consists of the uveal portion and the epithelial portion. The ciliary muscle is in the uveal portion and the ciliary processes are in the epithelial portion. Eye: Anatomy, and the choroid Choroid The thin, highly vascular membrane covering most of the posterior of the eye between the retina and sclera. Eye: Anatomy.
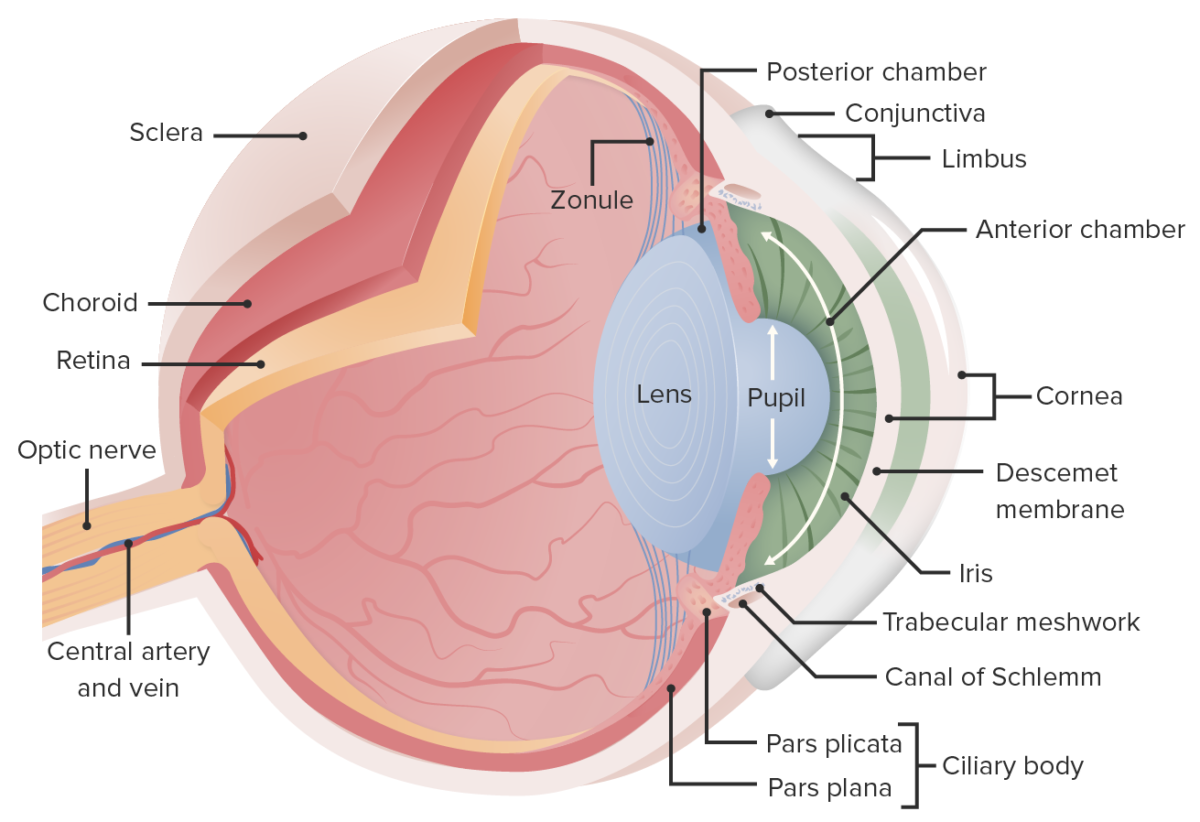
This image displays the essential anatomy of the eye. In cataracts, there is clouding of the lens, which opacifies the light as it projects to the retina; this leads to reduced vision, particularly at night when light levels are low.
Image by Lecturio.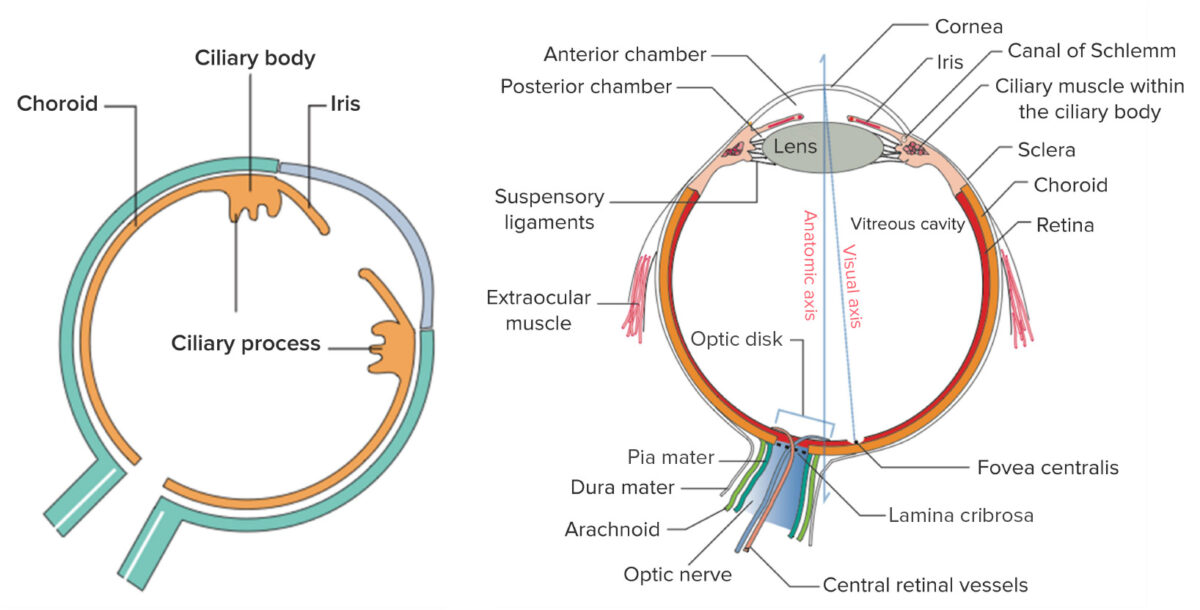
Left: the components of the uvea, the middle vascular layer of the eye
Right: general structure of the eye
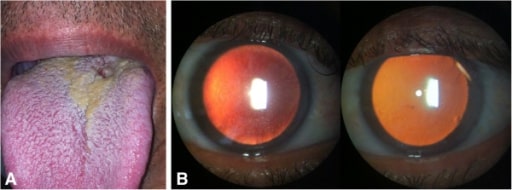
Bilateral nongranulomatous anterior uveitis associated with syphilis. (A): Lesion consistent with syphilitic chancre on base of the tongue; (B): Slit-lamp examination: small keratic precipitates (right) and fibrin deposits overlying corneal endothelium (left) in retroillumination
Image: “initial presentation of syphilis” by Hospital de Olhos Santa Luzia, Estrada do Encanamento 909, CEP 52070-000, Recife-Pernambuco, Brazil. License: CC BY 2.0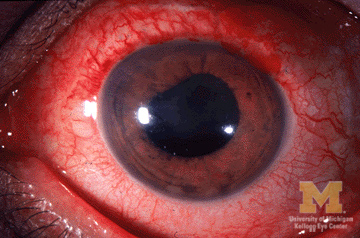
Image showing eye redness and irregular pupil from anterior uveitis
Image: “Anterior-uveitis” by Jonathan Trobe, M.D. License: CC BY 3.0Diagnosis is made by dilated fundus examination Dilated Fundus Examination Chorioretinitis and slit-lamp examination Slit-Lamp Examination Blepharitis. Scleral depression is an additional maneuver to visualize structures posterior to the lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy.
Findings
Additional laboratory and radiographic imaging are indicated when extraocular signs and symptoms are attributable to a causative disease (e.g., sarcoidosis Sarcoidosis Sarcoidosis is a multisystem inflammatory disease that causes noncaseating granulomas. The exact etiology is unknown. Sarcoidosis usually affects the lungs and thoracic lymph nodes, but it can also affect almost every system in the body, including the skin, heart, and eyes, most commonly. Sarcoidosis, syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis).
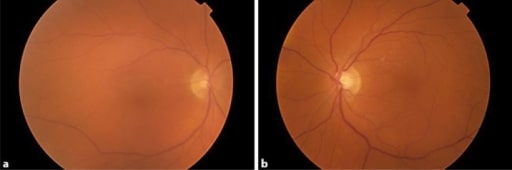
Fundus photographs demonstrating vitreous haze in both eyes. Patient was treated with dabrafenib and trametinib and developed bilateral uveitis.
Image: “Uveitis as a Result of MAP Kinase Pathway Inhibition” by Royal Surrey County Hospital NHS Foundation Trust, Guildford, Surrey, London, UK. License: CC BY 3.0
A 27-year-old pregnant woman with Behçet’s disease panuveitis with ciliary flush and a hypopyon (layering of white cells at the lower part of the anterior chamber)
Image: “Behçet’s Uveitis” by Department of Ophthalmology, Istanbul University, Istanbul Faculty of Medicine, Istanbul, Turkey. License: CC BY 2.0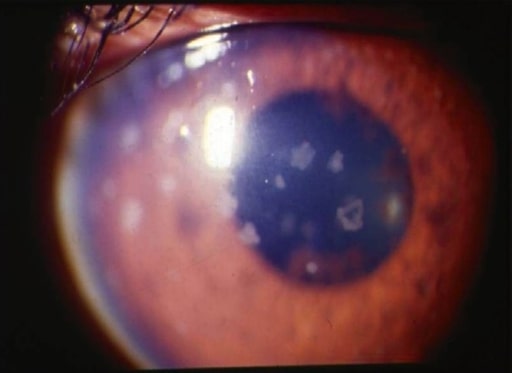
Anterior uveitis: slit-lamp photograph showing large, old keratic precipitates
Image: “anterior uveitis” by L. V. Prasad Eye Institute, Kallam Anji Reddy Campus, Hyderabad, India. License: CC BY 2.0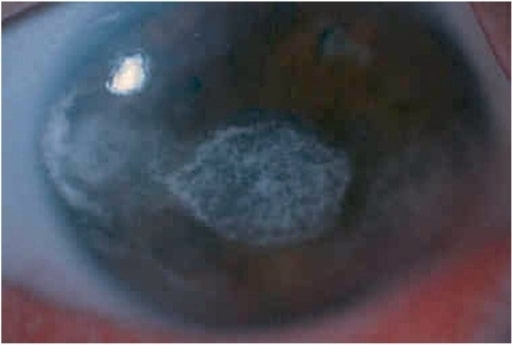
Diffuse illumination at the slit lamp shows severe band keratopathy in the left eye of a boy with anterior uveitis (associated with juvenile idiopathic arthritis).
Image: “keratopathy” by Department of Ophthalmology, Faculty of Medicine, Istanbul University, Istanbul, Turkey. License: CC BY 2.5