Glaucoma is an optic neuropathy Neuropathy Leprosy characterized by typical visual field Visual Field The Visual Pathway and Related Disorders defects and optic nerve Optic nerve The 2nd cranial nerve which conveys visual information from the retina to the brain. The nerve carries the axons of the retinal ganglion cells which sort at the optic chiasm and continue via the optic tracts to the brain. The largest projection is to the lateral geniculate nuclei; other targets include the superior colliculi and the suprachiasmatic nuclei. Though known as the second cranial nerve, it is considered part of the central nervous system. The 12 Cranial Nerves: Overview and Functions atrophy Atrophy Decrease in the size of a cell, tissue, organ, or multiple organs, associated with a variety of pathological conditions such as abnormal cellular changes, ischemia, malnutrition, or hormonal changes. Cellular Adaptation seen as optic disc Optic disc The portion of the optic nerve seen in the fundus with the ophthalmoscope. It is formed by the meeting of all the retinal ganglion cell axons as they enter the optic nerve. Eye: Anatomy cupping on examination. The acute form of glaucoma is a medical emergency. Glaucoma is often, but not always, caused by increased intraocular pressure Intraocular Pressure The pressure of the fluids in the eye. Ophthalmic Exam (IOP). Frequently, there is peripheral vision Vision Ophthalmic Exam loss that eventually leads to loss of central vision Vision Ophthalmic Exam. The 2 main types of glaucoma are open-angle and angle-closure. Overproduction or reduced excretion of the aqueous humor Humor Defense Mechanisms leads to open-angle glaucoma. Onset of symptoms is gradual. Angle-closure glaucoma results from blockage in the angle (of the iris and cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy), preventing drainage of the aqueous fluid. Diagnosis involves IOP determination (tonometry) and angle visualization with slit lamp Slit Lamp A microscope with a light source that can be projected into a linear beam. It allows cross-sectional viewing of the aqueous humor; conjuncteiva; cornea; eyelids; iris; and lens of the eye. Ophthalmic Exam (gonioscopy). Treatment includes topical medications that reduce IOP, and eye surgery.
Last updated: May 17, 2024
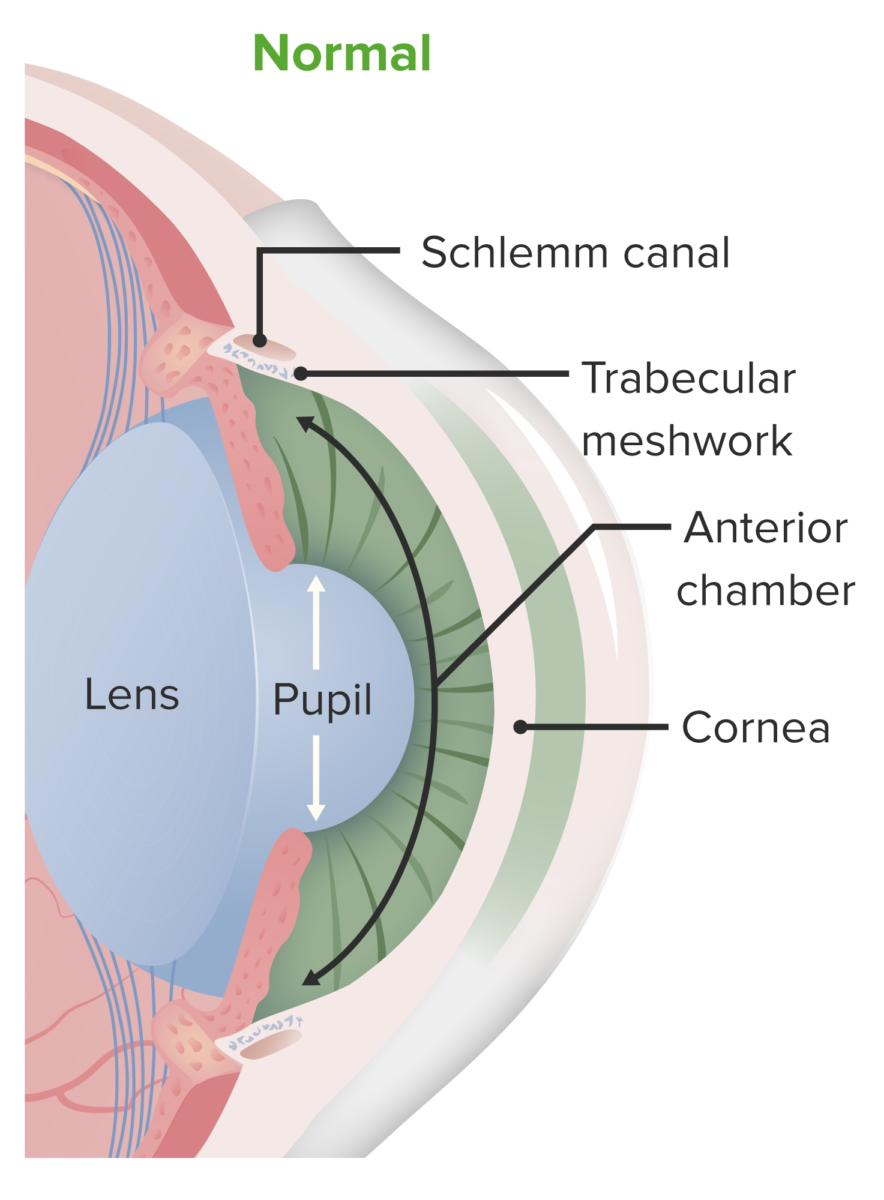
Anatomy of the anterior chamber. Aqueous humor is produced in the posterior chamber but travels to the anterior chamber (passing through the pupil). It is drained from the anterior chamber via the trabecular meshwork and ultimately through the canal of Schlemm.
Image by Lecturio.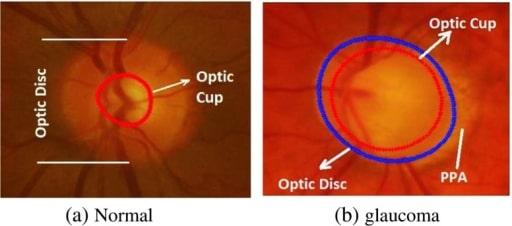
This image shows the fundoscopic changes that occur in glaucoma. Note the normal fundoscopic exam on the left and the findings consistent with glaucoma on the right, with a large optic cup occupying most of the optic disc.
Image: “Comparison of the optic disc area of the a normal and b glaucomatous image” by Manchester Metropolitan University, School of Computing, Mathematics and Digital Technology, Manchester, M1 5GD, UK. License: Open Source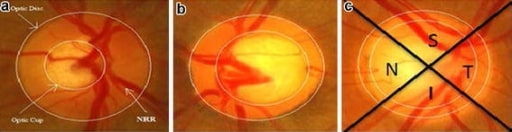
The progression of glaucoma: (a) shows a normal eye; (b) shows an eye with moderate glaucoma; and (c) demonstrates an eye with severe glaucoma. Note the continuously increasing optic cup-to-optic disc ratio.
Image: “a Normal eye; b eye with moderate glaucoma; c eye with severe glaucoma” by US National Library of Medicine. License: CC BY 4.0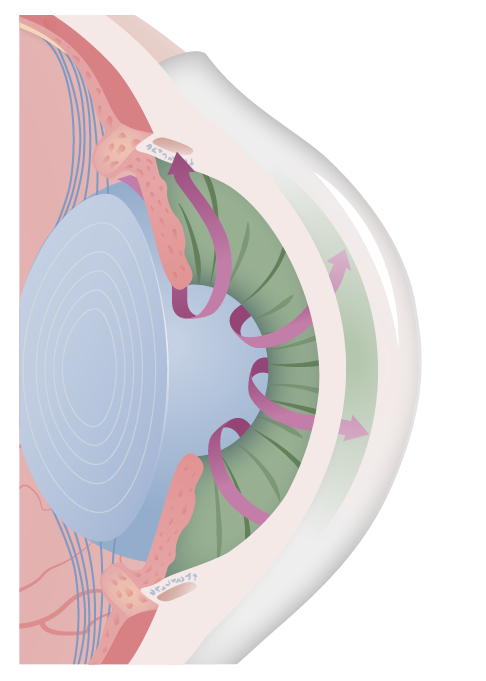
Illustration of the open-angle and free flow of aqueous humor in open-angle glaucoma. The most common cause is idiopathic and related to either increased production or decreased drainage.
Image by Lecturio.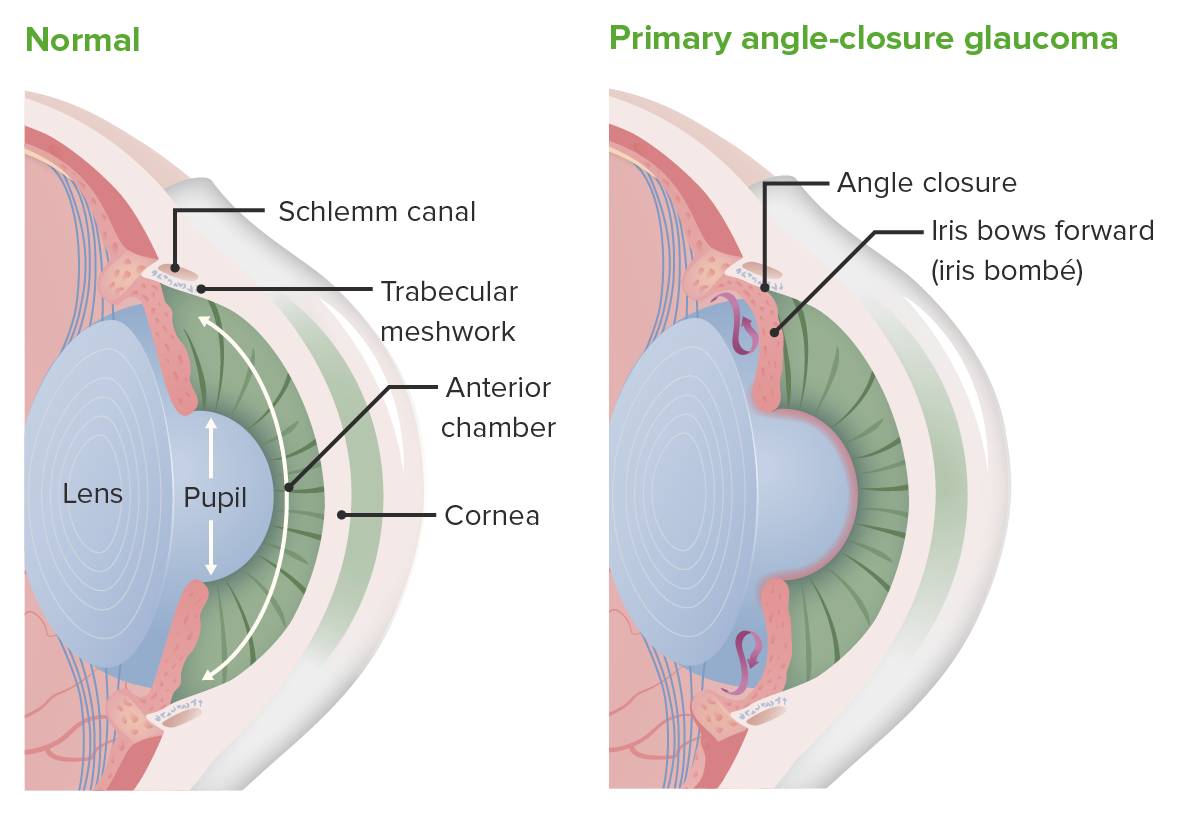
The changes that occur with closed-angle glaucoma. In the normal eye (left image), aqueous humor exits from the posterior chamber and enters the anterior chamber, where it can drain through the trabecular meshwork and the canal of Schlemm. In patients with closed-angle glaucoma (right image), that pathway is blocked, resulting in an accumulation of aqueous humor and increased intraocular pressure.
Image by Lecturio.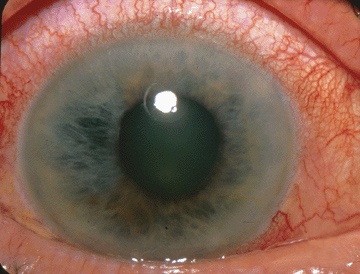
Photograph showing acute angle-closure glaucoma
Image: “The Eyes Have It” by Jonathan Trobe, M.D. License: CC BY 3.0The differential diagnoses of glaucoma include the following conditions: