The pupil is the space within the eye that permits light to project onto the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy. Anatomically located in front of the lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy, the pupil's size is controlled by the surrounding iris. The pupil provides insight Insight Psychiatric Assessment into the function of the central and autonomic nervous systems. The afferent Afferent Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology pathway for visual function starts from the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy and moves through the optic tracts and lateral geniculate nuclei, terminating in the visual cortex Visual cortex Area of the occipital lobe concerned with the processing of visual information relayed via visual pathways. Cerebral Cortex: Anatomy. Light stimulus is conducted by the parasympathetic system Parasympathetic system The craniosacral division of the autonomic nervous system. The cell bodies of the parasympathetic preganglionic fibers are in brain stem nuclei and in the sacral spinal cord. They synapse in cranial autonomic ganglia or in terminal ganglia near target organs. The parasympathetic nervous system generally acts to conserve resources and restore homeostasis, often with effects reciprocal to the sympathetic nervous system. Autonomic Nervous System: Anatomy to the midbrain Midbrain The middle of the three primitive cerebral vesicles of the embryonic brain. Without further subdivision, midbrain develops into a short, constricted portion connecting the pons and the diencephalon. Midbrain contains two major parts, the dorsal tectum mesencephali and the ventral tegmentum mesencephali, housing components of auditory, visual, and other sensorimotor systems. Brain Stem: Anatomy, while psychosensory reaction is processed by the sympathetic system Sympathetic system The thoracolumbar division of the autonomic nervous system. Sympathetic preganglionic fibers originate in neurons of the intermediolateral column of the spinal cord and project to the paravertebral and prevertebral ganglia, which in turn project to target organs. The sympathetic nervous system mediates the body's response to stressful situations, i.e., the fight or flight reactions. It often acts reciprocally to the parasympathetic system. Autonomic Nervous System: Anatomy. Efferent Efferent Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology pathways produce the appropriate response: miosis and mydriasis Mydriasis Dilation of pupils to greater than 6 mm combined with failure of the pupils to constrict when stimulated with light. This condition may occur due to injury of the pupillary fibers in the oculomotor nerve, in acute angle-closure glaucoma, and in adie syndrome. Glaucoma from the parasympathetic and sympathetic innervations, respectively. Pupillary disorders result from defects in areas of the visual afferent Afferent Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology and efferent Efferent Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology pathways. Presentation varies with pupillary size along with response to light and medication.
Last updated: May 17, 2024
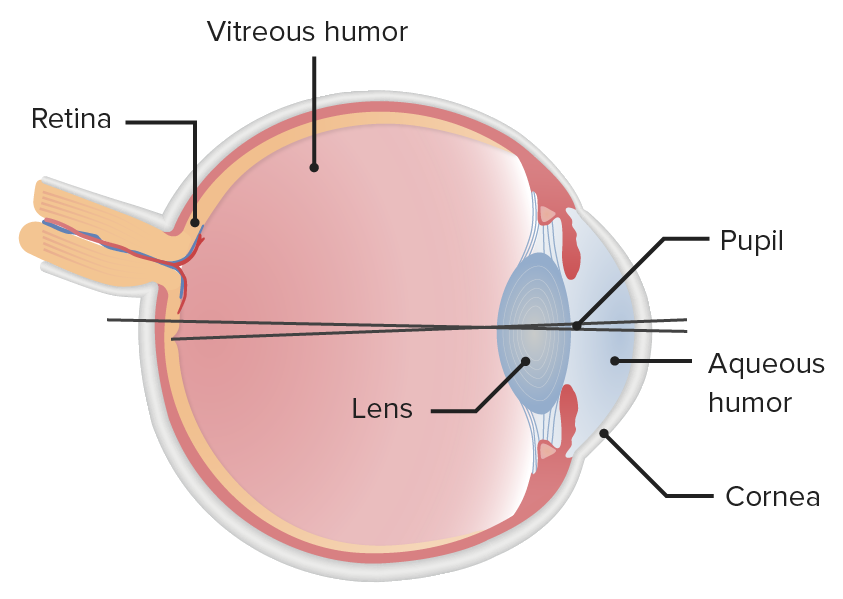
Illustration of the structure of the eyeball, highlighting the spatial location that defines the pupil
Image by Lecturio.From stimuli to the primary visual cortex Primary Visual Cortex The Visual Pathway and Related Disorders:
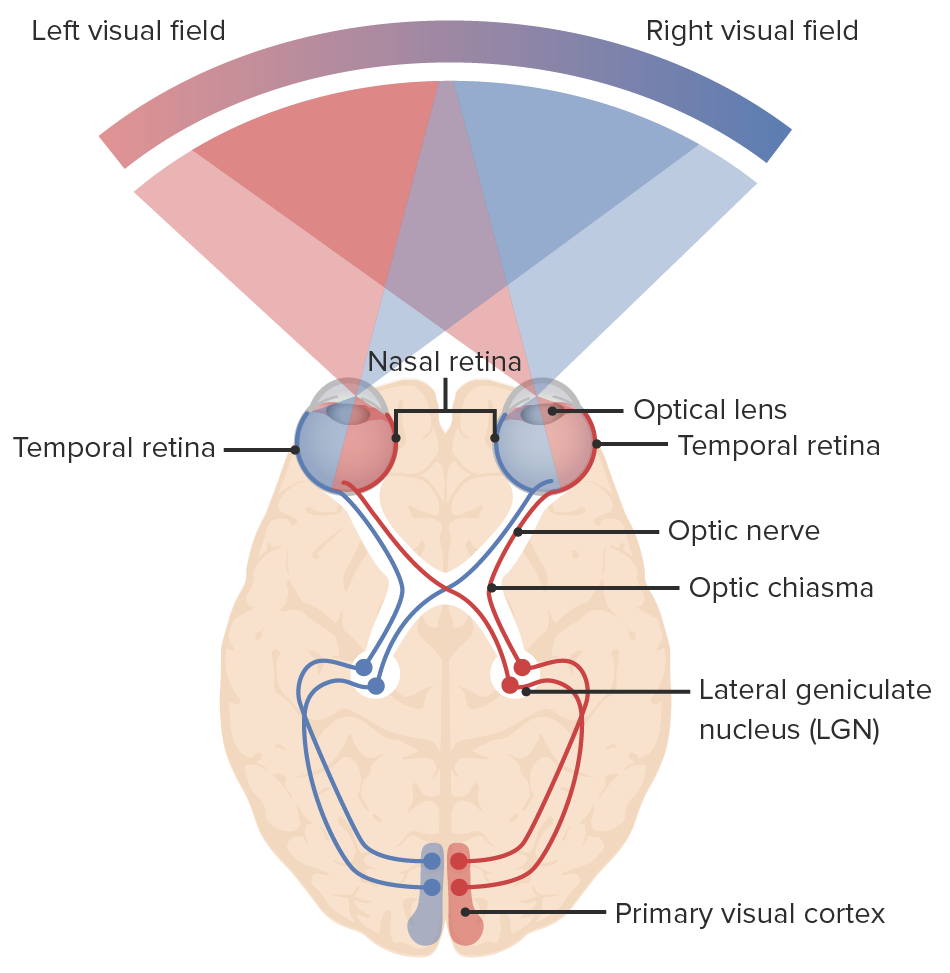
Diagram of the visual pathway and the visual fields: light enters the eye, sending signals to the retina and through the optic nerve. The nasal fibers of each eye decussate at the optic chiasm, continuing to the optic tract with the temporal fibers: right nasal fibers join the left temporal fibers (blue lines) and the left nasal fibers join the right temporal fibers (red lines). Neurons synapse at the lateral geniculate nucleus. Optic radiations connect the lateral geniculate nucleus to the primary visual cortex of the occipital lobe where visual information is processed.
Image by Lecturio.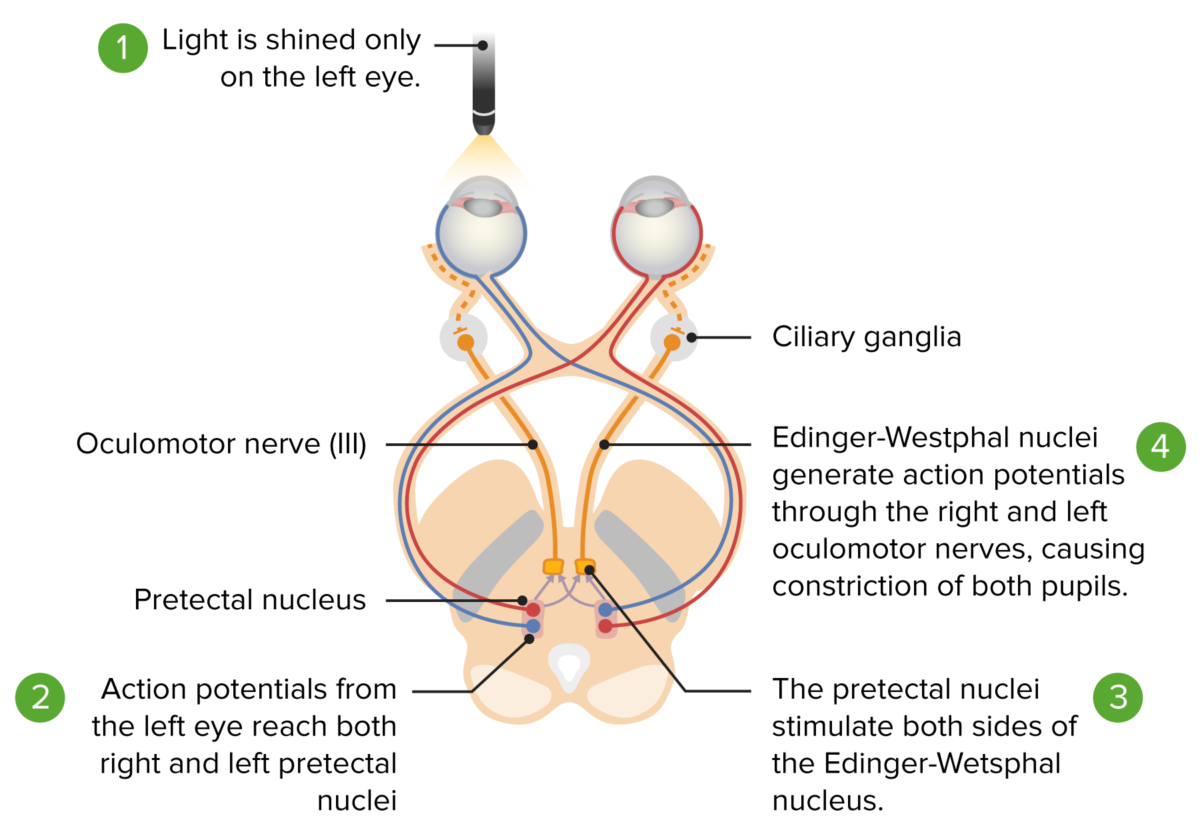
Pupillary light reflex pathway: from light stimulation of the retina to the midbrain. Afferent pathway (red and blue lines): Left light stimulus goes from the left retina to the optic chiasm to the optic tract, ending at the ipsilateral pretectal nucleus. The pretectal nucleus supplies both left and right Edinger-Westphal nuclei. Yellow lines show impulse from both nuclei reaching both ciliary ganglia and resulting in bilateral miosis.
Image by Lecturio.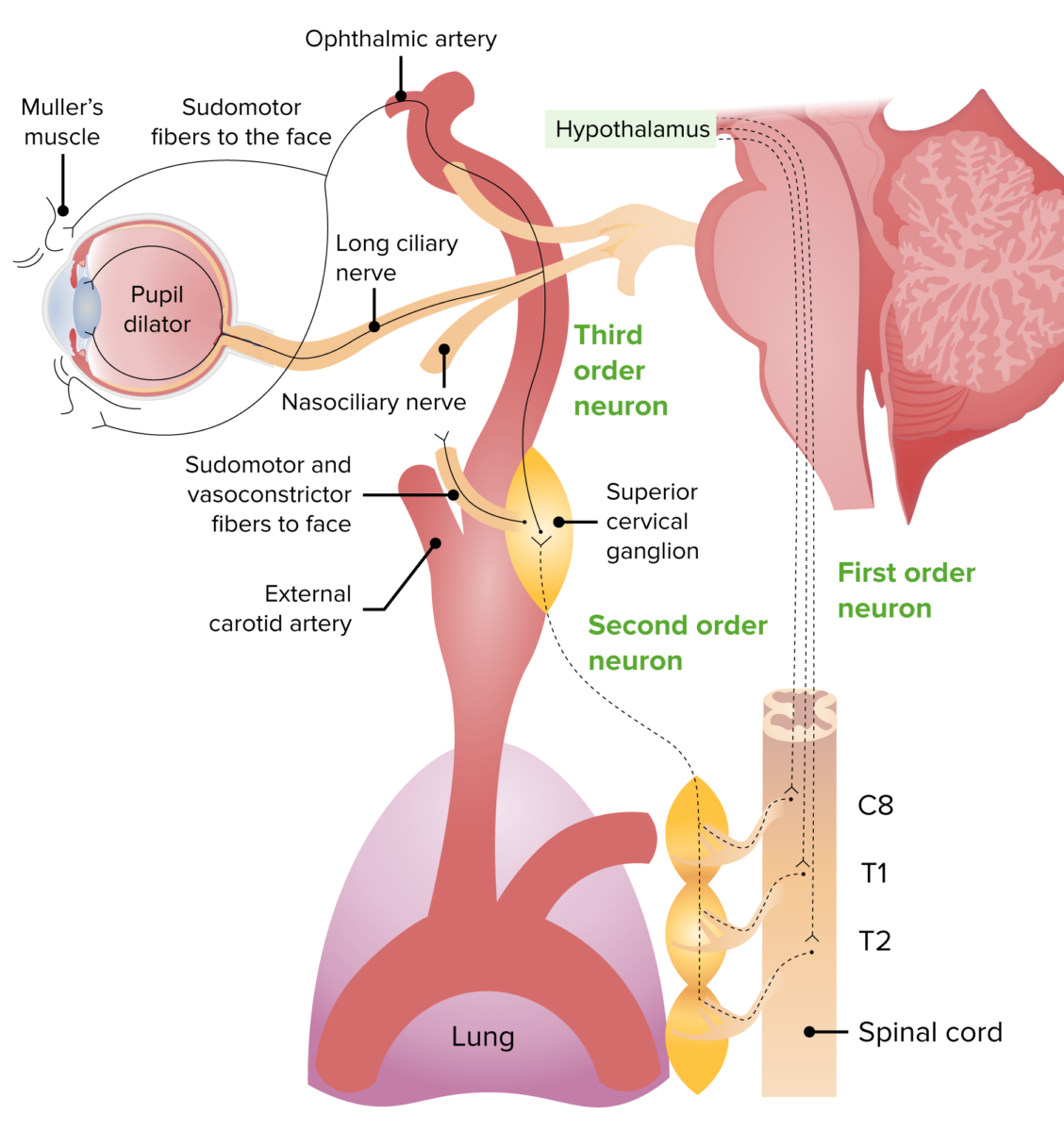
Image of the sympathetic innervation pathway:
1st-order neuron: starts from the hypothalamus to the center of Budge (spinal cord C8–T2)
2nd-order neuron: passes out of the spinal cord going superiorly to the superior cervical ganglion
3rd-order neuron: joins the trigeminal nerve and oculosympathetic fibers, synapses on the dilator pupillae and Müller’s muscle, causing mydriasis and eyelid opening.
Consists of 3 responses:

Illustration of the pupillary response to light: Bright light levels result in miosis and low light levels stimulate sympathetic activity, resulting in mydriasis.
Image by Lecturio.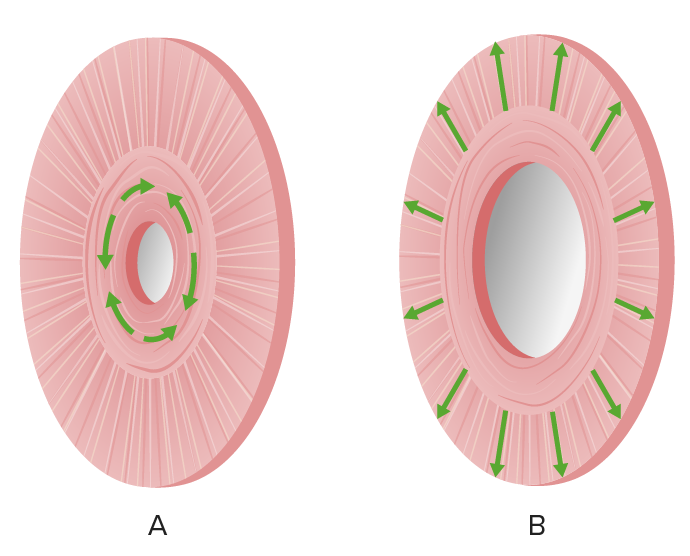
Illustration of the iris muscle actions:
(a) miosis by the sphincter pupillae;
(b) mydriasis by the dilator pupillae (radial muscles)

Anisocoria with right mydriasis
Image: “Evident right mydriasis” by U,O,C Pediatria Generale Dipartimento di Medicina Pediatrica, Ospedale Pediatrico Bambino Gesù, Piazza Sant’Onofrio 4, 00165 Roma, Italy. License: CC BY 2.0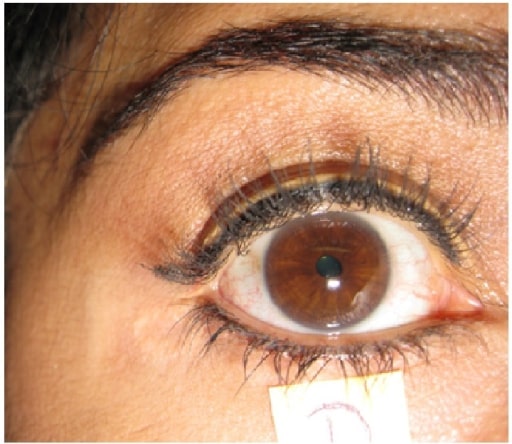
Tonic right pupil: unresponsive to light stimulation
Image: “Holmes-Adie’s Syndrome” by US National Library of Medicine. License: CC BY 4.0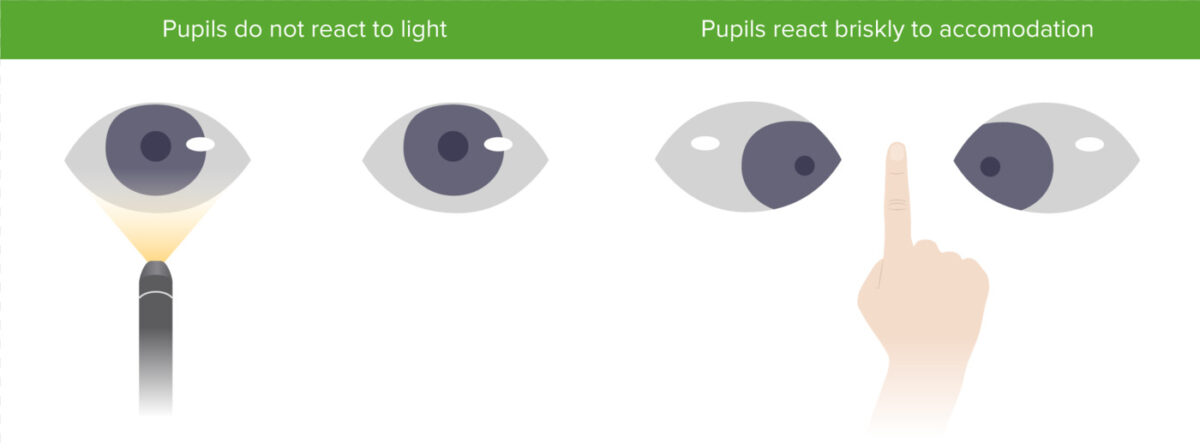
Argyll Robertson pupil with bilateral miosis that do not constrict to light, but do constrict to accommodation
Image by Lecturio.
Horner’s syndrome after superficial cervical plexus block placement (regional anesthesia for clavicular fracture). A: right ptosis; B: right miosis.
Image: “Horner’s syndrome” by Highland Hospital-Alameda Health System, Department of Emergency Medicine, Oakland, California. License: CC BY 4.0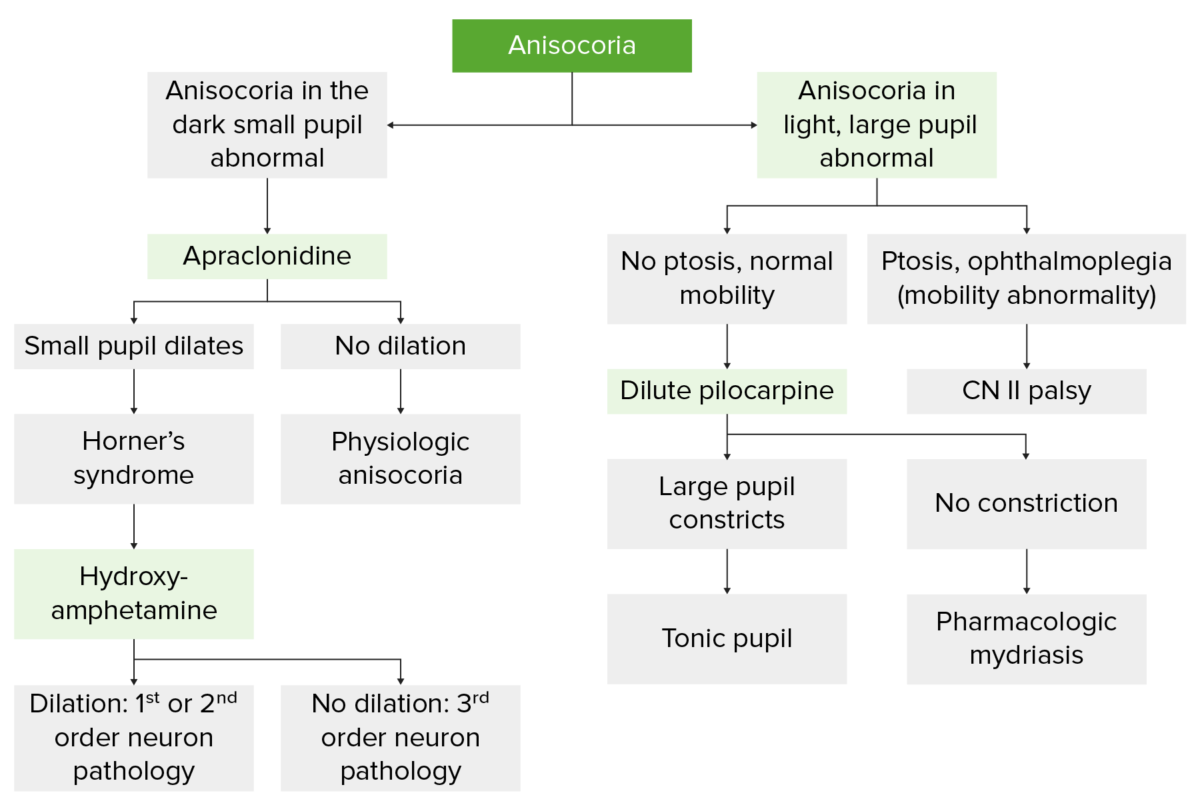
Flowchart illustrating the evaluation of anisocoria
Image by Lecturio.| Medication | Mydriasis Mydriasis Dilation of pupils to greater than 6 mm combined with failure of the pupils to constrict when stimulated with light. This condition may occur due to injury of the pupillary fibers in the oculomotor nerve, in acute angle-closure glaucoma, and in adie syndrome. Glaucoma | Miosis |
|---|---|---|
| Ophthalmic medications |
|
|
| Illicit drugs Illicit Drugs Drugs that are manufactured, obtained, or sold illegally. They include prescription drugs obtained or sold without prescription and non-prescription drugs. Illicit drugs are widely distributed, tend to be grossly impure and may cause unexpected toxicity. Delirium |
|
Heroin Heroin A narcotic analgesic that may be habit-forming. It is a controlled substance (opium derivative) listed in the U.S. Code of federal regulations, title 21 parts 329. 1, 1308. 11 (1987). Sale is forbidden in the United States by federal statute. Nephrotic Syndrome |
| Other medications |
|
Opioid
Opioid
Compounds with activity like opiate alkaloids, acting at opioid receptors. Properties include induction of analgesia or narcosis.
Constipation
|
| Herbal | Jimsonweed (with anticholinergic Anticholinergic Anticholinergic drugs block the effect of the neurotransmitter acetylcholine at the muscarinic receptors in the central and peripheral nervous systems. Anticholinergic agents inhibit the parasympathetic nervous system, resulting in effects on the smooth muscle in the respiratory tract, vascular system, urinary tract, GI tract, and pupils of the eyes. Anticholinergic Drugs properties) |