Blepharitis is an ocular condition characterized by eyelid inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation. Anterior blepharitis involves the eyelid skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and eyelashes, while the posterior type affects the meibomian glands. Often, these conditions overlap. The typical presentation of blepharitis includes eyelid edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema with itching and redness Redness Inflammation, crusts and scales Scales Dry or greasy masses of keratin that represent thickened stratum corneum. Secondary Skin Lesions around the eyelashes, and gritty sensation. Diagnosis is clinical, with a slit-lamp examination providing details of the structural changes affecting the eye. The mainstay of treatment is eyelid hygiene using warm compresses Warm Compresses Chalazion and eyelid scrubs. In moderate-to-severe cases, topical and oral antibiotics are utilized. Topical glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids also help improve symptoms but require an ophthalmology evaluation due to potential adverse effects.
Last updated: May 17, 2024

Erythematous, swollen eyelids from blepharitis
Image: “Blepharitis” by clubtable. License: Public Domain
Herpetic blepharitis: swelling and erythema of the eyelids. Erosions and ulcerations of the lid margins can be seen.
Image: “Herpetic blepharitis” by 3501 Champion Lake Boulevard, #1609, Shreveport, LA 71105 USA. License: CC BY 3.0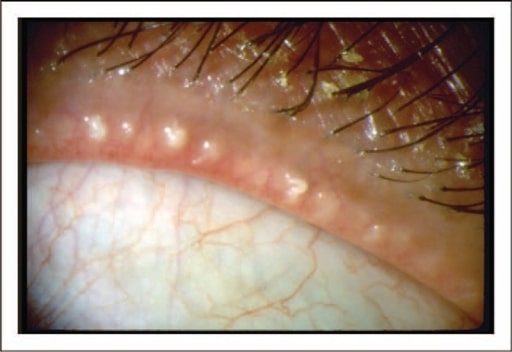
Image of a patient with posterior blepharitis/meibomian gland dysfunction: There is obstruction of the orifices of the meibomian glands with thick crusts around the eyelash follicles.
Image: “Dysfunctional tear syndrome” by American Academy of Ophthalmology. License: CC BY 4.0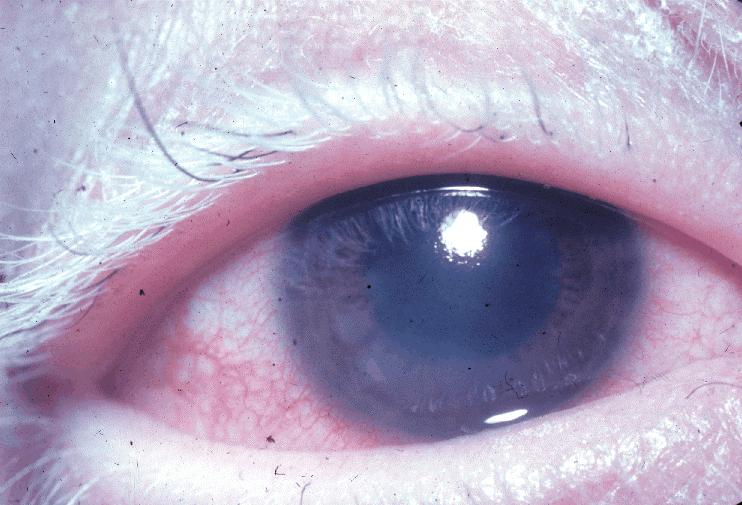
Whitening of eyelashes (poliosis)
Image: “Poliosis VKHS” by National Eye Institute. License: Public Domain