Molluscum contagiosum is a viral infection limited to the epidermis, typically without systemic manifestations. This infection is common in children below 5 years of age, though it can also be seen in healthy adolescents and adults, typically related to either contact sports or, with lesions on the genitals, as a sexually transmitted infection (STI). Lesions appear as grouped, flesh-colored, dome-shaped papules with central umbilication. Molluscum contagiosum is mild in immunocompetent patients and self resolves within months. Immunocompromised individuals present with extensive lesions, which require treatment. Molluscum contagiosum is highly transmissible; therefore, patient education is key in its management. Cryotherapy with liquid nitrogen is the 1st-line treatment.
Last updated: Mar 11, 2025
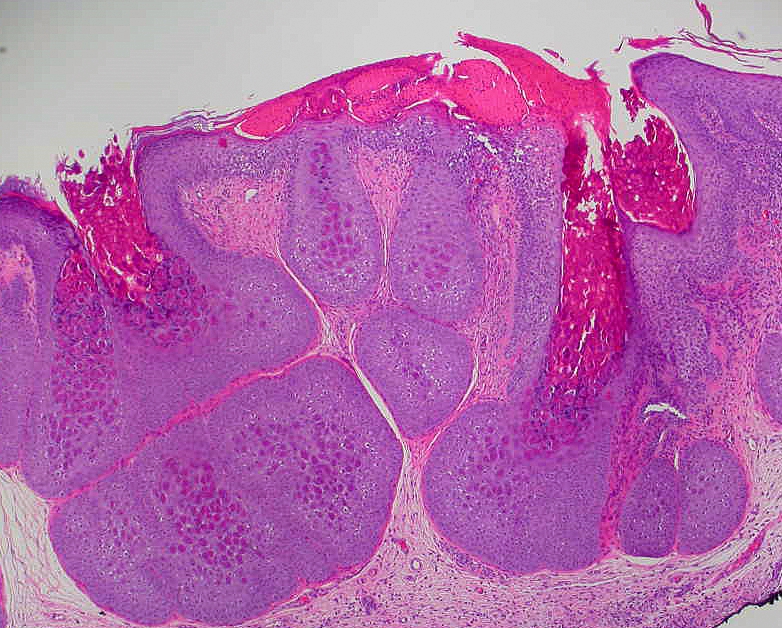
Henderson-Paterson bodies:
Characteristic histological features of molluscum contagiosum. Henderson-Paterson bodies are inclusions that are visible in the keratinocytes of the basal, spinous, and granular layers of the epidermis.

Dermatologic manifestation of molluscum contagiosum:
Flesh-colored pearly papules with central umbilication are present in the inguinal region, suggestive of molluscum contagiosum.

Multiple instances of molluscum contagiosum on the back of a child:
Flesh-colored pearly papules with central umbilication